Abstract
Purpose
To evaluate the effects of the central corneal thickness (CCT) and residual stromal thickness (RST) on the formation of opaque bubble layer (OBL) during small-incision lenticule extraction (SMILE).
Methods
A total of 345 eyes from Refractive Surgery Center database at Tianjin Eye Hospital that had been subjected to SMILE surgery and followed for 6 months were included in this study and divided into OBL and OBL-free groups. Preoperative, intraoperative, and postoperative data for all eyes were evaluated and analyzed using multivariate regression analysis. After adjustment for several confounding factors, potential associations of CCT and RST with OBL were elucidated by determining odds ratios (ORs) and 95% confidence intervals (CIs).
Results
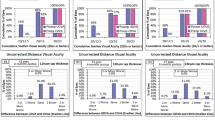
In total, 22 of the 345 eyes developed various degrees of OBL during the femtosecond laser scanning phase of SMILE surgery. After adjustment for age, sex, and refractive errors, significant relationships were detected between CCT and RST and OBL formation (OR 1.04; 95% CI 1.02–1.06; OR 1.03; 95% CI 1.02–1.05, respectively, P < 0.001). Smooth curve fitting revealed an increased risk of OBL in the presence of an increased CCT or RST. However, visual outcomes were comparable between the two groups at both 3 and 6 months postoperatively.
Conclusions
The results suggest that OBL formation during SMILE surgery is more likely in eyes with a thicker cornea. CCT and RST can be considered independent risk factors for OBL formation. Although this phenomenon may disturb the surgical procedure, it is unlikely to affect the postoperative visual outcome.




Similar content being viewed by others
References
Juhasz T, Loesel FH, Kurtz RM, Horvath C (1999) Corneal refractive surgery with femtosecond lasers. IEEE J Sel Top Quantum Electron 5:902–910
Vestergaard AH, Grauslund J, Ivarsen AR, Hjortdal JØ (2014) Efficacy, safety, predictability, contrast sensitivity, and aberrations after femtosecond laser lenticule extraction. J Cataract Refract Surg 40:403–411
Tian H, Ke Z, Chen Y, Yang G, Li H, Zhou X (2016) Four-year observation of predictability and stability of small incision lenticule extraction. BMC Ophthalmol 16:149
Zhang Y, Shen Q, Jia Y, Zhou D, Zhou J (2016) Clinical outcomes of smile and FS-LASIK used to treat myopia: a meta-analysis. J Refract Surg 32:256–265
Reinstein DZ, Archer TJ, Gobbe M (2013) Accuracy and reproducibility of cap thickness in small incision lenticule extraction. J Refract Surg 29:810–818
Reinstein DZ, Gobbe M, Gobbe L, Archer TJ, Carp GI (2015) Optical zone centration accuracy using corneal fixation-based SMILE compared to eye tracker-based femtosecond laser-assisted LASIK for myopia. J Refract Surg 31:586–592
Aristeidou A, Taniguchi EV, Tsatsos M, Muller R, Mcalinden C, Pineda R (2015) The evolution of corneal and refractive surgery with the femtosecond laser. Eye Vis 2:1–14
Ratkay-Traub I, Ferincz IE, Juhasz T, Kurtz RM, Krueger RR (2003) First clinical results with the femtosecond neodynium-glass laser in refractive surgery. J Refract Surg 19:94–103
Luengo Gimeno F, Chan CM, Li L, Tan DT, Mehta JS (2011) Comparison of eye-tracking success in laser in situ keratomileusis after flap creation with 2 femtosecond laser models. J Cataract Refract Surg 37:538–543
Ide T, Yoo SH, Kymionis GD, Haft P, O’Brien TP (2009) Second femtosecond laser pass for incomplete laser in situ keratomileusis flaps caused by suction loss. J Cataract Refract Surg 35:153–157
Ide T, Kymionis GD, Goldman DA, Yoo SH, O’Brien TP (2008) Subconjunctival gas bubble Formation during LASIK flap creation using femtosecond laser. J Refract Surg 24:850–851
Srinivasan S, Herzig S (2007) Sub-epithelial gas breakthrough during femtosecond laser flap creation for LASIK. Br J Ophthalmol 91:1373
Srinivasan S, Rootman DS (2007) Anterior chamber gas bubble formation during femtosecond laser flap creation for LASIK. J Refract Surg 23:828–830
Kaiserman I, Maresky HS, Bahar I, Rootman DS (2008) Incidence, possible risk factors, and potential effects of an opaque bubble layer created by a femtosecond laser. J Cataract Refract Surg 34:417–423
Liu CH, Sun CC, Huikang MD, Chienchieh HJ, Liu CF, Chen HF (2014) Opaque bubble layer: incidence, risk factors, and clinical relevance. J Cataract Refract Surg 40:435–440
Jung HG, Kim J, Lim TH (2015) Possible risk factors and clinical effects of an opaque bubble layer created with femtosecond laser-assisted laser in situ keratomileusis. J Cataract Refract Surg 41:1393–1399
Courtin R, Saad A, Guilbert E, Grise-Dulac A, Gatinel D (2015) Opaque bubble layer risk factors in femtosecond laser-assisted LASIK. J Refract Surg 31:608–612
Son G, Lee J, Jang C, Choi KY, Cho BJ, Lim TH (2017) Possible risk factors and clinical effects of opaque bubble layer in small incision lenticule extraction (SMILE). J Refract Surg 33:24–29
Liu M, Zhou Y, Wu X, Ye T, Liu Q (2016) Comparison of 120- and 140-μm SMILE cap thickness results in eyes with thick corneas. Cornea 35:1
Soong HK, Malta JB (2009) Femtosecond lasers in ophthalmology. Am J Ophthalmol 147:189–197
Shah R, Shah S (2011) Effect of scanning patterns on the results of femtosecond laser lenticule extraction refractive surgery. J Cataract Refract Surg 37:1636–1647
Hamed AM, Fekry AY (2016) Refractive small-incision lenticule extraction: push-up and push-down techniques. J Cataract Refract Surg 42:1713–1715
Jacob S, Nariani A, Figus M, Agarwal A, Agarwal A (2016) White ring sign for uneventful lenticule separation in small-incision lenticule extraction. J Cataract Refract Surg 42:1251–1254
Wang Y, Dou R (2015) The effect of corneal biomechanics of the OBL during SMILE. Cataract Refract Surg Today Eur March:1–3
Acknowledgements
The authors are grateful for the technical support of Tianjin Eye Hospital and Eye Institute, Tianjin Key Laboratory of Ophthalmology and Visual Science.
Funding
This study was supported by the National Natural Science Foundation of China (No. 81670884). The funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
This study was adhered to the tenets of the Declaration of Helsinki and was approved by the ethics committee of Tianjin Eye Hospital.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ma, J., Wang, Y., Li, L. et al. Corneal thickness, residual stromal thickness, and its effect on opaque bubble layer in small-incision lenticule extraction. Int Ophthalmol 38, 2013–2020 (2018). https://doi.org/10.1007/s10792-017-0692-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-017-0692-2