Abstract
Purpose
The aims of this study were to assess the outcome of in vitro fertilization (IVF) in women with very low circulating anti-müllerian hormone (AMH) and to investigate factors affecting their probability of pregnancy.
Methods
The outcome of 448 IVF cycles in 361 women with circulating AMH <0.5 ng/ml was retrospectively analyzed.
Results
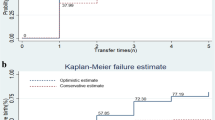
Cycle cancellation rate was 14.5 %; patients whose cycle was cancelled had significantly lower AMH than women who reached oocyte pickup (OPU). Among those who reached OPU, age significantly affected the success rate: despite comparable AMH levels, patients below 35 years obtained significantly more oocytes and a better clinical pregnancy rate (CPR)/OPU than patients aged 35–39 or 40–43 (31 % vs. 23.2 % vs. 10.2 %, respectively; p = 0.001). Differently, comparable IVF results were observed stratifying patients for AMH levels in the range 0.14–0.49 ng/ml. Multivariable logistic regression analysis confirmed that the probability of pregnancy was significantly affected by age, but not by small differences in AMH level.
Conclusions
Women with very low (<0.5 ng/ml) AMH levels undergoing IVF still have reasonable chances of achieving a pregnancy, but their prognosis is significantly affected by chronological age. Very low AMH levels are associated with a relevant risk of cycle cancellation but should not be considered a reason to exclude a couple from IVF.
Similar content being viewed by others
References
Broekmans FJ, Knauff EA, te Velde ER, Macklon NS, Fauser BC. Female reproductive ageing: current knowledge and future trends. Trends Endocrinol Metab. 2007;18:58–65.
Steiner AZ. Clinical implications of ovarian reserve testing. Obstet Gynecol Surv. 2009;64:120–8.
Broekmans FJ, Kwee J, Hendriks DJ, Mol BW, Lambalk CB. A systematic review of tests predicting ovarian reserve and IVF outcome. Hum Reprod Update. 2006;12:685–718.
Dewailly D, Andersen CY, Balen A, Broekmans F, Dilaver N, Fanchin R, et al. The physiology and clinical utility of anti-mullerian hormone in women. Hum Reprod Update. 2014;20:370–85.
La Marca A, Giulini S, Tirelli A, Bertucci E, Marsella T, Xella S, et al. Anti-müllerian hormone measurement on any day of the menstrual cycle strongly predicts ovarian response in assisted reproductive technology. Hum Reprod. 2007;22:766–71.
Nelson SM, Yates RW, Fleming R. Serum anti-müllerian hormone and FSH: prediction of live birth and extremes of response in stimulated cycles—implications for individualization of therapy. Hum Reprod. 2007;22:2414–21.
Muttukrishna S, Suharjono H, McGarrigle H, Sathanandan M. Inhibin B and anti-mullerian hormone: markers of ovarian response in IVF/ICSI patients? Bjog. 2004;111:1248–53.
Lekamge DN, Barry M, Kolo M, Lane M, Gilchrist RB, Tremellen KP. Anti-müllerian hormone as a predictor of IVF outcome. Reprod Biomed Online. 2007;14:602–10.
Koshy AK, Gudi A, Shah A, Bhide P, Timms P, Homburg R. Pregnancy prognosis in women with anti-müllerian hormone below the tenth percentile. Gynecol Endocrinol. 2013;29:662–5.
Nelson SM, Yates RW, Lyall H, Jamieson M, Traynor I, Gaudoin M, et al. Anti-müllerian hormone-based approach to controlled ovarian stimulation for assisted conception. Hum Reprod. 2009;24:867–75.
Merhi Z, Zapantis A, Berger DS, Jindal SK. Determining an anti-mullerian hormone cutoff level to predict clinical pregnancy following in vitro fertilization in women with severely diminished ovarian reserve. J Assist Reprod Genet. 2013;30:1361–5.
Tocci A, Ferrero S, Iacobelli M, Greco E. Negligible serum anti-mullerian hormone: pregnancy and birth after a 1-month course of an oral contraceptive, ovarian hyperstimulation, and intracytoplasmic sperm injection. Fertil Steril. 2009;92:395 e399–12.
Weghofer A, Dietrich W, Barad DH, Gleicher N. Live birth chances in women with extremely low-serum anti-mullerian hormone levels. Hum Reprod. 2011;26:1905–9.
Fraisse T, Ibecheole V, Streuli I, Bischof P, de Ziegler D. Undetectable serum anti-müllerian hormone levels and occurrence of ongoing pregnancy. Fertil Steril. 2008;89:723 e729–711.
Tokura Y, Yoshino O, Ogura-Nose S, Motoyama H, Harada M, Osuga Y, et al. The significance of serum anti-müllerian hormone (AMH) levels in patients over age 40 in first IVF treatment. J Assist Reprod Genet. 2013;30:821–5.
Holte J, Berglund L, Milton K, Garello C, Gennarelli G, Revelli A, et al. Construction of an evidence-based integrated morphology cleavage embryo score for implantation potential of embryos scored and transferred on day 2 after oocyte retrieval. Hum Reprod. 2007;22:548–57.
Marinakis G, Nikolaou D. What is the role of assisted reproduction technology in the management of age-related infertility? Hum Fertil (Camb). 2011;14:8–15.
La Marca A, Sunkara SK. Individualization of controlled ovarian stimulation in IVF using ovarian reserve markers: from theory to practice. Hum Reprod Update. 2014;20:124–40.
Nardo LG, Gelbaya TA, Wilkinson H, Roberts SA, Yates A, Pemberton P, et al. Circulating basal anti-müllerian hormone levels as predictor of ovarian response in women undergoing ovarian stimulation for in vitro fertilization. Fertil Steril. 2009;92:1586–93.
Gleicher N, Weghofer A, Barad DH. Anti-müllerian hormone (AMH) defines, independent of age, low versus good live-birth chances in women with severely diminished ovarian reserve. Fertil Steril. 2010;94:2824–7.
Brodin T, Hadziosmanovic N, Berglund L, Olovsson M, Holte J. Antimüllerian hormone levels are strongly associated with live-birth rates after assisted reproduction. J Clin Endocrinol Metab. 2013;98:1107–14.
Iliodromiti S, Kelsey TW, Wu O, Anderson RA, Nelson SM. The predictive accuracy of anti-müllerian hormone for live birth after assisted conception: a systematic review and meta-analysis of the literature. Hum Reprod Update. 2014;20:560–70.
Lukaszuk K, Kunicki M, Liss J, Bednarowska A, Jakiel G. Probability of live birth in women with extremely low anti-müllerian hormone concentrations. Reprod Biomed Online. 2014;28:64–9.
Kedem A, Haas J, Geva LL, Yerushalmi G, Gilboa Y, Kanety H, et al. Ongoing pregnancy rates in women with low and extremely low AMH levels. A multivariate analysis of 769 cycles. PLoS ONE. 2013;8:e81629.
Gianaroli L, Magli MC, Ferraretti AP, Fortini D, Tabanelli C, Gergolet M. Gonadal activity and chromosomal constitution of in vitro generated embryos. Mol Cell Endocrinol. 2000;161:111–6.
Wang JG, Douglas NC, Nakhuda GS, Choi JM, Park SJ, Thornton MH, et al. The association between anti-müllerian hormone and IVF pregnancy outcomes is influenced by age. Reprod Biomed Online. 2010;21:757–61.
van Loendersloot LL, van Wely M, Limpens J, Bossuyt PM, Repping S, van der Veen F. Predictive factors in in vitro fertilization (IVF): a systematic review and meta-analysis. Hum Reprod Update. 2010;16:577–89.
Lee RK, Wu FS, Lin MH, Lin SY, Hwu YM. The predictability of serum anti-müllerian level in IVF/ICSI outcomes for patients of advanced reproductive age. Reprod Biol Endocrinol. 2011;9:115.
Bhide P, Gudi A, Shah A, Timms P, Grayson K, Homburg R. Anti-müllerian hormone as a predictor of pregnancy following IVF. Reprod Biomed Online. 2013;26:247–52.
Brodin T, Hadziosmanovic N, Berglund L, Olovsson M, Holte J. Comparing four ovarian reserve markers—associations with ovarian response and live births after assisted reproduction. Acta Obstet Gynecol Scand. 2015;94:1056–63.
Honnma H, Baba T, Sasaki M, Hashiba Y, Oguri H, Fukunaga T, et al. Different ovarian response by age in an anti-müllerian hormone-matched group undergoing in vitro fertilization. J Assist Reprod Genet. 2012;29:117–25.
Casadei L, Manicuti C, Puca F, Madrigale A, Emidi E, Piccione E. Can anti-müllerian hormone be predictive of spontaneous onset of pregnancy in women with unexplained infertility? J Obstet Gynaecol. 2013;33:857–61.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule: Women with very low (<0.5 ng/ml) AMH levels undergoing IVF have an increased risk of cycle cancellation, and their prognosis is significantly affected by chronological age.
Rights and permissions
About this article
Cite this article
Revelli, A., Biasoni, V., Gennarelli, G. et al. IVF results in patients with very low serum AMH are significantly affected by chronological age. J Assist Reprod Genet 33, 603–609 (2016). https://doi.org/10.1007/s10815-016-0675-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-016-0675-7