Abstract
Purpose
Oxidative stress and mitochondrial dysfunction play central roles in reduced oocyte quality and infertility in obese patients. Mitochondria-targeted treatments containing co-enzyme Q10 such as mitoquinone (MitoQ) can increase mitochondrial antioxidative capacity; however, their safety and efficiency when supplemented to oocytes under lipotoxic conditions have not been described.
Methods
We tested the effect of different concentrations of MitoQ or its cationic carrier (TPP) (0, 0.1, 0.5, 1.0 μM each) during bovine oocyte IVM. Then, we tested the protective capacity of MitoQ (0.1 μM) against palmitic acid (PA)–induced lipotoxicity and mitochondrial dysfunction in oocytes.
Results
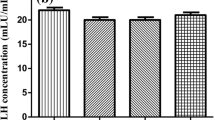
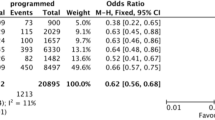
Exposure to MitoQ, or TPP only, at 1 μM significantly (P<0.05) reduced oocyte mitochondrial inner membrane potential (JC-1 staining) and resulted in reduced cleavage and blastocyst rates compared with solvent control. Lower concentrations of MitoQ or TPP had no effects on embryo development under control (PA-free) conditions. As expected, PA increased the levels of MMP and ROS in oocytes (CellROX staining) and reduced cleavage and blastocyst rates compared with the controls (P<0.05). These negative effects were ameliorated by 0.1 μM MitoQ. In contrast, 0.1 μM TPP alone had no protective effects. MitoQ also normalized the expression of HSP10 and TFAM, and partially normalized HSP60 in the produced blastocysts, indicating at least a partial alleviation of PA-induced mitochondrial stress.
Conclusion
Oocyte exposure to MitoQ may disturb mitochondrial bioenergetic functions and developmental capacity due to a TPP-induced cationic overload. A fine-tuned concentration of MitoQ can protect against lipotoxicity-induced mitochondrial stress during IVM and restore developmental competence and embryo quality.





Similar content being viewed by others
Data availability
Raw data files are available at Marei, Waleed (2023), “MitoQ during IVM”, Mendeley Data, V1, doi: 10.17632/htrsvbjfk5.1.
References
Adhikari D, Lee IW, Yuen WS, Carroll J. Oocyte mitochondria-key regulators of oocyte function and potential therapeutic targets for improving fertility. Biol Reprod. 2022;106:366–77. https://doi.org/10.1093/biolre/ioac024.
Wu LL, Norman RJ, Robker RL. The impact of obesity on oocytes: evidence for lipotoxicity mechanisms. Reprod Fertil Dev. 2011;24:29–34. https://doi.org/10.1071/RD11904.
Wang Q, Ratchford AM, Chi MM, Schoeller E, Frolova A, Schedl T, Moley KH. Maternal diabetes causes mitochondrial dysfunction and meiotic defects in murine oocytes. Mol Endocrinol. 2009;23:1603–12. https://doi.org/10.1210/me.2009-0033.
Wu LL, Russell DL, Wong SL, Chen M, Tsai TS, St John JC, Norman RJ, Febbraio MA, Carroll J, Robker RL. Mitochondrial dysfunction in oocytes of obese mothers: transmission to offspring and reversal by pharmacological endoplasmic reticulum stress inhibitors. Development. 2015;142:681–91. https://doi.org/10.1242/dev.114850.
Marei WFA, Smits A, Mohey-Elsaeed O, Pintelon I, Ginneberge D, Bols PEJ, Moerloose K, Leroy J. Differential effects of high fat diet-induced obesity on oocyte mitochondrial functions in inbred and outbred mice. Sci Rep. 2020;10:9806. https://doi.org/10.1038/s41598-020-66702-6.
Smits A, Marei WFA, Moorkens K, Bols PEJ, De Neubourg D, Leroy J. Obese outbred mice only partially benefit from diet normalization or calorie restriction as preconception care interventions to improve metabolic health and oocyte quality. Hum Reprod. 2022;37:2867–84. https://doi.org/10.1093/humrep/deac226.
Saben JL, Boudoures AL, Asghar Z, Thompson A, Drury A, Zhang W, Chi M, Cusumano A, Scheaffer S, Moley KH. Maternal metabolic syndrome programs mitochondrial dysfunction via germline changes across three generations. Cell Rep. 2016;16:1–8. https://doi.org/10.1016/j.celrep.2016.05.065.
Van Blerkom J. Mitochondrial function in the human oocyte and embryo and their role in developmental competence. Mitochondrion. 2011;11:797–813. https://doi.org/10.1016/j.mito.2010.09.012.
Thouas GA, Trounson AO, Wolvetang EJ, Jones GM. Mitochondrial dysfunction in mouse oocytes results in preimplantation embryo arrest in vitro. Biol Reprod. 2004;71:1936–42. https://doi.org/10.1095/biolreprod.104.033589.
Acton BM, Jurisicova A, Jurisica I, Casper RF. Alterations in mitochondrial membrane potential during preimplantation stages of mouse and human embryo development. Mol Hum Reprod. 2004;10:23–32. https://doi.org/10.1093/molehr/gah004.
Itami N, Shirasuna K, Kuwayama T, Iwata H. Palmitic acid induces ceramide accumulation, mitochondrial protein hyperacetylation, and mitochondrial dysfunction in porcine oocytes. Biol Reprod. 2018;98:644–53. https://doi.org/10.1093/biolre/ioy023.
Igosheva N, Abramov AY, Poston L, Eckert JJ, Fleming TP, Duchen MR, McConnell J. Maternal diet-induced obesity alters mitochondrial activity and redox status in mouse oocytes and zygotes. PLoS One. 2010;5:e10074. https://doi.org/10.1371/journal.pone.0010074.
Bournat JC, Brown CW. Mitochondrial dysfunction in obesity. Curr Opin Endocrinol Diabetes Obes. 2010;17:446–52. https://doi.org/10.1097/MED.0b013e32833c3026.
Mirabi P, Chaichi MJ, Esmaeilzadeh S, Ali Jorsaraei SG, Bijani A, Ehsani M, Hashemi Karooee SF. The role of fatty acids on ICSI outcomes: a prospective cohort study. Lipids Health Dis. 2017;16:18. https://doi.org/10.1186/s12944-016-0396-z.
Valckx SD, De Bie J, Michiels ED, Goovaerts IG, Punjabi U, Ramos-Ibeas P, Gutierrez-Adan A, Bols PE, Leroy JL. The effect of human follicular fluid on bovine oocyte developmental competence and embryo quality. Reprod Biomed Online. 2015;30:203–7. https://doi.org/10.1016/j.rbmo.2014.10.008.
Aardema H, Vos PL, Lolicato F, Roelen BA, Knijn HM, Vaandrager AB, Helms JB, Gadella BM. Oleic acid prevents detrimental effects of saturated fatty acids on bovine oocyte developmental competence. Biol Reprod. 2011;85:62–9. https://doi.org/10.1095/biolreprod.110.088815.
Van Hoeck V, Sturmey RG, Bermejo-Alvarez P, Rizos D, Gutierrez-Adan A, Leese HJ, Bols PE, Leroy JL. Elevated non-esterified fatty acid concentrations during bovine oocyte maturation compromise early embryo physiology. PLoS One. 2011;6:e23183. https://doi.org/10.1371/journal.pone.0023183.
Marei WFA, Van Raemdonck G, Baggerman G, Bols PEJ, Leroy J. Proteomic changes in oocytes after in vitro maturation in lipotoxic conditions are different from those in cumulus cells. Sci Rep. 2019;9:3673. https://doi.org/10.1038/s41598-019-40122-7.
Desmet KL, Van Hoeck V, Gagne D, Fournier E, Thakur A, O'Doherty AM, Walsh CP, Sirard MA, Bols PE, Leroy JL. Exposure of bovine oocytes and embryos to elevated non-esterified fatty acid concentrations: integration of epigenetic and transcriptomic signatures in resultant blastocysts. BMC Genomics. 2016;17:1004. https://doi.org/10.1186/s12864-016-3366-y.
Meulders B, Leroy JLMR, De Keersmaeker L, Bols PEJ, Marei WFA. Inhibition of mitochondrial ATP production during <i>in vitro</i> maturation of bovine oocytes alters DNA methylation patterns in mature oocytes and resulting embryos. Reprod Fertil Dev. 2023;35:125–6. https://doi.org/10.1071/RDv35n2Ab2.
Desmet KLJ, Marei WFA, Richard C, Sprangers K, Beemster GTS, Meysman P, Laukens K, Declerck K, Vanden Berghe W, Bols PEJ, Hue I, Leroy J. Oocyte maturation under lipotoxic conditions induces carryover transcriptomic and functional alterations during post-hatching development of good-quality blastocysts: novel insights from a bovine embryo-transfer model. Hum Reprod. 2020;35:293–307. https://doi.org/10.1093/humrep/dez248.
Bruna de Lima C, Cristina Dos Santos E, Sirard MA. DOHaD: A menagerie of adaptations and perspectives: the interplay between early embryo metabolism and mitoepigenetic programming of development. Reproduction. 2023;166:F15–26. https://doi.org/10.1530/REP-22-0424.
Marei WFA, Leroy J. Cellular stress responses in oocytes: molecular changes and clinical implications. Adv Exp Med Biol. 2022;1387:171–89. https://doi.org/10.1007/5584_2021_690.
Marei WFA, Van den Bosch L, Pintelon I, Mohey-Elsaeed O, Bols PEJ, Leroy J. Mitochondria-targeted therapy rescues development and quality of embryos derived from oocytes matured under oxidative stress conditions: a bovine in vitro model. Hum Reprod. 2019;34:1984–98. https://doi.org/10.1093/humrep/dez161.
Kim J, Seli E. Mitochondria as a biomarker for IVF outcome. Reproduction. 2019;157:R235–42. https://doi.org/10.1530/REP-18-0580.
Hu X-Q, Zhang L. Hypoxia and mitochondrial dysfunction in pregnancy complications. Antioxidants. 2021;10:405.
Smith AN, Wang X, Thomas DG, Tatum RE, Booz GW, Cunningham MW Jr. The role of mitochondrial dysfunction in preeclampsia: causative factor or collateral damage? Am J Hypertens. 2021;34:442–52. https://doi.org/10.1093/ajh/hpab003.
Gupta S, Agarwal A, Banerjee J, Alvarez JG. The role of oxidative stress in spontaneous abortion and recurrent pregnancy loss: a systematic review. Obstet Gynecol Surv. 2007;62:335–47. https://doi.org/10.1097/01.ogx.0000261644.89300.df.
Miles MV, Horn PS, Tang PH, Morrison JA, Miles L, DeGrauw T, Pesce AJ. Age-related changes in plasma coenzyme Q10 concentrations and redox state in apparently healthy children and adults. Clin Chim Acta. 2004;347:139–44. https://doi.org/10.1016/j.cccn.2004.04.003.
Turi A, Giannubilo SR, Bruge F, Principi F, Battistoni S, Santoni F, Tranquilli AL, Littarru G, Tiano L. Coenzyme Q10 content in follicular fluid and its relationship with oocyte fertilization and embryo grading. Arch Gynecol Obstet. 2012;285:1173–6. https://doi.org/10.1007/s00404-011-2169-2.
Akarsu S, Gode F, Isik AZ, Dikmen ZG, Tekindal MA. The association between coenzyme Q10 concentrations in follicular fluid with embryo morphokinetics and pregnancy rate in assisted reproductive techniques. J Assist Reprod Genet. 2017;34:599–605. https://doi.org/10.1007/s10815-017-0882-x.
Ballesteros-Guzman AK, Carrasco-Legleu CE, Levario-Carrillo M, Chavez-Corral DV, Sanchez-Ramirez B, Marinelarena-Carrillo EO, Guerrero-Salgado F, Reza-Lopez SA. Prepregnancy obesity, maternal dietary intake, and oxidative stress biomarkers in the fetomaternal unit. Biomed Res Int. 2019;2019:5070453. https://doi.org/10.1155/2019/5070453.
Deichmann R, Lavie C, Andrews S. Coenzyme q10 and statin-induced mitochondrial dysfunction. Ochsner J. 2010;10:16–21.
Turunen M, Appelkvist EL, Sindelar P, Dallner G. Blood concentration of coenzyme Q(10) increases in rats when esterified forms are administered. J Nutr. 1999;129:2113–8. https://doi.org/10.1093/jn/129.12.2113.
Kyei G, Sobhani A, Nekonam S, Shabani M, Ebrahimi F, Qasemi M, Salahi E, Fardin A. Assessing the effect of MitoQ(10) and Vitamin D3 on ovarian oxidative stress, steroidogenesis and histomorphology in DHEA induced PCOS mouse model. Heliyon. 2020;6:e04279. https://doi.org/10.1016/j.heliyon.2020.e04279.
Gong X, Li H, Zhao Y. The improvement and clinical application of human oocyte in vitro maturation (IVM). Reprod Sci. 2022;29:2127–35. https://doi.org/10.1007/s43032-021-00613-3.
Smitz JE, Thompson JG, Gilchrist RB. The promise of in vitro maturation in assisted reproduction and fertility preservation. Semin Reprod Med. 2011;29:24–37. https://doi.org/10.1055/s-0030-1268701.
Sun B, Ma Y, Li L, Hu L, Wang F, Zhang Y, Dai S, Sun Y. Factors associated with ovarian hyperstimulation syndrome (OHSS) severity in women with polycystic ovary syndrome undergoing IVF/ICSI. Front Endocrinol (Lausanne). 2020;11:615957. https://doi.org/10.3389/fendo.2020.615957.
Agarwal A, Said TM, Bedaiwy MA, Banerjee J, Alvarez JG. Oxidative stress in an assisted reproductive techniques setting. Fertil Steril. 2006;86:503–12. https://doi.org/10.1016/j.fertnstert.2006.02.088.
Budani MC, Tiboni GM. Effects of supplementation with natural antioxidants on oocytes and preimplantation embryos. Antioxidants (Basel). 2020;9 https://doi.org/10.3390/antiox9070612.
De Bie J, Smits A, Marei WFA, Leroy J. Capacity of Trolox to improve the development and quality of metabolically compromised bovine oocytes and embryos invitro during different windows of development. Reprod Fertil Dev. 2021;33:291–304. https://doi.org/10.1071/RD20194.
Reily C, Mitchell T, Chacko BK, Benavides G, Murphy MP, Darley-Usmar V. Mitochondrially targeted compounds and their impact on cellular bioenergetics. Redox Biol. 2013;1:86–93. https://doi.org/10.1016/j.redox.2012.11.009.
Valckx SD, Arias-Alvarez M, De Pauw I, Fievez V, Vlaeminck B, Fransen E, Bols PE, Leroy JL. Fatty acid composition of the follicular fluid of normal weight, overweight and obese women undergoing assisted reproductive treatment: a descriptive cross-sectional study. Reprod Biol Endocrinol. 2014;12:13. https://doi.org/10.1186/1477-7827-12-13.
Leroy JL, Vanholder T, Mateusen B, Christophe A, Opsomer G, de Kruif A, Genicot G, Van Soom A. Non-esterified fatty acids in follicular fluid of dairy cows and their effect on developmental capacity of bovine oocytes in vitro. Reproduction. 2005;130:485–95. https://doi.org/10.1530/rep.1.00735.
Marei WFA, De Bie J, Mohey-Elsaeed O, Wydooghe E, Bols PEJ, Leroy J. Alpha-linolenic acid protects the developmental capacity of bovine cumulus-oocyte complexes matured under lipotoxic conditions in vitro. Biol Reprod. 2017;96:1181–96. https://doi.org/10.1093/biolre/iox046.
De Biasi S, Gibellini L, Cossarizza A. Uncompensated polychromatic analysis of mitochondrial membrane potential using JC-1 and Multilaser Excitation. Curr Protoc Cytom. 2015;72 https://doi.org/10.1002/0471142956.cy0732s72.
Komatsu K, Iwase A, Mawatari M, Wang J, Yamashita M, Kikkawa F. Mitochondrial membrane potential in 2-cell stage embryos correlates with the success of preimplantation development. Reproduction. 2014;147:627–38. https://doi.org/10.1530/REP-13-0288.
Pfaffl MW. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 2001;29:e45. https://doi.org/10.1093/nar/29.9.e45.
Bhatti JS, Kumar S, Vijayan M, Bhatti GK, Reddy PH. Therapeutic strategies for mitochondrial dysfunction and oxidative stress in age-related metabolic disorders. Prog Mol Biol Transl Sci. 2017;146:13–46. https://doi.org/10.1016/bs.pmbts.2016.12.012.
Cocheme HM, Kelso GF, James AM, Ross MF, Trnka J, Mahendiran T, Asin-Cayuela J, Blaikie FH, Manas AR, Porteous CM, Adlam VJ, Smith RA, et al. Mitochondrial targeting of quinones: therapeutic implications. Mitochondrion. 2007;7(Suppl):S94–102. https://doi.org/10.1016/j.mito.2007.02.007.
Pala L, Senn HM, Caldwell ST, Prime TA, Warrington S, Bright TP, Prag HA, Wilson C, Murphy MP, Hartley RC. Enhancing the mitochondrial uptake of phosphonium cations by carboxylic acid incorporation. Frontiers. Chemistry. 2020:8. https://doi.org/10.3389/fchem.2020.00783.
Austin S, Nowikovsky K. Mitochondrial osmoregulation in evolution, cation transport and metabolism. Biochim Biophys Acta Bioenerg. 2021;1862:148368. https://doi.org/10.1016/j.bbabio.2021.148368.
Strubbe-Rivera JO, Schrad JR, Pavlov EV, Conway JF, Parent KN, Bazil JN. The mitochondrial permeability transition phenomenon elucidated by cryo-EM reveals the genuine impact of calcium overload on mitochondrial structure and function. Sci Rep. 2021;11:1037. https://doi.org/10.1038/s41598-020-80398-8.
Liu M. The biology and dynamics of mammalian cortical granules. Reprod Biol Endocrinol. 2011;9:149. https://doi.org/10.1186/1477-7827-9-149.
Leo S, Szabadkai G, Rizzuto R. The mitochondrial antioxidants MitoE(2) and MitoQ(10) increase mitochondrial Ca(2+) load upon cell stimulation by inhibiting Ca(2+) efflux from the organelle. Ann N Y Acad Sci. 2008;1147:264–74. https://doi.org/10.1196/annals.1427.019.
Sugimura S, Matoba S, Hashiyada Y, Aikawa Y, Ohtake M, Matsuda H, Kobayashi S, Konishi K, Imai K. Oxidative phosphorylation-linked respiration in individual bovine oocytes. J Reprod Dev. 2012;58:636–41. https://doi.org/10.1262/jrd.2012-082.
Krisher RL, Prather RS. A role for the Warburg effect in preimplantation embryo development: metabolic modification to support rapid cell proliferation. Mol Reprod Dev. 2012;79:311–20. https://doi.org/10.1002/mrd.22037.
Wei YH, Lu CY, Wei CY, Ma YS, Lee HC. Oxidative stress in human aging and mitochondrial disease-consequences of defective mitochondrial respiration and impaired antioxidant enzyme system. Chin J Phys. 2001;44:1–11.
Kelso GF, Porteous CM, Hughes G, Ledgerwood EC, Gane AM, Smith RA, Murphy MP. Prevention of mitochondrial oxidative damage using targeted antioxidants. Ann N Y Acad Sci. 2002;959:263–74. https://doi.org/10.1111/j.1749-6632.2002.tb02098.x.
Tatemoto H, Ootaki K, Shigeta K, Muto N. Enhancement of developmental competence after in vitro fertilization of porcine oocytes by treatment with ascorbic acid 2-O-alpha-glucoside during in vitro maturation. Biol Reprod. 2001;65:1800–6. https://doi.org/10.1095/biolreprod65.6.1800.
Takami M, Preston SL, Toyloy VA, Behrman HR. Antioxidants reversibly inhibit the spontaneous resumption of meiosis. Am J Phys. 1999;276:E684–8. https://doi.org/10.1152/ajpendo.1999.276.4.E684.
Ruder EH, Hartman TJ, Blumberg J, Goldman MB. Oxidative stress and antioxidants: exposure and impact on female fertility. Hum Reprod Update. 2008;14:345–57. https://doi.org/10.1093/humupd/dmn011.
Valckx SD, Van Hoeck V, Arias-Alvarez M, Maillo V, Lopez-Cardona AP, Gutierrez-Adan A, Berth M, Cortvrindt R, Bols PE, Leroy JL. Elevated non-esterified fatty acid concentrations during in vitro murine follicle growth alter follicular physiology and reduce oocyte developmental competence. Fertil Steril. 2014;102:1769–76. https://doi.org/10.1016/j.fertnstert.2014.08.018.
Iossa S, Mollica MP, Lionetti L, Crescenzo R, Botta M, Liverini G. Skeletal muscle oxidative capacity in rats fed high-fat diet. Int J Obes Relat Metab Disord. 2002;26:65–72. https://doi.org/10.1038/sj.ijo.0801844.
Smits A, Marei WFA, De Neubourg D, Leroy J. Diet normalization or caloric restriction as a preconception care strategy to improve metabolic health and oocyte quality in obese outbred mice. Reprod Biol Endocrinol. 2021;19(166) https://doi.org/10.1186/s12958-021-00848-4.
Yang HW, Hwang KJ, Kwon HC, Kim HS, Choi KW, Oh KS. Detection of reactive oxygen species (ROS) and apoptosis in human fragmented embryos. Hum Reprod. 1998;13:998–1002. https://doi.org/10.1093/humrep/13.4.998.
Al-Zubaidi U, Adhikari D, Cinar O, Zhang QH, Yuen WS, Murphy MP, Rombauts L, Robker RL, Carroll J. Mitochondria-targeted therapeutics, MitoQ and BGP-15, reverse aging-associated meiotic spindle defects in mouse and human oocytes. Hum Reprod. 2021;36:771–84. https://doi.org/10.1093/humrep/deaa300.
Hu F, Liu F. Mitochondrial stress: a bridge between mitochondrial dysfunction and metabolic diseases? Cell Signal. 2011;23:1528–33. https://doi.org/10.1016/j.cellsig.2011.05.008.
Kang SG, Dimitrova MN, Ortega J, Ginsburg A, Maurizi MR. Human mitochondrial ClpP is a stable heptamer that assembles into a tetradecamer in the presence of ClpX. J Biol Chem. 2005;280:35424–32. https://doi.org/10.1074/jbc.M507240200.
Antelman J, Manandhar G, Yi YJ, Li R, Whitworth KM, Sutovsky M, Agca C, Prather RS, Sutovsky P. Expression of mitochondrial transcription factor A (TFAM) during porcine gametogenesis and preimplantation embryo development. J Cell Physiol. 2008;217:529–43. https://doi.org/10.1002/jcp.21528.
Campbell BK, Souza C, Gong J, Webb R, Kendall N, Marsters P, Robinson G, Mitchell A, Telfer EE, Baird DT. Domestic ruminants as models for the elucidation of the mechanisms controlling ovarian follicle development in humans. Reprod Suppl. 2003;61:429–43.
Santos RR, Schoevers EJ, Roelen BA. Usefulness of bovine and porcine IVM/IVF models for reproductive toxicology. Reprod Biol Endocrinol. 2014;12:117. https://doi.org/10.1186/1477-7827-12-117.
Acknowledgements
The authors would like to acknowledge ACAM, the microscopy core facility of the University of Antwerp, for the use of their microscopy facilities. The Leica SP8 microscope used in this publication was funded by a Medium-scale research infrastructure grant (GOH4216N) of the FWO.
Author information
Authors and Affiliations
Contributions
WFAM contributed with the main project idea, conducted the experiments, analyzed the data, and wrote the manuscript. O.M-E performed the confocal microscopy and image analysis. IP helped with the optimization of microscopy and image data analysis. J.L.M.R supervised the project and critically read and edited the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marei, W.F., Mohey-Elsaeed, O., Pintelon, I. et al. Risks of using mitoquinone during in vitro maturation and its potential protective effects against lipotoxicity-induced oocyte mitochondrial stress. J Assist Reprod Genet 41, 371–383 (2024). https://doi.org/10.1007/s10815-023-02994-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02994-7