Abstract
A number of authors have argued that technological innovation has increased U.S. health care spending. We investigate the impact that pharmaceutical innovation had on the average cost of U.S. health care episodes during the period 2000–2014, using data from the Bureau of Economic Analysis’ Health Care Satellite Account and other sources. We analyze the relationship across approximately 200 diseases between the growth in the number of drugs that have been approved to treat the disease and the subsequent growth in the mean amount spent per episode of care, controlling for the growth in the number of episodes and other factors. Our estimates indicate that mean episode cost is not significantly related to the number of drugs ever approved 0–4 years before, but it is significantly inversely related to the number of drugs ever approved 5–20 years before. This delay is consistent with the fact (which we document) that utilization of a drug is relatively low during the first few years after it was approved, and that some drugs may have to be consumed for several years to have their maximum impact on treatment cost. Our estimates of the effect of pharmaceutical innovation on the average cost of health care episodes are quite insensitive to the weights used and to whether we control for 3 covariates. Our most conservative estimates imply that the drugs approved during 1986–1999 reduced mean episode cost by 4.7%, and that the drugs approved during 1996–2009 reduced mean episode cost by 2.1%. If drug approvals did not affect the number of episodes, the drugs approved during 1986–1999 would have reduced 2014 medical expenditure by about $93 billion. However, drug approvals may have affected the number, as well as the average cost, of episodes. We also estimate models of hospital utilization. The number of hospital days is significantly inversely related to the number of drugs ever approved 10–19 years before, controlling for the number of disease episodes. Our estimates imply that the drugs approved during 1984–1997 reduced the number of hospital days by 10.5%. The hospital cost reduction was larger than expenditure on the drugs.







Similar content being viewed by others
Notes
Dunn et al (2018) say that “there is evidence that many new technologies are cost-effective, but they are often more expensive than older treatments. That is, despite their cost-effectiveness, they are not cost-saving, which leads to rising health care expenditures.”.
The number of hospital discharges and days of care in 2015 were not significantly related to the number of drugs launched after 2005. As discussed below, utilization of drugs during the first few years after they are launched is relatively low, and drugs for chronic conditions may have to be consumed for several years to achieve full effectiveness.
Several studies have examined the effect of changes in prescription drug use (e.g., due to changes in insurance coverage), as opposed to prescription drug innovation, on medical expenditure. The Congressional Budget Office (2012) estimated that a 1 percent increase in the number of prescriptions filled by beneficiaries would cause Medicare’s spending on medical services to fall by roughly one-fifth of 1 percent.” Roebuck et al (2015) found that “a 1% increase in overall prescription drug use was associated with decreases in total nondrug Medicaid costs by 0.108% for blind or disabled adults, 0.167% for other adults, and 0.041% for children. Reductions in combined inpatient and outpatient spending from increased drug utilization in Medicaid were similar to an estimate for Medicare by the Congressional Budget Office.” Zhang et al (2009) found that “enrollment in Medicare Part D was associated with increased spending on prescription drugs. Groups that had no or minimal drug coverage before the implementation of Part D had reductions in other medical spending that approximately offset the increased spending on drugs, but medical spending increased in the group that had more generous previous coverage.”.
We will also briefly examine the relationship between the growth in the number of drugs used to treat the disease ever approved and the growth in the number of cases of the disease, although this relationship is likely to be subject to reverse causality.
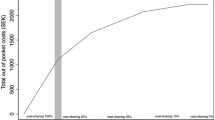
As discussed below, there is likely to be a substantial lag between the approval of a new drug and its maximum impact on health care spending.
Many drugs have multiple indications: 66% of drugs have 2 or more Clinical Classification Software (CCS) indications; 25% of drugs have 5 or more CCS indications.
psn is the mean gross price of the drug, not the price net of rebates. Data on rebates are not available.
The mean net (of rebates) price probably fell by less than 74%. In the U.S. in 2014, rebates reduced total brand name drug cost in Medicare Part D plans by 17.5% (Centers for Medicare and Medicaid Services 2021). Alston et al. (2018) argued that rebates are rarely used for generics, so for generic products, net prices are likely to be very close to the gross prices. According to those authors, “rebates are mostly used for high-cost brand-name prescription drugs in competitive therapeutic classes where there are interchangeable products (rarely for generics), and aim to incentivize PBMs and health insurers to include the pharmaceutical manufacturer’s products on their formularies and to obtain preferred ‘tier’ placement.”.
The e-Drug3D database is based on the FDA’s Drugs@FDA database (Food and Drug Administration 2023a), but the latter does not include WHO ATC codes.
The surge in new drug approvals during the 1990s was partly due to passage by Congress in 1992 of the Prescription Drug User Fee Act, which allowed the FDA to collect fees from drug manufacturers to fund the new drug approval process. The average annual number of new drugs approved by the FDA during 1996–1999 was 67% higher than it was during 1985–1995 (Food and Drug Administration 2023b).
Community hospitals are defined as all nonfederal, short-term general, and other special hospitals. Other special hospitals include obstetrics and gynecology; eye, ear, nose, and throat; long term acute-care; rehabilitation; orthopedic; and other individually described specialty services. Community hospitals include academic medical centers or other teaching hospitals if they are nonfederal short-term hospitals. Excluded are hospitals not accessible by the general public, such as prison hospitals or college infirmaries.
When the 3 covariates are excluded from Eq. (3), all of the estimates of βk are negative but statistically insignificant.
Aggregate hospital charges were $1471 billion in 2014.
The National Health Expenditure Data includes a broader range of hospital services: physician and clinical services, prescription drugs, etc. It also includes a broader range of hospitals such as military, Veterans, Indian Health Services, etc.
References
Agency for Healthcare Research and Quality. (2023a). Clinical classifications software.
Agency for Healthcare Research and Quality. (2023b). Healthcare cost and utilization project (HCUPnet).
Alston, M., Dieguez, G., & Tomicki, S. (2018). A primer on prescription drug rebates: Insights into why rebates are a target for reducing prices. In: Milliman white paper. 21 May.
Baker, L., Birnbaum, H., Geppert, J., Mishol, D., & Moyneur, E. (2003). The relationship between technology availability and health care spending. Health Affairs, 22, 3–537.
Blankart, K. E., & Lichtenberg, F. R. (2022). The effects of off-label drug use on disability and medical expenditure. In: NBER working paper 30440. http://www.nber.org/papers/w30440
Bureau of Economic Analysis. (2023a). Health care.
Bureau of Economic Analysis. (2023b). Health care satellite account, more detailed blended data.
Bureau of Economic Analysis. (2023c). Health care satellite account, blended account, 2000–2020.
Cahan, E. M., Kocher, B., & Bohn, R. (2020). Why isn’t innovation helping reduce health care costs? Health Affairs Forefront, June 4.
Centers for Medicare and Medicaid Services. (2021). 2014 Part D rebate summary for all brand name drugs.
Centers for Medicare and Medicaid Services. (2023). National health expenditures by type of service and source of funds, CY 1960–2021.
Centre National Hospitalier d'Information sur le Médicament. (2023). Thériaque.
Congressional Budget Office. (2012). Offsetting effects of prescription drug use on Medicare’s spending for medical services, November 29.
Dorsey, E. R., de Roulet, J., Thompson, J. P., et al. (2010). Financial anatomy of biomedical research, 2003–2008. Journal of the American Medical Association, 303(2), 137–143.
Douguet, D. (2018). Data sets representative of the Structures and experimental properties of FDA-approved Drugs. ACS Medicinal Chemistry Letters, 9(3), 204–209.
Duflos, G., & Lichtenberg, F. R. (2012). Does competition stimulate drug utilization? The impact of changes in market structure on US drug prices, marketing and utilization. International Review of Law and Economics, 32(1), 95–109.
Dunn, A., Rittmueller, L., & Whitmire, B. (2015). Introducing the new health care satellite account, Bureau of economic analysis, January.
Dunn, A., Liebman, E. B., Shapiro, A. (2014). Developing a framework for decomposing medical care expenditure growth: Exploring issues of representativeness. In: D. W. Jorgenson, J. Steven Landefeld, and P. Schreyer (Eds.), Measuring economic sustainability and progress (pp. 545–574). Chicago: University of Chicago Press, for the National Bureau of Economic Research.
Dunn, A., Whitmire, B., Batch, A., Fernando, L., & Rittmueller, L. (2018). High spending growth rates for key diseases in 2000–14 Were driven by technology and demographic factors. Health Affairs, 37(6), 915–924.
Food and Drug Administration. (2023a). Drugs@FDA data files.
Food and Drug Administration. (2023b). Compilation of CDER NME and new biologic approvals 1985–2022.
Institut de Pharmacologie Moleculaire et Cellulaire. (2023). Cheminformatic tools and databases for pharmacology.
Lat, I., Micek, S., Janzen, J., Cohen, H., Olsen, K., & Haas, C. (2011). Off-label medication use in adult critical care patients. Journal of Critical Care, 26(1), 89–94. https://doi.org/10.1016/j.jcrc.2010.06.012
Lichtenberg, F. R. (2014). The impact of pharmaceutical innovation on disability days and the use of medical services in the United States, 1997–2010. Journal of Human Capital, 8(4), 432–480.
Lichtenberg, F. R. (2018). The impact of new drug launches on hospitalization in 2015 for 67 medical conditions in 15 OECD countries: A two-way fixed-effects analysis. Forum for Health Economics and Policy, 21(2).
Lichtenberg, F. R. (2021). Are drug prices subject to creative destruction? Evidence from the U.S., 1997–2017. Health Economics, 30(8), 1910–1932.
Lichtenberg, F. R. (2022a). The effects of dynamic and static competition on prescription drug prices in Denmark, 1997–2017. Journal of Evolutionary Economics, 32, 1155–1173.
Lichtenberg, F. R. (2022). The effect of pharmaceutical innovation on longevity: Evidence from the U.S. and 26 high-income countries. Economics and Human Biology, 46, 101124.
McKibbin, R. J. (2020). The effect of RCTs on demand for off-label cancer drugs. In SSRN scholarly paper ID 3574623. Rochester, NY: Social Science Research Network. https://doi.org/10.2139/ssrn.3574623
Radley, D. C., Finkelstein, S. N., & Stafford, R. S. (2006). Off-label prescribing among office-based physicians. Archives of Internal Medicine, 166(9), 1021–1026. https://doi.org/10.1001/archinte.166.9.1021
Research America. (2019). U.S. Investments in medical and health research and development 2013–2018.
Robinson, J. C., & Smith, M. D. (2008). Cost-reducing innovation in health care. Health Affairs, 27(5), 1353–1356.
Roebuck, M. C., Dougherty, J. S., Kaestner, R., & Miller, L. M. (2015). Increased use of prescription drugs reduces medical costs in Medicaid populations. Health Affairs, 34(9), 1586–1593.
Zhang, Y., Donohue, J. M., Lave, J. R., O’Donnell, G., & Newhouse, J. P. (2009). The effect of Medicare Part D on drug and medical spending. New England Journal of Medicine, 361(1), 52–61.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
I am grateful to Dominique Douguet of the Institut de Pharmacologie Moleculaire et Cellulaire for providing me with data from the e-Drug3D database, and to Stéphane Klegou of Centre National Hospitalier d'Information sur le Médicament for providing me with data from the Thériaque database.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lichtenberg, F.R. Has pharmaceutical innovation reduced the average cost of U.S. health care episodes?. Int J Health Econ Manag. 24, 1–31 (2024). https://doi.org/10.1007/s10754-023-09363-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10754-023-09363-y