Abstract
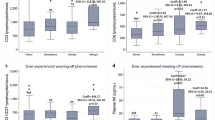
Idiopathic inflammatory myopathies (IIM) are a group of myopathies that present with muscle weakness and multiple extra-muscular manifestations, in which lymphocytes play central roles in myositis pathogenesis. This study aimed to explore the clinical characteristics of lymphocyte subsets, especially B cell subsets, in patients with IIM. Our study included 176 patients with active IIM and 210 gender/age-matched healthy controls (HCs). Compared to HCs, patients have reduced counts of T cells, B cells, and natural killer cells. In addition, B cell subsets from 153 patients with IIM and 92 HCs were characterized. Patients had a lower percentage of memory B cells and translational memory B cells, while those patients were with an elevated percentage of CD19+ B cells, plasmablast and naïve B cells compared with HCs. Moreover, to further explore the heterogeneity of B cells in IIM, patients were categorized into three clusters based on clustering analysis. Cluster 1 was dominated by CD19+ B cells, Bregs and naïve B cells, cluster 3 was dominated by memory B cells and plasmablast, and cluster 2 had the highest proportion of translational memory B cells. Notably, patients in cluster 1 presented with higher CK levels, indicating muscle damage, whereas patients in cluster 3 showed a higher incidence of chest tightness. Our study indicated that lymphopenia is a common manifestation in patients with IIM. B cell subsets are abnormally expressed and showed high heterogeneity in patients with IIM. The patients with IIM were divided into three different clusters with different percentages of chest tightness and distinct CK levels.





Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Lundberg, I.E., M. Fujimoto, J. Vencovsky, R. Aggarwal, M. Holmqvist, L. Christopher-Stine, A.L. Mammen, and F.W. Miller. 2021. Idiopathic inflammatory myopathies. Nature Reviews Disease Primers 7: 86. https://doi.org/10.1038/s41572-021-00321-x.
Ashton, C., S. Paramalingam, B. Stevenson, A. Brusch, and M. Needham. 2021. Idiopathic inflammatory myopathies: A review. Internal Medicine Journal 51: 845–852. https://doi.org/10.1111/imj.15358.
Aggarwal, R., C.V. Oddis, D. Goudeau, D. Koontz, Z. Qi, A.M. Reed, D.P. Ascherman, and M.C. Levesque. 2016. Autoantibody levels in myositis patients correlate with clinical response during B cell depletion with rituximab. Rheumatology 55: 991–999. https://doi.org/10.1093/rheumatology/kev444.
Ceribelli, A., M. De Santis, N. Isailovic, M.E. Gershwin, and C. Selmi. 2016. The immune response and the pathogenesis of idiopathic inflammatory myositis: a critical review. Clinical Reviews in Allergy & Immunology 52: 58–70. https://doi.org/10.1007/s12016-016-8527-x.
Greenberg, S.A., E.M. Bradshaw, J.L. Pinkus, G.S. Pinkus, T. Burleson, B. Due, L. Bregoli, K.C. O’Connor, and A.A. Amato. 2005. Plasma cells in muscle in inclusion body myositis and polymyositis. Neurology 65: 1782–1787. https://doi.org/10.1212/01.wnl.0000187124.92826.20.
Rayavarapu, S., W. Coley, T.B. Kinder, and K. Nagaraju. 2013. Idiopathic inflammatory myopathies: Pathogenic mechanisms of muscle weakness. Skeletal Muscle 3: 13. https://doi.org/10.1186/2044-5040-3-13.
Bradshaw, E.M., A. Orihuela, S.L. McArdel, M. Salajegheh, A.A. Amato, D.A. Hafler, S.A. Greenberg, and K.C. O’Connor. 2007. A local antigen-driven humoral response is present in the inflammatory myopathies. Journal of Immunology (Baltimore, Md. : 1950) 178: 547–556. https://doi.org/10.4049/jimmunol.178.1.547.
Li, W., X. Tian, X. Lu, Q. Peng, X. Shu, H. Yang, Y. Li, Y. Wang, X. Zhang, Q. Liu, et al. 2016. Significant decrease in peripheral regulatory B cells is an immunopathogenic feature of dermatomyositis. Scientific Reports 6: 27479. https://doi.org/10.1038/srep27479.
Mackay, F., P. Schneider, P. Rennert, and J. Browning. 2003. BAFF AND APRIL: A tutorial on B cell survival. Annual Review of Immunology 21: 231–264. https://doi.org/10.1146/annurev.immunol.21.120601.141152.
Nemazee, D. 2017. Mechanisms of central tolerance for B cells. Nature Reviews Immunology 17: 281–294. https://doi.org/10.1038/nri.2017.19.
Rosser Elizabeth, C., and C. Mauri. 2015. Regulatory B cells: origin, phenotype, and function. Immunity 42: 607–612. https://doi.org/10.1016/j.immuni.2015.04.005.
Glaros, V., R. Rauschmeier, A.V. Artemov, A. Reinhardt, S. Ols, A. Emmanouilidi, C. Gustafsson, Y. You, C. Mirabello, Å.K. Björklund, et al. 2021. Limited access to antigen drives generation of early B cell memory while restraining the plasmablast response. Immunity 54: 2005-2023.e2010. https://doi.org/10.1016/j.immuni.2021.08.017.
Jenks, S.A., C. Wei, R. Bugrovsky, A. Hill, X. Wang, F.M. Rossi, K. Cashman, M.C. Woodruff, L.D. Aspey, S.S. Lim, et al. 2021. B cell subset composition segments clinically and serologically distinct groups in chronic cutaneous lupus erythematosus. Annals of the Rheumatic Diseases 80: 1190–1200. https://doi.org/10.1136/annrheumdis-2021-220349.
Hu, F., W. Zhang, L. Shi, X. Liu, Y. Jia, L. Xu, H. Zhu, Y. Li, D. Xu, L. Lu, et al. 2018. Impaired CD27+IgD+ B cells with altered gene signature in rheumatoid arthritis. Frontiers In Immunology 9: 626. https://doi.org/10.3389/fimmu.2018.00626.
London, J., N. Dumoitier, S. Lofek, J. Dion, B. Chaigne, J. Mocek, N. Thieblemont, P. Cohen, C. Le Jeunne, L. Guillevin, et al. 2021. Skewed peripheral B- and T-cell compartments in patients with ANCA-associated vasculitis. Rheumatology (Oxford, England) 60: 2157–2168. https://doi.org/10.1093/rheumatology/keaa432.
Feng, R., J. Zhao, F. Sun, M. Miao, X. Sun, J. He, and Z. Li. 2022. Comparison of the deep immune profiling of B cell subsets between healthy adults and Sjögren’s syndrome. Annals of Medicine 54: 472–483. https://doi.org/10.1080/07853890.2022.2031272.
Young-Glazer, J., A. Cisneros, E.M. Wilfong, S.A. Smith, L.J. Crofford, and R.H. Bonami. 2021. Jo-1 autoantigen-specific B cells are skewed towards distinct functional B cell subsets in anti-synthetase syndrome patients. Arthritis Research & Therapy. https://doi.org/10.1186/s13075-020-02412-8.
Radke, J., R. Koll, C. Preuße, D. Pehl, K. Todorova, C. Schönemann, Y. Allenbach, E. Aronica, M. de Visser, F.L. Heppner, et al. 2018. Architectural B-cell organization in skeletal muscle identifies subtypes of dermatomyositis. Neurology - Neuroimmunology Neuroinflammation. https://doi.org/10.1212/nxi.0000000000000451.
Wang, Y., L. Zhu, B. Ju, J. Luo, Q. Li, X. Lv, D. Pu, Z. Hao, J. Wang, and L. He. 2022. Alterations of peripheral blood B cell subsets in Chinese patients with adult idiopathic inflammatory myopathies. Clinical and Experimental Rheumatology 40: 260–266. https://doi.org/10.55563/clinexprheumatol/ohsmuj.
Kikuchi, Y., S. Koarada, Y. Tada, O. Ushiyama, F. Morito, N. Suzuki, A. Ohta, T. Horiuchi, K. Miyake, and K. Nagasawa. 2001. Difference in B cell activation between dermatomyositis and polymyositis: Analysis of the expression of RP105 on peripheral blood B cells. Annals of the Rheumatic Diseases 60: 1137–1140. https://doi.org/10.1136/ard.60.12.1137.
Wilfong, E.M., T. Bartkowiak, K.N. Vowell, C.S. Westlake, J.M. Irish, P.L. Kendall, L.J. Crofford, and R.H. Bonami. 2022. High-dimensional analysis reveals distinct endotypes in patients with idiopathic inflammatory myopathies. Frontiers in Immunology 13: 756018. https://doi.org/10.3389/fimmu.2022.756018.
Bohan, A., and J.B. Peter. 1975. Polymyositis and dermatomyositis (first of two parts). The New England Journal of Medicine 292: 344–347. https://doi.org/10.1056/NEJM197502132920706.
Lundberg, I.E., A. Tjärnlund, M. Bottai, V.P. Werth, C. Pilkington, M. de Visser, L. Alfredsson, A.A. Amato, R.J. Barohn, M.H. Liang, et al. 2017. 2017 European League Against Rheumatism/American College of Rheumatology Classification Criteria for Adult and Juvenile Idiopathic Inflammatory Myopathies and Their Major Subgroups. Arthritis & Rheumatology (Hoboken, N.J.) 69: 2271–2282. https://doi.org/10.1002/art.40320.
Mammen, A.L., Y. Allenbach, W. Stenzel, and O. Benveniste. 2020. 239th ENMC International Workshop: Classification of dermatomyositis, Amsterdam, the Netherlands, 14–16 December 2018. Neuromuscular Disorders: NMD 30: 70–92. https://doi.org/10.1016/j.nmd.2019.10.005.
Connors, G.R., L. Christopher-Stine, C.V. Oddis, and S.K. Danoff. 2010. Interstitial lung disease associated with the idiopathic inflammatory myopathies: What progress has been made in the past 35 years? Chest 138: 1464–1474. https://doi.org/10.1378/chest.10-0180.
Isenberg, D.A., E. Allen, V. Farewell, M.R. Ehrenstein, M.G. Hanna, I.E. Lundberg, C. Oddis, C. Pilkington, P. Plotz, D. Scott, et al. 2004. International consensus outcome measures for patients with idiopathic inflammatory myopathies. Development and initial validation of myositis activity and damage indices in patients with adult onset disease. Rheumatology (Oxford, England) 43: 49–54. https://doi.org/10.1056/NEJM197502132920706.
Jin, Q., L. Fu, H. Yang, X. Chen, S. Lin, Z. Huang, B. Gao, X. Tian, W. Jiang, X. Shu, et al. 2023. Peripheral lymphocyte count defines the clinical phenotypes and prognosis in patients with anti-MDA5-positive dermatomyositis. Journal of Internal Medicine 293: 494–507. https://doi.org/10.1111/joim.13607.
Zuo, Y., L. Ye, F. Chen, Y. Shen, X. Lu, G. Wang, and X. Shu. 2022. Different multivariable risk factors for rapid progressive interstitial lung disease in Anti-MDA5 positive dermatomyositis and anti-synthetase syndrome. Frontiers In Immunology 13: 845988. https://doi.org/10.3389/fimmu.2022.845988.
Huang, W., F. Ren, L. Luo, J. Zhou, D. Huang, Z. Pan, and L. Tang. 2020. The characteristics of lymphocytes in patients positive for anti-MDA5 antibodies in interstitial lung disease. Rheumatology (Oxford, England) 59: 3886–3891. https://doi.org/10.1093/rheumatology/keaa266.
Ren, F.-P., Q. Chen, S.-S. Yao, L. Feng, X.-Y. Xue, W.-C. Zhao, D. Wang, Z.-L. Zhao, S.-W. Gu, T. Li, et al. 2023. Characteristics and prognostic implications of peripheral blood lymphocyte subsets in patients with anti-MDA5 antibody positive dermatomyositis-interstitial lung disease. BMC Pulmonary Medicine 23: 411. https://doi.org/10.1186/s12890-023-02706-y.
Lin, S., Y. Zhang, Z. Cao, Y. Xu, Q. Jin, X. Chen, X. Shu, X. Lu, G. Wang, and Q. Peng. 2023. Decrease in cell counts and alteration of phenotype characterize peripheral NK cells of patients with anti-MDA5-positive dermatomyositis. Clinica Chimica Acta; International Journal of Clinical Chemistry 543: 117321. https://doi.org/10.1016/j.cca.2023.117321.
Noyola, D.E., G. Juárez-Vega, C. Monjarás-Ávila, F. Escalante-Padrón, V. Rangel-Ramírez, S. Cadena-Mota, A. Monsiváis-Urenda, C.A. García-Sepúlveda, and R. González-Amaro. 2015. NK cell immunophenotypic and genotypic analysis of infants with severe respiratory syncytial virus infection. Microbiology and Immunology 59: 389–397. https://doi.org/10.1111/1348-0421.12265.
Sasaki, H., A. Takamura, K. Kawahata, T. Takashima, K. Imai, T. Morio, and H. Kohsaka. 2019. Peripheral blood lymphocyte subset repertoires are biased and reflect clinical features in patients with dermatomyositis. Scandinavian Journal of Rheumatology 48: 225–229. https://doi.org/10.1080/03009742.2018.1530371.
Dzangué-Tchoupou, G., Y. Allenbach, C. Preuße, W. Stenzel, and O. Benveniste. 2019. Mass cytometry reveals an impairment of B cell homeostasis in anti-synthetase syndrome. Journal of Neuroimmunology 332: 212–215. https://doi.org/10.1016/j.jneuroim.2019.04.014.
Glaros, V., R. Rauschmeier, A.V. Artemov, A. Reinhardt, S. Ols, A. Emmanouilidi, C. Gustafsson, Y. You, C. Mirabello, Å.K. Björklund, et al. 2021. Limited access to antigen drives generation of early B cell memory while restraining the plasmablast response. Immunity. https://doi.org/10.1016/j.immuni.2021.08.017.
Dörner, T., A.M. Jacobi, and P.E. Lipsky. 2009. B cells in autoimmunity. Arthritis Research & Therapy 11: 247. https://doi.org/10.1186/ar2780.
Pelzek, A.J., C. Grönwall, P. Rosenthal, J.D. Greenberg, M. McGeachy, L. Moreland, W.F.C. Rigby, and G.J. Silverman. 2017. Persistence of disease-associated anti-citrullinated protein antibody-expressing memory B Cells in rheumatoid arthritis in clinical remission. Arthritis & Rheumatology 69: 1176–1186. https://doi.org/10.1002/art.40053.
Sugimori, Y., Y. Iwasaki, Y. Takeshima, M. Okubo, S. Kobayashi, H. Hatano, S. Yamada, M. Nakano, R. Yoshida, M. Ota, et al. 2023. Transcriptome profiling of immune cell types in peripheral blood reveals common and specific pathways involved in the pathogenesis of myositis-specific antibody-positive inflammatory myopathies. ACR Open Rheumatology. https://doi.org/10.1002/acr2.11521.
Acknowledgements
We thank all the patients and healthy volunteers who participated in this study. We acknowledge assistance with the access of analytic instruments from Translational Medicine Center at The First Affiliated Hospital of Zhengzhou University.
Funding
This study was supported by the National Natural Science Foundation of China (82101889, 82302051, 82371819) and a Joint project of Medical Science and Technology Key Program of Henan Province (LHGJ20230175).
Author information
Authors and Affiliations
Contributions
Study design: ZP, ML, SL, and YZ. Patient enrollment and disease activity evaluation: PZ, SL, JL, TL and YZ. Sample collection: PZ, ML, YZ, RL, JL, TL, ZP, and SL. Sample processing and data analysis: ZP, ML, PZ, and YZ. Drafting of the article: ZP. Review and editing: PZ, YZ, RL, ML and SL. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Ethical Approval and Consent to Participate
The studies involving human participants were reviewed and approved by the Ethics Committee of the First Affiliated Hospital of Zhengzhou University. The patients/participants provided their written informed consent to participate in this study.
Consent to Publish
All patients and controls provided written informed consent.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pan, Z., Li, M., Zhang, P. et al. Peripheral Blood Lymphocyte Subsets and Heterogeneity of B Cell Subsets in Patients of Idiopathic Inflammatory Myositis with Different Myositis-specific Autoantibodies. Inflammation (2024). https://doi.org/10.1007/s10753-024-02052-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10753-024-02052-z