Abstract
Purpose
To investigate the impact of elevated serum estradiol (E2) levels on the day of hCG trigger on the birth weight of term singletons after fresh In Vitro Fertilization (IVF)-Embryo Transfer (ET) cycles.
Methods
Retrospective cohort study of all patients initiating fresh IVF-ET cycles resulting in live births between January 2004 and February 2013. The incidence of low birthweight (LBW) term singletons in patients with E2 levels on day of hCG trigger above or below the 95 % cutoff for E2 values in our clinic (3,069.2 pg/mL) was estimated. Multiple gestations and vanishing twin pregnancies were excluded.
Results
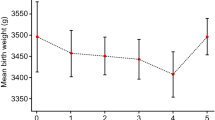
Two thousand nine hundred thirty-nine singleton live births were identified for inclusion. One hundred forty seven (5 %) and 2792 (95 %) live singleton births occurred in patients with peak E2 levels above and below 3,069.2 pg/mL, respectively. The overall incidence of term LBW was 5.4 % in the >3,069.2 pg/mL group compared to 2.4 % in the ≤3,069.2 pg/mL group (P = .038). An E2 level >3,069.2 pg/mL on the day of hCG administration was associated with increased odds of LBW term singletons (OR = 2.29; 95 % CI = 1.03–5.11). The increased odds remained unchanged when adjusting for maternal age (aOR = 2.29; 95 % CI = 1.02–5.14; P = .037), gestational age at delivery (aOR = 2.04; 95 % CI = 1.22–3.98; P = .025), and day 3 versus blastocyst transfer (aOR = 2.5; 95 % CI = 1.11–5.64; P = .023).
Conclusions
Peak E2 level >3,069.2 pg/mL is associated with increased odds of LBW term singletons after fresh IVF-ET cycles. Conservative stimulation protocols aiming not to exceed an E2 level of 3,000 pg/mL may be advantageous for placentation and fetal growth if a fresh transfer is planned.

Similar content being viewed by others
References
Sunderam S, Kissin DM, Crawford S, Anderson JE, Folger SG, Jamieson DJ, et al. Assisted reproductive technology surveillance – United States, 2010. MMWR Surveill Summ. 2013;62(9):1–24.
Center for Disease Control and Prevention. Assisted Reproductive Technology (ART). Available at: http://www.cdc.gov/art. Accessed on 10/18/2014.
Kalra SK, Barnhart KT. In vitro fertilization and adverse childhood outcomes: what we know, where we are going, and how we will get there. A glimpse into what lies behind and beckons ahead. Fertil Steril. 2011;95(6):1887–9.
Kondapalli LA, Perales-Puchalt A. Low birth weight: is it related to assisted reproductive technology or underlying infertility? Fertil Steril. 2013;99(2):303–10.
Barnhart KT. Assisted reproductive technologies and perinatal morbidity: interrogating the association. Fertil Steril. 2013;99(2):299–302.
Schieve LA, Meikle SF, Ferre C, Peterson HB, Jeng G, Wilcox LS. Low and very low birth weight in infants conceived with the use of assisted reproductive technology. N Engl J Med. 2002;346:731–7.
Helmerhorst FM, Perquin DA, Donker D, Keirse MJ. Perinatal outcome of singletons and twins after assisted conception; a systematic review of controlled studies. BMJ. 2004;328:261–5.
Jackson R, Gibson KA, Wu YW, Croughan MS. Perinatal outcomes in singletons following in vitro fertilization: a meta-analysis. Obstet Gynecol. 2004;130:551–63.
McDonald SD, Han Z, Mulla S, Murphy KE, Beyene J, Ohlsson A. Preterm birth and low birth weight among in vitro fertilization singletons: a systematic review and meta-analyses. Eur J Obstet Gynecol Reprod Biol. 2009;146:138–48.
Kalra SK, Ratcliffe SJ, Coutifaris C, Molinaro T, Barnhart KT. Ovarian stimulation and low birth weight in newborns conceived through in vitro fertilization. Obstet Gynecol. 2011;118(4):863–71.
Imudia AN, Awonuga AO, Doyle JO, Kaimal AJ, Wright DL, Toth TL, et al. Peak serum estradiol level during controlled ovarian hyperstimulation is associated with increased risk of small for gestational age and preeclampsia in singleton pregnancies after in vitro fertilization. Fertil Steril. 2012;97(6):1374–9.
Spong CY, Mercer BM, D’alton M, Kilpatrick S, Blackwell S, Saade G. Timing of indicated late-preterm and early-term birth. Obstet Gynecol. 2011;118(2 Pt 1):323–33.
Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996;87:163–8.
Reichman DE, Greenwood E, Meyer L, Kligman I, Rosenwaks Z. Can in vitro fertilization cycles be salvaged by repeat administration of intramuscular human chorionic gonadotropin the day after failed injection? Fertil Steril. 2012;98:671–4.
Reichman DE, Chung P, Meyer L, Greenwood E, Davis O, Rosenwaks Z. Consecutive gonadotropin-releasing hormone-antagonist in vitro fertilization cycles: does the elapsed time interval between successive treatments affect outcomes? Fertil Steril. 2013;99:1277–82.
Reichman DE, Goldschlag D, Rosenwaks Z. Value of antimüllerian hormone as a prognostic indicator of in vitro fertilization outcome. Fertil Steril. 2014;98(5):1225–8.
Engmann L, Benadiva C. Agonist trigger: what is the best approach? Agonist trigger with aggressive luteal support. Fertil Steril. 2012;97:531–3.
Ma WG, Song H, Das SK, Paria BC, Dey SK. Estrogen is a critical determinant that specifies the duration of the window of uterine receptivity for implantation. Proc Natl Acad Sci U S A. 2003;100:2963–8.
Valbuena D, Martin J, de Pablo JL, Remohi J, Pellicer A, Simon C. Increasing levels of estradiol are deleterious to embryonic implantation because they directly affect the embryo. Fertil Steril. 2001;76:962–8.
Bittner AK, Horsthemke B, Winterhager E, Grummer R. Hormone-induced delayed ovulation affects early embryonic development. Fertil Steril. 2011;95:2390–4.
Ertzeid G, Storeng R. The impact of ovarian stimulation on implantation and fetal development in mice. Hum Reprod. 2001;16:221–5.
Kalra SK. Adverse perinatal outcome and in vitro fertilization singleton pregnancies: what lies beneath? Further evidence to support an underlying role of the modifiable hormonal milieu in in vitro fertilization stimulation. Fertil Steril. 2012;97(6):1295–6.
Albrecht ED, Bonagura TW, Burleigh DW, Enders AC, Aberdeen GW, Pepe GJ. Suppression of extravillous trophoblast invasion of uterine spiral arteries by estrogen during early baboon pregnancy. Placenta. 2006;27:483–90.
Simon C, Cano F, Valbuena D, Remohi J, Pellicer A. Clinical evidence for a detrimental effect on uterine receptivity of high serum oestradiol concentrations in high and normal responder patients. Hum Reprod. 1995;10:2432–7.
Valbuena D, Jasper M, Remohi J, Pellicer A, Simon C. Ovarian stimulation and endometrial receptivity. Hum Reprod. 1999;14 Suppl 2:107–11.
Norwitz ER, Schust DJ, Fisher SJ. Implantation and the survival of early pregnancy. N Engl J Med. 2001;345:1400–8.
Dominguez F, Remohi J, Pellicer A, Simon C. Human endometrial receptivity: a genomic approach. Reprod Biomed Online. 2003;6:332–8.
Horcajadas JA, Riesewijk A, Polman J, van Os R, Pellicer A, Mosselman S, et al. Effect of controlled ovarian hyperstimulation in IVF on endometrial gene expression profiles. Mol Hum Reprod. 2005;11:195–205.
Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84.
Barnhart KT. Introduction: are we ready to eliminate the transfer of fresh embryos in in vitro fertilization? Fertil Steril. 2014;102(1):1–2.
Grella PV. Low birth weight and early life origins of adult disease: insulin resistance and type 2 diabetes. Clin Exp Obstet Gynecol. 2007;34(1):9–13.
Nesterenko TH, Aly H. Fetal and neonatal programming: evidence and clinical implications. Am J Perinatol. 2009;26(3):191–8.
Negrato C, Gomes M. Low birth weight: causes and consequences. Diabetol Metab Syndr. 2013;5(1):49.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule Peak estradiol levels and birth weight
Nigel Pereira and David E. Reichman contributed equally to this work.
Rights and permissions
About this article
Cite this article
Pereira, N., Reichman, D.E., Goldschlag, D.E. et al. Impact of elevated peak serum estradiol levels during controlled ovarian hyperstimulation on the birth weight of term singletons from fresh IVF-ET cycles. J Assist Reprod Genet 32, 527–532 (2015). https://doi.org/10.1007/s10815-015-0434-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-015-0434-1