Abstract
Purpose
To investigate whether live birth rates from euploid blastocyst frozen-thawed embryo transfer (FET) cycles are associated with infertility diagnosis or oocyte source.
Design
Retrospective analysis of FET cycles reported to SART CORS in 2014.
Methods
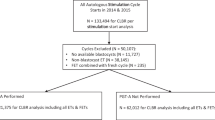
Data from fresh IVF cycles with preimplantation genetic testing for aneuploidy (PGT-A), linked to the first FET cycles, were collected from the 2014 SART CORS database for autologous and donor oocyte cycles. Inclusion criteria were patients undergoing FET with euploid embryos (n = 4148). Demographic data including age, BMI, prior fertility, and etiology of infertility were collected from the retrieval cycle and analyzed. Patients with uterine anomalies, preimplantation genetic testing-mutation (PGT-M) for genetic diseases, gender selection, HLA determination, or systemic and immunologic disorders were excluded. The primary outcome measure was live birth (LB) rate. Potential confounders such as age, prior fertility, and maximum baseline FSH values were analyzed with regression models as indicated.
Results
Though age, maximum baseline FSH, and infertility diagnosis were significantly different, LB was similar between patients undergoing autologous or donor oocyte FET cycles. Etiology of infertility was not significantly associated with LB in autologous cycles (p = 0.95). Potential confounders such as maternal age, prior fertility, and maximum baseline FSH were not associated with outcomes; however, maternal BMI was inversely related to LB in autologous cycles, with an odds ratio of 0.97 (95% CI: 0.96–0.98 (rho = − 0.08, p < 0.01)).
Conclusions
After controlling for confounding variables, a euploid embryo derived from a donor or autologous oocyte results in similar LB in women with different infertility diagnoses.

Similar content being viewed by others
Data availability
SART CORS database available with application to SART.
References
Hassold T, Abruzzo M, Adkins K, Griffin D, Merrill M, Millie E, et al. Human aneuploidy: incidence, origin, and etiology. Environ Mol Mutagen. 1996;28(3):167–75. https://doi.org/10.1002/(sici)1098-2280(1996)28:3<167::Aid-em2>3.0.Co;2-b.
Scott RT Jr, Upham KM, Forman EJ, Zhao T, Treff NR. Cleavage-stage biopsy significantly impairs human embryonic implantation potential while blastocyst biopsy does not: a randomized and paired clinical trial. Fertil Steril. 2013;100(3):624–30. https://doi.org/10.1016/j.fertnstert.2013.04.039.
Forman EJ, Hong KH, Ferry KM, Tao X, Taylor D, Levy B, et al. In vitro fertilization with single euploid blastocyst transfer: a randomized controlled trial. Fertil Steril. 2013;100(1):100–7.e1. https://doi.org/10.1016/j.fertnstert.2013.02.056.
Dahdouh EM, Balayla J, Garcia-Velasco JA. Comprehensive chromosome screening improves embryo selection: a meta-analysis. Fertil Steril. 2015;104(6):1503–12. https://doi.org/10.1016/j.fertnstert.2015.08.038.
Franasiak JM, Scott RT. Contribution of immunology to implantation failure of euploid embryos. Fertil Steril. 2017;107(6):1279–83. https://doi.org/10.1016/j.fertnstert.2017.04.019.
Luo L, Gu F, Jie H, Ding C, Zhao Q, Wang Q, et al. Early miscarriage rate in lean polycystic ovary syndrome women after euploid embryo transfer - a matched-pair study. Reprod BioMed Online. 2017;35(5):576–82. https://doi.org/10.1016/j.rbmo.2017.07.010.
Lessey BA, Young SL. What exactly is endometrial receptivity? Fertil Steril. 2019;111(4):611–7. https://doi.org/10.1016/j.fertnstert.2019.02.009.
Bellver J, Simón C. Implantation failure of endometrial origin: what is new? Curr Opin Obstet Gynecol. 2018;30(4):229–36. https://doi.org/10.1097/gco.0000000000000468.
Perkins KM, Boulet SL, Jamieson DJ, Kissin DM. Trends and outcomes of gestational surrogacy in the United States. Fertil Steril. 2016;106(2):435–42.e2. https://doi.org/10.1016/j.fertnstert.2016.03.050.
Galgani M, Insabato L, Cali G, Della Gatta AN, Mirra P, Papaccio F, et al. Regulatory T cells, inflammation, and endoplasmic reticulum stress in women with defective endometrial receptivity. Fertil Steril. 2015;103(6):1579–86.e1. https://doi.org/10.1016/j.fertnstert.2015.03.014.
Geva E, Yaron Y, Lessing JB, Yovel I, Vardinon N, Burke M, et al. Circulating autoimmune antibodies may be responsible for implantation failure in in vitro fertilization. Fertil Steril. 1994;62(4):802–6. https://doi.org/10.1016/S0015-0282(16)57008-3.
Mazzilli R, Cimadomo D, Vaiarelli A, Capalbo A, Dovere L, Alviggi E, et al. Effect of the male factor on the clinical outcome of intracytoplasmic sperm injection combined with preimplantation aneuploidy testing: observational longitudinal cohort study of 1,219 consecutive cycles. Fertil Steril. 2017;108(6):961–72.e3. https://doi.org/10.1016/j.fertnstert.2017.08.033.
Weghofer A, Munne S, Chen S, Barad D, Gleicher N. Lack of association between polycystic ovary syndrome and embryonic aneuploidy. Fertil Steril. 2007;88(4):900–5. https://doi.org/10.1016/j.fertnstert.2006.12.018.
Center for Disease Control and Prevention ASRM, and Society for Assisted Reproductive Technology. 2012 assisted reproductive technology success rates: national summary and fertility clinic reports US Dept of Health and Human Services. 2014. http://www.cdc.gov/art/pdf/2012-report/national-summary/art_2012_national_summary_report.pdf.
Sparic R, Mirkovic L, Malvasi A, Tinelli A. Epidemiology of uterine myomas: a review. Int J Fertil Steril. 2016;9(4):424–35.
Dandolu V, Singh R, Lidicker J, Harmanli O. BMI and uterine size: is there any relationship? Int J Gynecol Pathol Off J Int Soc Gynecol Pathol. 2010;29(6):568–71. https://doi.org/10.1097/PGP.0b013e3181e8ae64.
Pal L, Santoro N. Age-related decline in fertility. Endocrinol Metab Clin N Am. 2003;32(3):669–88. https://doi.org/10.1016/S0889-8529(03)00046-X.
Malizia BA, Hacker MR, Penzias AS. Cumulative live-birth rates after in vitro fertilization. N Engl J Med. 2009;360(3):236–43. https://doi.org/10.1056/NEJMoa0803072.
Bellver J, Ayllon Y, Ferrando M, Melo M, Goyri E, Pellicer A, et al. Female obesity impairs in vitro fertilization outcome without affecting embryo quality. Fertil Steril. 2010;93(2):447–54. https://doi.org/10.1016/j.fertnstert.2008.12.032.
Provost MP, Acharya KS, Acharya CR, Yeh JS, Steward RG, Eaton JL, et al. Pregnancy outcomes decline with increasing body mass index: analysis of 239,127 fresh autologous in vitro fertilization cycles from the 2008–2010 Society for Assisted Reproductive Technology registry. Fertil Steril. 2016;105(3):663–9. https://doi.org/10.1016/j.fertnstert.2015.11.008.
Guidance on the limits to the number of embryos to transfer: a committee opinion. Fertil Steril. 2017;107(4):901–3. https://doi.org/10.1016/j.fertnstert.2017.02.107.
Gonzalez-Comadran M, Schwarze JE, Zegers-Hochschild F, Souza MD, Carreras R, Checa MA. The impact of endometriosis on the outcome of assisted reproductive technology. Reprod Biol Endocrinol: RB&E. 2017;15(1):8. https://doi.org/10.1186/s12958-016-0217-2.
La Marca A, Minasi MG, Sighinolfi G, Greco P, Argento C, Grisendi V, et al. Female age, serum antimullerian hormone level, and number of oocytes affect the rate and number of euploid blastocysts in in vitro fertilization/intracytoplasmic sperm injection cycles. Fertil Steril. 2017;108(5):777–83.e2. https://doi.org/10.1016/j.fertnstert.2017.08.029.
Reig A, Franasiak J, Scott RT Jr, Seli E. The impact of age beyond ploidy: outcome data from 8175 euploid single embryo transfers. J Assist Reprod Genet. 2020;37(3):595–602. https://doi.org/10.1007/s10815-020-01739-0.
Shah DK, Missmer SA, Berry KF, Racowsky C, Ginsburg ES. Effect of obesity on oocyte and embryo quality in women undergoing in vitro fertilization. Obstet Gynecol. 2011;118(1):63–70. https://doi.org/10.1097/AOG.0b013e31821fd360.
Maheshwari A, Stofberg L, Bhattacharya S. Effect of overweight and obesity on assisted reproductive technology--a systematic review. Hum Reprod Update. 2007;13(5):433–44. https://doi.org/10.1093/humupd/dmm017.
Zaadstra BM, Seidell JC, Van Noord PA, te Velde ER, Habbema JD, Vrieswijk B, et al. Fat and female fecundity: prospective study of effect of body fat distribution on conception rates. BMJ: Br Med J. 1993;306(6876):484–7.
Thaler JP, Schwartz MW. Minireview: inflammation and obesity pathogenesis: the hypothalamus heats up. Endocrinology. 2010;151(9):4109–15. https://doi.org/10.1210/en.2010-0336.
Nteeba J, Ganesan S, Keating AF. Progressive obesity alters ovarian folliculogenesis with impacts on pro-inflammatory and steroidogenic signaling in female mice. Biol Reprod. 2014;91(4):86. https://doi.org/10.1095/biolreprod.114.121343.
Bellver J, Melo MA, Bosch E, Serra V, Remohi J, Pellicer A. Obesity and poor reproductive outcome: the potential role of the endometrium. Fertil Steril. 2007;88(2):446–51. https://doi.org/10.1016/j.fertnstert.2006.11.162.
Orostica L, Astorga I, Plaza-Parrochia F, Vera C, Garcia V, Carvajal R, et al. Proinflammatory environment and role of TNF-alpha in endometrial function of obese women having polycystic ovarian syndrome. Int J Obes (2005). 2016;40(11):1715–22. https://doi.org/10.1038/ijo.2016.154.
Pinborg A, Gaarslev C, Hougaard CO, Nyboe Andersen A, Andersen PK, Boivin J, et al. Influence of female bodyweight on IVF outcome: a longitudinal multicentre cohort study of 487 infertile couples. Reprod BioMed Online. 2011;23(4):490–9. https://doi.org/10.1016/j.rbmo.2011.06.010.
Veleva Z, Tiitinen A, Vilska S, Hyden-Granskog C, Tomas C, Martikainen H, et al. High and low BMI increase the risk of miscarriage after IVF/ICSI and FET. Human Reprod (Oxf, Engl). 2008;23(4):878–84. https://doi.org/10.1093/humrep/den017.
Provost MP, Acharya KS, Acharya CR, Yeh JS, Steward RG, Eaton JL, et al. Pregnancy outcomes decline with increasing recipient body mass index: an analysis of 22,317 fresh donor/recipient cycles from the 2008-2010 Society for Assisted Reproductive Technology Clinic Outcome Reporting System registry. Fertil Steril. 2016;105(2):364–8. https://doi.org/10.1016/j.fertnstert.2015.10.015.
Fiorentino F, Bono S, Biricik A, Nuccitelli A, Cotroneo E, Cottone G, et al. Application of next-generation sequencing technology for comprehensive aneuploidy screening of blastocysts in clinical preimplantation genetic screening cycles. Hum Reprod (Oxf, Engl). 2014;29(12):2802–13. https://doi.org/10.1093/humrep/deu277.
Acknowledgments
SART wishes to thank all of its members for providing clinical information to the SART CORS database for use by patients and researchers. Without the efforts of our members, this research would not have been possible.
Author information
Authors and Affiliations
Contributions
FM, SJ, EW, and EB contributed to the study conception and design. EW assisted with data acquisition and material preparation. FM, MG, EB, and SJ performed data analysis, interpretation, and writing of the manuscript. All authors edited and approved the final manuscript.
Corresponding author
Ethics declarations
This study was approved by the institutional review board of Albert Einstein College of Medicine.
Conflict of interest
FM, MG, EB, and SJ with nothing to disclose. EW employed by Redshift technologies, the data vendor for SART.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
F. Meng and M. Goldsammler share first authorship equally.
Rights and permissions
About this article
Cite this article
Meng, F., Goldsammler, M., Wantman, E. et al. Live birth rate from euploid blastocysts is not associated with infertility etiology or oocyte source following frozen-thawed embryo transfer (FET): analysis of 4148 cycles reported to SART CORS. J Assist Reprod Genet 38, 185–192 (2021). https://doi.org/10.1007/s10815-020-01996-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-020-01996-z