Abstract
Purpose
To report the microbiological spectrum, antimicrobial resistance patterns, and visual outcomes in patients with endogenous endophthalmitis (EE).
Methods
This was a retrospective study of 50 patients with culture-positive EE managed in a tertiary referral center between October 2009 and 2019. Clinical, microbiology analysis, and antimicrobial resistance were reviewed. A multivariable linear regression analysis was used for identifying risk factors associated with worse visual outcomes.
Results
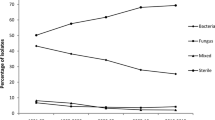
Fifty organisms were identified, 62% bacterial and 38% fungal. The most common bacterial organism was Staphylococcus aureus (75% methicillin resistant), and Candida was the most common fungal species. Multidrug resistance was observed in methicillin-resistant Staphylococcus aureus (MRSA) isolates against clindamycin, daptomycin, and fluoroquinolones. The distributions of the final visual acuity (VA) between the bacterial and fungal groups were significantly different, and the visual outcomes in the bacterial group tended to be worse (p = 0.01). The distributions of enucleation status were significantly higher in bacterial EE (35%) than fungal EE (5.3%) (p = 0.02). Results from the multivariable linear regression analysis revealed that older age was significantly associated with worse visual outcome (coef = 0.03; p = 0.02), while fungal infections were associated with better outcomes (coef = − 0.87; p = 0.01). Intravenous drug use (coef = 0.87; p = 0.054) was a marginally significant factor associated with worse visual outcomes.
Conclusion
There was a higher prevalence of bacterial organisms than fungal species among EE. Bacterial EE was associated with worse visual outcomes and higher enucleation rates than fungal EE. Multidrug resistance was prevalent among MRSA isolates. Older age and intravenous drug use may be factors associated with poor prognosis.
Similar content being viewed by others
Data availability
All data are available upon request.
Code availability
Not applicable.
References
Chee SP, Jap A (2001) Endogenous endophthalmitis. Curr Opin Ophthalmol 12(6):464–470. https://doi.org/10.1097/00055735-200112000-00012
Ness T, Schneider C (2009) Endogenous endophthalmitis caused by methicillin-resistant Staphylococcus aureus (MRSA). Retina 29(6):831–834. https://doi.org/10.1097/IAE.0b013e3181a3b7a1
Greenwald MJ, Wohl LG, Sell CH (1986) Metastatic bacterial endophthalmitis: a contemporary reappraisal. Surv Ophthalmol 31(2):81–101. https://doi.org/10.1016/0039-6257(86)90076-7
Wong JS, Chan TK, Lee HM, Chee SP (2000) Endogenous bacterial endophthalmitis: an east Asian experience and a reappraisal of a severe ocular affliction. Ophthalmology 107(8):1483–1491
Connell PP, O’Neill EC, Fabinyi D, Islam FMA, Buttery R, McCombe M, Essex RW, Roufail E, Clark B, Chiu D, Campbell W, Allen P (2011) Endogenous endophthalmitis: 10-year experience at a tertiary referral centre. Eye 25(1):66–72. https://doi.org/10.1038/eye.2010.145
Shrader SK, Band JD, Lauter CB, Murphy P (1990) The clinical spectrum of endophthalmitis: incidence, predisposing factors, and features influencing outcome. J Infect Dis 162(1):115–120
Okada AA, Johnson RP, Liles WC, D’Amico DJ, Baker AS (1994) Endogenous bacterial endophthalmitis: report of a ten-year retrospective study. Ophthalmology 101(5):832–838
Zhang H, Liu Z (2010) Endogenous endophthalmitis: a 10-year review of culture-positive cases in northern China. Ocul Immunol Inflamm 18(2):133–138. https://doi.org/10.3109/09273940903494717
Schiedler V, Scott IU, Flynn HW, Davis JL, Benz MS, Miller D (2004) Culture-proven endogenous endophthalmitis: clinical features and visual acuity outcomes. Am J Ophthalmol 137:725–731. https://doi.org/10.1016/j.ajo.2003.11.013
Lemley C, Han D (2007) Endophthalmitis: a review of current evaluation and management. Retina 27:662–680
Lee S, Um T, Joe SG, Hwang JU, Kim JG, Yoon YH, Lee JY (2012) Changes in the clinical features and prognostic factors of endogenous endophthalmitis: fifteen years of clinical experience in Korea. Retina 32(5):977–984. https://doi.org/10.1097/IAE.0b013e318228e312
Endophthalmitis Vitrectomy Study Group (1995) Results of the endophthalmitis vitrectomy study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol 113(12):1479–1496
Binder MI, Chua J, Kaiser PK, Procop GW, Isada CM (2003) Endogenous endophthalmitis: an 18-year review of culture-positive cases at a tertiary care center. Medicine (Baltimore) 82(2):97–105. https://doi.org/10.1097/00005792-200303000-00004
Murdoch IE, Morris SS, Cousens SN (1998) People and eyes: statistical approaches in ophthalmology. Br J Ophthalmol 82(8):971–973. https://doi.org/10.1136/bjo.82.8.971
Roberts MF, Fishman GA, Roberts DK, Heckenlively JR, Weleber RG, Anderson RJ, Grover S (2002) Retrospective, longitudinal, and cross sectional study of visual acuity impairment in choroideraemia. Br J Ophthalmol 86(6):658–662
Tirpack AR, Duker JS, Baumal CR (2017) An outbreak of endogenous fungal endophthalmitis among intravenous drug abusers in New England. JAMA Ophthalmol 135(6):534–540. https://doi.org/10.1001/jamaophthalmol.2017.0650
Modjtahedi BS, Finn AP, Barb SM, MacLachlan MJ, van Zyl T, Papakostas TD, Eliott D (2019) Characteristics and outcomes of endogenous endophthalmitis: eight-year experience at a tertiary care center. Ophthalmol Retina 3(1):61–72. https://doi.org/10.1016/j.oret.2018.08.009
Jackson TL, Paraskevopoulos T, Georgalas I (2014) Systematic review of 342 cases of endogenous bacterial endophthalmitis. Surv Ophthalmol 59(6):627–635. https://doi.org/10.1016/j.survophthal.2014.06.002
Sridhar J, Flynn HW, Kuriyan AE, Miller D, Albini T (2013) Endogenous fungal endophthalmitis: risk factors, clinical features, and treatment outcomes in mold and yeast infections. J Ophthalmic Inflamm Infect 3(1):60. https://doi.org/10.1186/1869-5760-3-60
Jackson TL, Eykyn SJ, Graham EM, Stanford MR (2003) Endogenous bacterial endophthalmitis: a 17-year prospective series and review of 267 reported cases. Surv Ophthalmol 48(4):403–423
Jenkins TL, Talcott KE, Matsunaga DR, Ryan ME, Obeid A, Chung CA, Garg SJ (2019) Endogenous bacterial endophthalmitis: a five-year retrospective review at a tertiary care academic center. Ocul Immunol Inflamm. https://doi.org/10.1080/09273948.2019.1642497
Durand ML (2017) Bacterial and fungal endophthalmitis. Clin Microbiol Rev 30(3):597–613. https://doi.org/10.1128/cmr.00113-16
Brod RD, Flynn HW Jr, Clarkson JG, Pflugfelder SC, Culbertson WW, Miller D (1990) Endogenous candida endophthalmitis: management without intravenous amphotericin B. Ophthalmology 97(5):666–672. https://doi.org/10.1016/s0161-6420(90)32547-2
Brod RD, Flynn HWJ (1993) Endophthalmitis: current approaches to diagnosis and therapy. Curr Opin Infect Dis 6(5):637
Essman TF, Flynn HW Jr, Smiddy WE, Brod RD, Murray TG, Davis JL, Rubsamen PE (1997) Treatment outcomes in a 10-year study of endogenous fungal endophthalmitis. Ophthalmic Surg Lasers 28(3):185–194
Nishida T, Ishida K, Niwa Y, Kawakami H, Mochizuki K, Ohkusu K (2015) An eleven-year retrospective study of endogenous bacterial endophthalmitis. J Ophthalmol. https://doi.org/10.1155/2015/261310
Chen YJ, Kuo HK, Wu PC, Kuo ML, Tsai HH, Liu CC, Chen CH (2004) A 10-year comparison of endogenous endophthalmitis outcomes: an east Asian experience with Klebsiella pneumoniae infection. Retina 24(3):383–390. https://doi.org/10.1097/00006982-200406000-00008
Asbell PA, Sanfilippo CM, Pillar CM, DeCory HH, Sahm DF, Morris TW (2015) Antibiotic resistance among ocular pathogens in the united states: five-year results from the antibiotic resistance monitoring in ocular microorganisms (armor) surveillance study. JAMA Ophthalmol 133(12):1445–1454. https://doi.org/10.1001/jamaophthalmol.2015.3888
Yonekawa Y, Chan RV, Reddy AK, Pieroni CG, Lee TC, Lee S (2011) Early intravitreal treatment of endogenous bacterial endophthalmitis. Clin Exp Ophthalmol 39(8):771–778. https://doi.org/10.1111/j.1442-9071.2011.02545.x
Liu C, Bayer A, Cosgrove SE, Daum RS, Fridkin SK, Gorwitz RJ, Kaplan SL, Karchmer AW, Levine DP, Murray BE, Rybak MJ, Talan DA, Chambers HF (2011) Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis Off Publ Infect Dis Soc Am 52(3):285–292. https://doi.org/10.1093/cid/cir034
Whaley SG, Berkow EL, Rybak JM, Nishimoto AT, Barker KS, Rogers PD (2016) Azole antifungal resistance in candida albicans and emerging non-albicans candida species. Front Microbiol 7:2173. https://doi.org/10.3389/fmicb.2016.02173
Lu X, Ng DS, Zheng K, Peng K, Jin C, Xia H, Chen W, Chen H (2016) Risk factors for endophthalmitis requiring evisceration or enucleation. Sci Rep 6:28100. https://doi.org/10.1038/srep28100
Gaton DD, Ehrlich R, Muzmacher L, Hamel N, Lusky M, Weinberger D (2008) Enucleations and eviscerations in a large medical center between the years 1981 and 2007. Harefuah 147(10):758–762, 840
Lingappan A, Wykoff CC, Albini TA, Miller D, Pathengay A, Davis JL, Flynn HW Jr (2012) Endogenous fungal endophthalmitis: causative organisms, management strategies, and visual acuity outcomes. Am J Ophthalmol 153(1):162-166.e161. https://doi.org/10.1016/j.ajo.2011.06.020
Sridhar J, Kuriyan AE, Flynn HW Jr, Miller D (2015) Endophthalmitis caused by pseudomonas aeruginosa: clinical features, antibiotic susceptibilities, and treatment outcomes. Retina 35(6):1101–1106. https://doi.org/10.1097/iae.0000000000000469
Desilets J, Lee CS, Fang W, Hinkle DM (2021) Mortality risk associated with endophthalmitis in West Virginia. Int Ophthalmol 41(8):2887–2895. https://doi.org/10.1007/s10792-021-01849-3
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this paper.
Consent to participate
Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Consent for publication
All information is anonymized and the submission does not include images that may identify the person.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, C.S., Desilets, J., Fang, W. et al. The microbiological spectrum, antimicrobial resistance pattern, and visual outcomes of endogenous endophthalmitis in West Virginia 2009–2019. Int Ophthalmol 42, 3153–3163 (2022). https://doi.org/10.1007/s10792-022-02315-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02315-4