Abstract
Purpose
Does existing scientific literature suggest an impact of oocyte dysmorphisms on biological or clinical outcomes of assisted reproduction treatments?
Methods
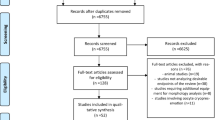
Studies of interest were selected from an initial cohort of 6651 potentially relevant records retrieved. PubMed was systematically searched for peer-reviewed original papers and reviews identified by keywords and medical subject heading (MeSH) terms. The most relevant publications were critically evaluated to identify criteria for oocyte morphological evaluation and IVF outcomes. For each morphological abnormality, we generated an oocyte literature score (OLS) through the following procedure: (a) papers showing a negative, absence of, or positive correlation between a given abnormality and IVF outcome were scored 1, 0, and − 1, respectively; (b) the sum of these scores was expressed as a fraction of all analyzed papers; (c) the obtained fraction was multiplied by 10 and converted into decimal number.
Result
We identified eleven different dysmorphisms, of which six were extracytoplasmic (COC, zona pellucida, perivitelline space, polar body 1, shape, giant size) and five intracytoplasmic (vacuoles, refractile bodies, SER clusters, granularity, color). Among the extracytoplasmic dysmorphisms, abnormal morphology of the COC generated an OLS of 8.33, indicating a large prevalence (5/6) of studies associated with a negative outcome. Three intracytoplasmic dysmorphisms (vacuoles, SER clusters, and granularity) produced OLS of 7.14, 7.78, and 6.25, respectively, suggestive of a majority of studies reporting a negative outcome.
Conclusion
COC morphology, vacuoles, SER clusters, and granularity produced OLS suggestive of a prevalence of studies reporting a negative outcome.


Similar content being viewed by others
References
Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting. Hum Reprod. 2011;26(6):1270–83.
Balaban B, Urman B, Sertac A, Alatas C, Aksoy S, Mercan R. Oocyte morphology does not affect fertilization rate, embryo quality and implantation rate after intracytoplasmic sperm injection. Hum Reprod. 1998;13(12):3431–3.
Dal Canto M, Guglielmo MC, Mignini Renzini M, Fadini R, Moutier C, Merola M, et al. Dysmorphic patterns are associated with cytoskeletal alterations in human oocytes. Hum Reprod. 2017;32(4):750–7.
Ebner T, Moser M, Shebl O, Sommerguber M, Tews G. Prognosis of oocytes showing aggregation of smooth endoplasmic reticulum. Reprod Biomed Online. 2008;16(1):113–8.
Rienzi L, Ubaldi FM, Iacobelli M, Minasi MG, Romano S, Ferrero S, et al. Significance of metaphase II human oocyte morphology on ICSI outcome. Fertil Steril. 2008;90(5):1692–700.
De Sutter P, Dozortsev D, Qian C, Dhont M. Oocyte morphology does not correlate with fertilization rate and embryo quality after intracytoplasmic sperm injection. Hum Reprod. 1996;11(3):595–7.
Ten J, Mendiola J, Vioque J, de Juan J, Bernabeu R. Donor oocyte dysmorphisms and their influence on fertilization and embryo quality. Reprod Biomed Online. 2007;14(1):40–8.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Akarsu C, Çağlar G, Vicdan K, Sözen E, Biberoğlu K. Smooth endoplasmic reticulum aggregations in all retrieved oocytes causing recurrent multiple anomalies: case report. Fertil Steril. 2009;92(4):1496.e1-1496.e3.
Alikani M, Palermo G, Adler A, Bertoli M, Blake M, Cohen J. Intracytoplasmic sperm injection in dysmorphic human oocytes. Zygote. 1995;3(4):283–8.
Ashrafi M, Karimian L, Eftekhari-Yazdi P, Hasani F, Arabipoor A, Bahmanabadi A, et al. Effect of oocyte dysmorphisms on intracytoplasmic sperm injection cycle outcomes in normal ovarian responders. J Obstet Gynaecol Res. 2015;41(12):1912–20.
Balaban B, Urman B. Effect of oocyte morphology on embryo development and implantation. Reprod Biomed Online. 2006;12(5):608–15.
Balaban B, Ata B, Isiklar A, Yakin K, Urman B. Severe cytoplasmic abnormalities of the oocyte decrease cryosurvival and subsequent embryonic development of cryopreserved embryos. Hum Reprod. 2008;23(8):1778–85.
Balakier H, Bouman D, Sojecki A, Librach C, Squire JA. Morphological and cytogenetic analysis of human giant oocytes and giant embryos. Hum Reprod. 2002;17(9):2394–401.
Bassil R, Casper RF, Meriano J, Smith R, Haas J, Mehta C, et al. Can oocyte diameter predict embryo quality? Reprod Sci. 2021;28(3):904–8.
Bertrand E, Van den Bergh M, Englert Y. Does zona pellucida thickness influence the fertilization rate? Hum Reprod. 1995;10(5):1189–93.
Braga DPAF, Setti AS, de Figueira RCS, Machado RB, Laconelli A, Borges E. Influence of oocyte dysmorphisms on blastocyst formation and quality. Fertil Steril. 2013;100(3):748–54.
Chamayou S, Ragolia C, Alecci C, Storaci G, Maglia E, Russo E, et al. Meiotic spindle presence and oocyte morphology do not predict clinical ICSI outcomes: a study of 967 transferred embryos. Reprod Biomed Online. 2006;13(5):661–7.
Ciotti PM, Notarangelo L, Morselli-Labate AM, Felletti V, Porcu E, Venturoli S. First polar body morphology before ICSI is not related to embryo quality or pregnancy rate. Hum Reprod. 2004;19(10):2334–9.
Dal Canto M, Brambillasca F, Mignini Renzini M, Coticchio G, Merola M, Lain M, et al. Cumulus cell-oocyte complexes retrieved from antral follicles in IVM cycles: relationship between COCs morphology, gonadotropin priming and clinical outcome. J Assist Reprod Genet. 2012;29(6):513–9.
Daya S, Kohut J, Gunby J, Younglai E. Influence of blood clots in the cumulus complex on oocyte fertilization and cleavage. Hum Reprod. 1990;5(6):744–6.
de Cássia Figueira RS, de Almeida Ferreira Braga DP, Semião-Francisco L, Madaschi C, Iaconelli A, Borges E. Metaphase II human oocyte morphology: contributing factors and effects on fertilization potential and embryo developmental ability in ICSI cycles. Fertil Steril. 2010;94(3):1115–7.
De Santis L, Cino I, Rabellotti E, Calzi F, Persico P, Borini A, et al. Polar body morphology and spindle imaging as predictors of oocyte quality. Reprod Biomed Online. 2005;11(1):36–42.
Ebner T, Yaman C, Moser M, Sommergruber M, Feichtinger O, Tews G. Prognostic value of first polar body morphology on fertilization rate and embryo quality in intracytoplasmic sperm injection. Hum Reprod. 2000;15(2):427–30.
Ebner T, Moser M, Sommergruber M, Gaiswinkler U, Shebl O, Jesacher K, et al. Occurrence and developmental consequences of vacuoles throughout preimplantation development. Fertil Steril. 2005;83(6):1635–40.
Ebner T, Moser M, Tews G. Is oocyte morphology prognostic of embryo developmental potential after ICSI? Reprod Biomed Online. 2006;12(4):507–12.
Ebner T, Moser M, Shebl O, Sommergruber M, Yaman C, Tews G. Blood clots in the cumulus-oocyte complex predict poor oocyte quality and post-fertilization development. Reprod Biomed Online. 2008;16(6):801–7.
Ebner T, Shebl O, Moser M, Sommergruber M, Tews G. Developmental fate of ovoid oocytes. Hum Reprod. 2008;23(1):62–6.
Esfandiari N, Burjaq H, Gotlieb L, Casper RF. Brown oocytes: implications for assisted reproductive technology. Fertil Steril. 2006;86(5):1522–5.
Fancsovits P, Tóthné ZG, Murber A, Takács FZ, Papp Z, Urbancsek J. Correlation between first polar body morphology and further embryo development. Acta Biol Hung. 2006;57(3):331–8.
Fancsovits P, Tóthné ZG, Murber Á, Rigó J, Urbancsek J. Importance of cytoplasmic granularity of human oocytes in in vitro fertilization treatments. Acta Biol Hung. 2012;63(2):189–201.
Faramarzi A, Khalili MA, Agha-Rahimi A, Omidi M. Is there any correlation between oocyte polarization microscopy findings with embryo time lapse monitoring in ICSI program? Arch Gynecol Obstet. 2017;295(6):1515–22.
Faramarzi A, Khalili MA, Omidi M. Morphometric analysis of human oocytes using time lapse: does it predict embryo developmental outcomes? Hum Fertil (Camb). 2019;22(3):171–6.
Farhi J, Nahum H, Weissman A, Zahalka N, Glezerman M, Levran D. Coarse granulation in the perivitelline space and IVF-ICSI outcome. J Assist Reprod Genet. 2002;19(12):545–9.
Ferreux L, Sallem A, Chargui A, Gille A-S, Bourdon M, Maignien C, et al. Is it time to reconsider how to manage oocytes affected by smooth endoplasmic reticulum aggregates? Hum Reprod. 2019;34(4):591–600.
González-Ortega C, Cancino-Villarreal P, Alonzo-Torres VE, Martínez-Robles I, Pérez-Peña E, Gutiérrez-Gutiérrez AM. Polarized light microscopy for evaluation of oocytes as a prognostic factor in the evolution of a cycle in assisted reproduction. Ginecol Obstet Mex. 2016;84(4):217–27.
Hassa H, Aydın Y, Taplamacıoğlu F. The role of perivitelline space abnormalities of oocytes in the developmental potential of embryos. J Turk Ger Gynecol Assoc. 2014;15(3):161–3.
Hassan-Ali H, Hisham-Saleh A, El-Gezeiry D, Baghdady I, Ismaeil I, Mandelbaum J. Perivitelline space granularity: a sign of human menopausal gonadotrophin overdose in intracytoplasmic sperm injection. Hum Reprod. 1998;13(12):3425–30.
Hattori H, Nakamura Y, Nakajo Y, Araki Y, Kyono K. Deliveries of babies with normal health derived from oocytes with smooth endoplasmic reticulum clusters. J Assist Reprod Genet. 2014;31(11):1461–7.
Høst E, Gabrielsen A, Lindenberg S, Smidt-Jensen S. Apoptosis in human cumulus cells in relation to zona pellucida thickness variation, maturation stage, and cleavage of the corresponding oocyte after intracytoplasmic sperm injection. Fertil Steril. 2002;77(3):511–5.
Kahraman S, Yakin K, Dönmez E, Samli H, Bahçe M, Cengiz G, et al. Relationship between granular cytoplasm of oocytes and pregnancy outcome following intracytoplasmic sperm injection. Hum Reprod. 2000;15(11):2390–3.
La Sala GB, Nicoli A, Villani MT, Di Girolamo R, Capodanno F, Blickstein I. The effect of selecting oocytes for insemination and transferring all resultant embryos without selection on outcomes of assisted reproduction. Fertil Steril. 2009;91(1):96–100.
Lehner A, Kaszas Z, Murber A, Rigo J, Urbancsek J, Fancsovits P. Giant oocytes in human in vitro fertilization treatments. Arch Gynecol Obstet. 2015;292(3):697–703.
Lin Y-C, Chang S-Y, Lan K-C, Huang H-W, Chang C-Y, Tsai M-Y, et al. Human oocyte maturity in vivo determines the outcome of blastocyst development in vitro. J Assist Reprod Genet. 2003;20(12):506–12.
Loutradis D, Drakakis P, Kallianidis K, Milingos S, Dendrinos S, Michalas S. Oocyte morphology correlates with embryo quality and pregnancy rate after intracytoplasmic sperm injection. Fertil Steril. 1999;72(2):240–4.
Machtinger R, Politch JA, Hornstein MD, Ginsburg ES, Racowsky C. A giant oocyte in a cohort of retrieved oocytes: does it have any effect on the in vitro fertilization cycle outcome? Fertil Steril. 2011;95(2):573–6.
Madaschi C, Aoki T, de Almeida Ferreira Braga DP, de Cássia Sávio Figueira R, Semião Francisco L, Iaconelli A, et al. Zona pellucida birefringence score and meiotic spindle visualization in relation to embryo development and ICSI outcomes. Reprod Biomed Online. 2009;18(5):681–6.
Mateizel I, Van Landuyt L, Tournaye H, Verheyen G. Deliveries of normal healthy babies from embryos originating from oocytes showing the presence of smooth endoplasmic reticulum aggregates. Hum Reprod. 2013;28(8):2111–7.
Meriano JS, Alexis J, Visram-Zaver S, Cruz M, Casper RF. Tracking of oocyte dysmorphisms for ICSI patients may prove relevant to the outcome in subsequent patient cycles. Hum Reprod. 2001;16(10):2118–23.
Montag M, Schimming T, Köster M, Zhou C, Dorn C, Rösing B, et al. Oocyte zona birefringence intensity is associated with embryonic implantation potential in ICSI cycles. Reprod Biomed Online. 2008;16(2):239–44.
Navarro PA, de Araújo MM, de Araújo CM, Rocha M, dos Reis R, Martins W. Relationship between first polar body morphology before intracytoplasmic sperm injection and fertilization rate, cleavage rate, and embryo quality. Int J Gynaecol Obstet. 2009;104(3):226–9.
Ng ST, Chang TH, Wu TC. Prediction of the rates of fertilization, cleavage, and pregnancy success by cumulus-coronal morphology in an in vitro fertilization program. Fertil Steril. 1999;72(3):412–7.
Otsuki J, Okada A, Morimoto K, Nagai Y, Kubo H. The relationship between pregnancy outcome and smooth endoplasmic reticulum clusters in MII human oocytes. Hum Reprod. 2004;19(7):1591–7.
Otsuki J, Nagai Y, Chiba K. Lipofuscin bodies in human oocytes as an indicator of oocyte quality. J Assist Reprod Genet. 2007;24(7):263–70.
Rama Raju GA, Prakash GJ, Krishna KM, Madan K. Meiotic spindle and zona pellucida characteristics as predictors of embryonic development: a preliminary study using PolScope imaging. Reprod Biomed Online. 2007;14(2):166–74.
Rattanachaiyanont M. Lack of correlation between oocyte- corona-cumulus complex morphology and nuclear maturity of oocytes collected in stimulated cycles for intracytoplasmic sperm injection. Fertil Steril. 1999;71(5):937–40.
Rosenbusch B, Schneider M, Gläser B, Brucker C. Cytogenetic analysis of giant oocytes and zygotes to assess their relevance for the development of digynic triploidy. Hum Reprod. 2002;17(9):2388–93.
Sá R, Cunha M, Silva J, Luís A, Oliveira C, Teixeira da Silva J, et al. Ultrastructure of tubular smooth endoplasmic reticulum aggregates in human metaphase II oocytes and clinical implications. Fertil Steril. 2011;96(1):143-149.e7.
Sauerbrun-Cutler M-T, Vega M, Breborowicz A, Gonzales E, Stein D, Lederman M, et al. Oocyte zona pellucida dysmorphology is associated with diminished in-vitro fertilization success. J Ovarian Res. 2015;27(8):5.
Serhal PF, Ranieri DM, Kinis A, Marchant S, Davies M, Khadum IM. Oocyte morphology predicts outcome of intracytoplasmic sperm injection. Hum Reprod. 1997;12(6):1267–70.
Setti AS, Figueira RCS, Braga DPAF, Colturato SS, Iaconelli A, Borges E. Relationship between oocyte abnormal morphology and intracytoplasmic sperm injection outcomes: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2011;159(2):364–70.
Setti AS, Figueira RCS, de Almeida Ferreira Braga DP, de Azevedo MC, Iaconelli A, Borges E. Oocytes with smooth endoplasmic reticulum clusters originate blastocysts with impaired implantation potential. Fertil Steril. 2016;106(7):1718–24.
Shaw-Jackson C, Thomas A-L, Van Beirs N, Ameye L, Colin J, Bertrand E, et al. Oocytes affected by smooth endoplasmic reticulum aggregates: to discard or not to discard? Arch Gynecol Obstet. 2016;294(1):175–84.
Shen Y, Stalf T, Mehnert C, Eichenlaub-Ritter U, Tinneberg HR. High magnitude of light retardation by the zona pellucida is associated with conception cycles. Hum Reprod. 2005;20(6):1596–606.
Shi W, Xu B, Wu L-M, Jin R-T, Luan H-B, Luo L-H, et al. Oocytes with a dark zona pellucida demonstrate lower fertilization, implantation and clinical pregnancy rates in IVF/ICSI cycles. PLoS ONE. 2014;9(2):e89409.
Sousa M, Teixeira da Silva J, Silva J, Cunha M, Viana P, Oliveira E, et al. Embryological, clinical and ultrastructural study of human oocytes presenting indented zona pellucida. Zygote. 2015;23(1):145–57.
Sousa M, Cunha M, Silva J, Oliveira E, Pinho MJ, Almeida C, et al. Ultrastructural and cytogenetic analyses of mature human oocyte dysmorphisms with respect to clinical outcomes. J Assist Reprod Genet. 2016;33(8):1041–57.
Tabibnejad N, Soleimani M, Aflatoonian A. Zona pellucida birefringence and meiotic spindle visualization are not related to the time-lapse detected embryo morphokinetics in women with polycystic ovarian syndrome. Eur J Obstet Gynecol Reprod Biol. 2018;230:96–102.
Takahashi H, Otsuki J, Yamamoto M, Saito H, Hirata R, Habara T, et al. Clinical outcomes of MII oocytes with refractile bodies in patients undergoing ICSI and single frozen embryo transfer. Reprod Med Biol. 2020;19(1):75–81.
Verlinsky Y, Lerner S, Illkevitch N, Kuznetsov V, Kuznetsov I, Cieslak J, et al. Is there any predictive value of first polar body morphology for embryo genotype or developmental potential? Reprod Biomed Online. 2003;7(3):336–41.
Wallbutton S, Kasraie J. Vacuolated oocytes: fertilization and embryonic arrest following intra-cytoplasmic sperm injection in a patient exhibiting persistent oocyte macro vacuolization–case report. J Assist Reprod Genet. 2010;27(4):183–8.
Weghofer A, Kushnir VA, Darmon SK, Jafri H, Lazzaroni-Tealdi E, Zhang L, et al. Age, body weight and ovarian function affect oocyte size and morphology in non-PCOS patients undergoing intracytoplasmic sperm injection (ICSI). PLoS ONE. 2019;14(10):e0222390.
Wilding M, Di Matteo L, D’Andretti S, Montanaro N, Capobianco C, Dale B. An oocyte score for use in assisted reproduction. J Assist Reprod Genet. 2007;24(8):350–8.
Xia P. Intracytoplasmic sperm injection: correlation of oocyte grade based on polar body, perivitelline space and cytoplasmic inclusions with fertilization rate and embryo quality. Hum Reprod. 1997;12(8):1750–5.
Yakin K, Balaban B, Isiklar A, Urman B. Oocyte dysmorphism is not associated with aneuploidy in the developing embryo. Fertil Steril. 2007;88(4):811–6.
Yi X-F, Xi H-L, Zhang S-L, Yang J. Relationship between the positions of cytoplasmic granulation and the oocytes developmental potential in human. Sci Rep. 2019;9(1):7215.
Zhou W, Fu L, Sha W, Chu D, Li Y. Relationship of polar bodies morphology to embryo quality and pregnancy outcome. Zygote. 2016;24(3):401–7.
Richani D, Dunning KR, Thompson JG, Gilchrist RB. Metabolic co-dependence of the oocyte and cumulus cells: essential role in determining oocyte developmental competence. Hum Reprod Update. 2021;27(1):27–47.
Attaran M, Pasqualotto E, Falcone T, Goldberg JM, Miller KF, Agarwal A, et al. The effect of follicular fluid reactive oxygen species on the outcome of in vitro fertilization. Int J Fertil Womens Med. 2000;45(5):314–20.
Ebner T, Balaban B, Moser M, Shebl O, Urman B, Ata B, et al. Automatic user-independent zona pellucida imaging at the oocyte stage allows for the prediction of preimplantation development. Fertil Steril. 2010;94(3):913–20.
Ubaldi F, Rienzi L. Morphological selection of gametes. Placenta. 2008;29(Suppl B):115–20.
Eichenlaub-Ritter U, Schmiady H, Kentenich H, Soewarto D. Recurrent failure in polar body formation and premature chromosome condensation in oocytes from a human patient: indicators of asynchrony in nuclear and cytoplasmic maturation. Hum Reprod. 1995;10(9):2343–9.
Austin CR. Anomalies of fertilization leading to triploidy. J Cell Comp Physiol. 1960;56(Suppl 1):1–15.
Rosenbusch B. The potential significance of binovular follicles and binucleate giant oocytes for the development of genetic abnormalities. J Genet. 2012;91(3):397–404.
Van Blerkom J. Occurrence and developmental consequences of aberrant cellular organization in meiotically mature human oocytes after exogenous ovarian hyperstimulation. J Electron Microsc Tech. 1990;16(4):324–46.
Veeck L, El Shafie M, Sousa M, Windt M-L, Kruger TF. An Atlas of the Ultrastructure of Human Oocytes: A Guide for Assisted Reproduction, First Edition. New York: The Parthenon Publishing Group, 2000. Fertil Steril. 2001;75(4):838–9.
ESHRE Special Interest Group of Embryology and Alpha Scientists in Reproductive Medicine. Electronic address: coticchio.biogenesi@grupposandonato.it. The Vienna consensus: report of an expert meeting on the development of ART laboratory performance indicators. Reprod Biomed Online. 2017; 35(5):494–510
Funding
The study was funded by the authors’ institution.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bartolacci, A., Intra, G., Coticchio, G. et al. Does morphological assessment predict oocyte developmental competence? A systematic review and proposed score. J Assist Reprod Genet 39, 3–17 (2022). https://doi.org/10.1007/s10815-021-02370-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02370-3