Abstract
Purpose
To study effects of hemodialysis (HD) on retinal and choroidal vasculature in patients with end-stage kidney disease (ESKD) using optical coherence tomography angiography (OCTA).
Methods
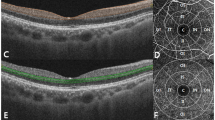
In this prospective study, we investigated eyes of patients undergoing hemodialysis for ESKD from Mondor University Hospital. Only one eye/patient was considered. Subfoveal choroidal thickness (SCT) was measured on enhanced-depth imaging optical coherence tomography (EDI-OCT) before and after the hemodialysis session. OCTA was used to extract retinal vascular density (superficial and deep capillary plexus, SCP, DCP) and choriocapillaris non-perfusion. Clinical, demographic and biological parameters (Blood B-Nitric Peptid rate prior to HD session) were reviewed.
Results
Twenty patients (mean age 53.2 ± 13.6 years, 10 males and 10 females) were included in this prospective study. SCT significantly decreased after the HD session (234.3 ± 56.14 µm before HD to 211.9 ± 60.79 µm after hemodialysis (Wilcoxon signed-rank test, p = 0.003)). Non-perfusion in the choriocapillaris significantly increased after HD (41.65 ± 3.58 before HD, 42.95 ± 3.19 after HD, p = 0.036) while no significant modification of the vascular density was observed in the retinal vasculature (SCP, DCP) around the macular zone or the optic nerve. An increased plasma B-Nitric Peptide (BNP) level prior to the onset of the HD session was significantly correlated with the decrease of the SCT (r = 0.45, p = 0.043).
Conclusion
Hemodialysis in patients with ESKD is associated with a significant decrease in SCT and an increase in non-perfusion in the choriocapillaris on OCTA. A High BNP level prior to the onset of the hemodialysis appears to be correlated with the decrease in SCT.

Similar content being viewed by others
References
Singh AT, Mc Causland FR (2017) Osmolality and blood pressure stability during hemodialysis. Semin Dial 30(6):509–517. https://doi.org/10.1111/sdi.12629
Elbay A, Altinisik M, Dincyildiz A et al (2017) Are the effects of hemodialysis on ocular parameters similar during and after a hemodialysis session? Arq Bras Oftalmol 80(5):290–295. https://doi.org/10.5935/0004-2749.20170071
Chen H, Zhang X, Shen X (2018) Ocular changes during hemodialysis in patients with end-stage renal disease. BMC Ophthalmol 18(1):208. https://doi.org/10.1186/s12886-018-0885-0
Chang IB, Lee JH, Kim JS (2017) Changes in choroidal thickness in and outside the macula after hemodialysis in patients with end-stage renal disease. Retina Phila Pa 37(5):896–905. https://doi.org/10.1097/IAE.0000000000001262
Nakano H, Hasebe H, Murakami K et al (2020) Choroid structure analysis following initiation of hemodialysis by using swept-source optical coherence tomography in patients with and without diabetes. PLoS ONE 15(9):e0239072. https://doi.org/10.1371/journal.pone.0239072
Ishibazawa A, Nagaoka T, Minami Y, Kitahara M, Yamashita T, Yoshida A (2015) Choroidal thickness evaluation before and after hemodialysis in patients with and without diabetes. Invest Ophthalmol Vis Sci 56(11):6534–6541. https://doi.org/10.1167/iovs.15-16719
Shin YU, Lee SE, Kang MH, Han SW, Yi JH, Cho H (2019) Evaluation of changes in choroidal thickness and the choroidal vascularity index after hemodialysis in patients with end-stage renal disease by using swept-source optical coherence tomography. Medicine (Baltimore) 98(18):e15421. https://doi.org/10.1097/MD.0000000000015421
Coppolino G, Carnevali A, Gatti V et al (2021) OCT angiography metrics predict intradialytic hypotension episodes in chronic hemodialysis patients: a pilot, prospective study. Sci Rep 11(1):7202. https://doi.org/10.1038/s41598-021-86609-0
Shin YU, Lee DE, Kang MH et al (2018) Optical coherence tomography angiography analysis of changes in the retina and the choroid after haemodialysis. Sci Rep 8(1):17184. https://doi.org/10.1038/s41598-018-35562-6
Jung JW, Chin HS, Lee DH, Yoon MH, Kim NR (2014) Changes in subfoveal choroidal thickness and choroidal extravascular density by spectral domain optical coherence tomography after haemodialysis: a pilot study. Br J Ophthalmol 98(2):207–212. https://doi.org/10.1136/bjophthalmol-2013-303645
Yang SJ, Han YH, Song GI, Lee CH, Sohn SW (2013) Changes of choroidal thickness, intraocular pressure and other optical coherence tomographic parameters after haemodialysis. Clin Exp Optom 96(5):494–499. https://doi.org/10.1111/cxo.12056
Theodossiadis PG, Theodoropoulou S, Neamonitou G et al (2012) Hemodialysis-induced alterations in macular thickness measured by optical coherence tomography in diabetic patients with end-stage renal disease. Ophthalmol J Int Z Augenheilkd 227(2):90–94. https://doi.org/10.1159/000331321
Kanbay M, Ertuglu LA, Afsar B et al (2020) An update review of intradialytic hypotension: concept, risk factors, clinical implications and management. Clin Kidney J 13(6):981–993. https://doi.org/10.1093/ckj/sfaa078
Assayag M, Levy D, Seris P et al (2020) Relative change of protidemia level predicts intradialytic hypotension. J Am Heart Assoc 9(1):e014264. https://doi.org/10.1161/JAHA.119.014264
Rubinger D, Backenroth R, Sapoznikov D (2013) Sympathetic nervous system function and dysfunction in chronic hemodialysis patients. Semin Dial 26(3):333–343. https://doi.org/10.1111/sdi.12093
Sander BP, Collins MJ, Read SA (2014) The effect of topical adrenergic and anticholinergic agents on the choroidal thickness of young healthy adults. Exp Eye Res 128:181–189. https://doi.org/10.1016/j.exer.2014.10.003
Robinson F, Riva CE, Grunwald JE, Petrig BL, Sinclair SH (1986) Retinal blood flow autoregulation in response to an acute increase in blood pressure. Invest Ophthalmol Vis Sci 27(5):722–726
Kur J, Newman EA, Chan-Ling T (2012) Cellular and physiological mechanisms underlying blood flow regulation in the retina and choroid in health and disease. Prog Retin Eye Res 31(5):377–406. https://doi.org/10.1016/j.preteyeres.2012.04.004
Maisel AS, Krishnaswamy P, Nowak RM et al (2002) Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 347:161–167. https://doi.org/10.1056/NEJMoa020233
Tani T, Nagaoka T, Nakabayashi S, Yoshioka T, Yoshida A (2014) Autoregulation of retinal blood flow in response to decreased ocular perfusion pressure in cats: comparison of the effects of increased intraocular pressure and systemic hypotension. Invest Ophthalmol Vis Sci 55(1):360–367. https://doi.org/10.1167/iovs.13-12591
Holmgaard K, Aalkjaer C, Lambert JDC, Hessellund A, Bek T (2008) The relaxing effect of perivascular tissue on porcine retinal arterioles in vitro is mimicked by N-methyl-D-aspartate and is blocked by prostaglandin synthesis inhibition. Acta Ophthalmol (Copenh) 86(1):26–33. https://doi.org/10.1111/j.1600-0420.2007.01010.x
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Alexandra MIERE (9) and Alexandra MOUALLEM (2) designed the study and developed the protocol. Vincent AUDARD (3), Narindra JOUAN (4) and Philippe GRIMBERT (5) were in charge of the patients who underwent hemodialysis for end-stage kidney failure. Eric H. SOUIED (8) reviewed the manuscript. Samira ZEGRARI (9) collected the data and wrote the manuscript. Hichem SAKHI (7) and Camille JUNG (6) provided the statistical analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zegrari, S., Mouallem, A., Audard, V. et al. Optical coherence tomography angiography analysis of changes in the retina and the choroid after hemodialysis for end stage kidney disease. Int Ophthalmol 43, 4473–4479 (2023). https://doi.org/10.1007/s10792-023-02847-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-023-02847-3