Abstract
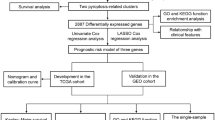
Pancreatic adenocarcinoma (PAAD) is a highly dangerous malignant tumor of the digestive tract, and difficult to diagnose, treat, and predict the prognosis. As we all know, tumor and inflammation can affect each other, and thus the inflammatory response in the microenvironment can be used to affect the prognosis. So far, the prognostic value of inflammatory response-related genes in PAAD is still unclear. Therefore, this study aimed to explore the inflammatory response-related genes for predicting the prognosis of PAAD. In this study, the mRNA expression profiles of PAAD patients and the corresponding clinical characteristics data of PAAD patients were downloaded from the public database. The least absolute shrinkage and selection operator (LASSO) Cox analysis model was used to identify and construct the prognostic gene signature in The Cancer Genome Atlas (TCGA) cohort. The PAAD patients used for verification are from the International Cancer Genome Consortium (ICGC) cohort. The Kaplan–Meier method was used to compare the overall survival (OS) between the high- and low-risk groups. Univariate and multivariate Cox analyses were performed to identify the independent predictors of OS. Gene set enrichment analysis (GSEA) was performed to obtain gene ontology (GO) terms and the Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways, and the correlation between gene expression and immune infiltrates was investigated via single sample gene set enrichment analysis (ssGSEA). The GEPIA database was performed to examine prognostic genes in PAAD. LASSO Cox regression analysis was used to construct a model of inflammatory response-related gene signature. Compared with the low-risk group, patients in the high-risk group had significantly lower OS. The receiver operating characteristic curve (ROC) analysis confirmed the signature’s predictive capacity. Multivariate Cox analysis showed that risk score is an independent predictor of OS. Functional analysis shows that the immune status between the two risk groups is significantly different, and the cancer-related pathways were abundant in the high-risk group. Moreover, the risk score is significantly related to tumor grade, stage, and immune infiltration types. It was also obtained that the expression level of prognostic genes was significantly correlated with the sensitivity of cancer cells to anti-tumor drugs. In addition, there are significant differences in the expression of PAAD tissues and adjacent non-tumor tissues. The novel signature constructed from five inflammatory response-related genes can be used to predict prognosis and affect the immune status of PAAD. In addition, suppressing these genes may be a treatment option.










Similar content being viewed by others
DATA AVAILABILITY
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- PAAD:
-
Pancreatic adenocarcinoma
- TCGA:
-
The Cancer Genome Atlas
- ICGC:
-
International Cancer Genome Consortium
- DEGs:
-
Differentially expressed genes
- BH:
-
Benjamini–Hochberg
- PCA:
-
Principal component analysis
- ROC:
-
Receiver operating characteristic
- KEGG:
-
Kyoto Encyclopedia of Genes and Genomes
- GSEA:
-
Gene set enrichment analysis
- GO:
-
Gene ontology
- ssGSEA:
-
Single-sample gene set enrichment analysis
- ANOVA:
-
Analysis of variance
- NCI:
-
National Cancer Institute
- AUC:
-
Area under the curve
- aDCs:
-
A dendritic cells
- Treg:
-
Regulatory T cells
- APC:
-
Antigen-presenting cells
- MHC:
-
Major histocompatibility complex
- HLA:
-
Human leukocyte antigen
- CCR:
-
Carbon catabolite repression
- TME:
-
Tumor microenvironment
- mDNAsi:
-
Stemness index
- DNAss:
-
DNA stemness score
- RNAss:
-
RNA stemness score
- IFN-γ:
-
Interferon-γ
References
Xu, T., X. Xu, P.C. Liu, H. Mao, and S. Ju. 2020. Transcriptomic analyses and potential therapeutic targets of pancreatic cancer with concomitant diabetes. Frontiers in Oncology 10: 563527. https://doi.org/10.3389/fonc.2020.563527.
Li, B., C. Zhang, J. Wang, M. Zhang, C. Liu, and Z. Chen. 2020. Impact of genetic variants of ABCB1, APOB, CAV1, and NAMPT on susceptibility to pancreatic ductal adenocarcinoma in Chinese patients. Molecular Genetics & Genomic Medicine 8: e1226. https://doi.org/10.1002/mgg3.1226.
Chen, J.X., C.S. Cheng, H.F. Gao, Z.J. Chen, L.L. Lv, J.Y. Xu, X.H. Shen, J. Xie, and L. Zheng. 2021. Overexpression of interferon-inducible protein 16 promotes progression of human pancreatic adenocarcinoma through interleukin-1β-induced tumor-associated macrophage infiltration in the tumor microenvironment. Frontiers in Cell and Developmental Biology 9:640786. https://doi.org/10.3389/fcell.2021.640786.
Okamoto, H., H. Kikuchi, H. Naganuma, and T. Kamei. 2020. Multiple carcinosarcomas of the esophagus with adeno-carcinomatous components: A case report. World Journal of Gastroenterology 26: 2111–2118. https://doi.org/10.3748/wjg.v26.i17.2111.
Setrerrahmane, S., and H. Xu. 2017. Tumor-related interleukins: Old validated targets for new anti-cancer drug development. Molecular Cancer 16: 153. https://doi.org/10.1186/s12943-017-0721-9.
Balkwill, F., and A. Mantovani. 2001. Inflammation and cancer: Back to Virchow? Lancet 357: 539–545. https://doi.org/10.1016/S0140-6736(00)04046-0.
Maruyama, T., T. Tomofuji, T. Machida, H. Kato, K. Tsutsumi, D. Uchida, A. Takaki, T. Yoneda, H. Miyai, H. Mizuno, D. Ekuni, H. Okada, and M. Morita. 2017. Association between periodontitis and prognosis of pancreatobiliary tract cancer: A pilot study. Molecular and Clinical Oncology 6: 683–687. https://doi.org/10.3892/mco.2017.1220.
Hurley, D.G., D.M. Budden, and E.J. Crampin. 2015. Virtual reference environments: A simple way to make research reproducible. Briefings in Bioinformatics 16: 901–903. https://doi.org/10.1093/bib/bbu043.
Benjamini, Y., and Y. Hochberg. 1995. Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B (Methodological). 57: 289–300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x.
Sun, H., and S. Wang. 2012. Penalized logistic regression for high-dimensional DNA methylation data with case-control studies. Bioinformatics 28: 1368–1375. https://doi.org/10.1093/bioinformatics/bts145.
Flobak, Å., B. Niederdorfer, V.T. Nakstad, L. Thommesen, G. Klinkenberg, and A. Lægreid. 2019. A high-throughput drug combination screen of targeted small molecule inhibitors in cancer cell lines. Scientific Data 6: 237. https://doi.org/10.1038/s41597-019-0255-7.
Ji, X., F. Ding, J. Gao, X. Huang, W. Liu, Y. Wang, Q. Liu, and T. Xin. 2020. Molecular and clinical characterization of a novel prognostic and immunologic biomarker FAM111A in diffuse lower-grade glioma. Frontiers in Oncology 10: 573800. https://doi.org/10.3389/fonc.2020.573800.
Chao, B., X. Ju, L. Zhang, X. Xu, and Y. Zhao. 2020. A novel prognostic marker systemic inflammation response index (SIRI) for operable cervical cancer patients. Frontiers in Oncology 10: 766. https://doi.org/10.3389/fonc.2020.00766.
Hsu, B.E., Y. Shen, and P.M. Siegel. 2020. Neutrophils: Orchestrators of the malignant phenotype. Frontiers in Immunology 11: 1778. https://doi.org/10.3389/fimmu.2020.01778.
Yang, C.C., L.D. Hsiao, and C.M. Yang. 2020. Galangin inhibits LPS-induced MMP-9 expression via suppressing protein kinase-dependent AP-1 and FoxO1 activation in rat brain astrocytes. Journal of Inflammation Research 13: 945–960. https://doi.org/10.2147/JIR.S276925.
Hoffmann, T.K., G. Dworacki, T. Tsukihiro, N. Meidenbauer, W. Gooding, J.T. Johnson, and T.L. Whiteside. 2002. Spontaneous apoptosis of circulating T lymphocytes in patients with head and neck cancer and its clinical importance. Clinical Cancer Research 8: 2553–2562.
Iwai, N., T. Okuda, J. Sakagami, T. Harada, T. Ohara, M. Taniguchi, H. Sakai, K. Oka, T. Hara, T. Tsuji, T. Komaki, K. Kagawa, H. Yasuda, Y. Naito, and Y. Itoh. 2020. Neutrophil to lymphocyte ratio predicts prognosis in unresectable pancreatic cancer. Science and Reports 10: 18758. https://doi.org/10.1038/s41598-020-75745-8.
Liu, Z., W. Liang, D. Kang, Q. Chen, Z. Ouyang, H. Yan, B. Huang, D. Jin, Y. Chen, and Q. Li. 2020. Increased osteoblastic Cxcl9 contributes to the uncoupled bone formation and resorption in postmenopausal osteoporosis. Clinical Interventions in Aging 15: 1201–1212. https://doi.org/10.2147/CIA.S254885.
Wang, Y., X. Wang, X. Huang, J. Zhang, J. Hu, Y. Qi, B. Xiang, and Q. Wang. 2021. Integrated genomic and transcriptomic analysis reveals key genes for predicting dual-phenotype hepatocellular carcinoma prognosis. Journal of Cancer 12: 2993–3010. https://doi.org/10.7150/jca.56005.
Pein, M., J. Insua-Rodríguez, T. Hongu, A. Riedel, J. Meier, L. Wiedmann, K. Decker, M.A.G. Essers, H.P. Sinn, S. Spaich, M. Sütterlin, A. Schneeweiss, A. Trumpp, and T. Oskarsson. 2020. Metastasis-initiating cells induce and exploit a fibroblast niche to fuel malignant colonization of the lungs. Nature Communications 11: 1494. https://doi.org/10.1038/s41467-020-15188-x.
Kuo, P., Z.K. Tuong, S.M. Teoh, I.H. Frazer, S.R. Mattarollo, and G.R. Leggatt. 2018. HPV16E7-induced hyperplasia promotes CXCL9/10 expression and induces CXCR3+ T-cell migration to skin. The Journal of Investigative Dermatology 138: 1348–1359. https://doi.org/10.1016/j.jid.2017.12.021.
Matsumoto, M., H. Oshiumi, and T. Seya. 2011. Antiviral responses induced by the TLR3 pathway. Reviews in Medical Virology 21: 67–77. https://doi.org/10.1002/rmv.680.
Meng, Q., and B. Qiu. 2020. Exosomal MicroRNA-320a derived from mesenchymal stem cells regulates rheumatoid arthritis fibroblast-like synoviocyte activation by suppressing CXCL9 expression. Frontiers in Physiology 11: 441. https://doi.org/10.3389/fphys.2020.00441.
Kotrych, D., V. Dziedziejko, K. Safranow, and A. Pawlik. 2015. Lack of association between CXCL9 and CXCL10 gene polymorphisms and the outcome of rheumatoid arthritis treatment with methotrexate. European Review for Medical and Pharmacological Sciences 19: 3037–3040.
Hasegawa, T., V. Venkata Suresh, Y. Yahata, M. Nakano, S. Suzuki, S. Suzuki, S. Yamada, H. Kitaura, I. Mizoguchi, Y. Noiri, K. Handa, and M. Saito. 2021. Inhibition of the CXCL9-CXCR3 axis suppresses the progression of experimental apical periodontitis by blocking macrophage migration and activation. Science and Reports 11: 2613. https://doi.org/10.1038/s41598-021-82167-7.
Corrales, L., V. Matson, B. Flood, S. Spranger, and T.F. Gajewski. 2017. Innate immune signaling and regulation in cancer immunotherapy. Cell Research 27: 96–108. https://doi.org/10.1038/cr.2016.149.
Aguilera-Durán, G., and A. Romo-Mancillas. 2020. Computational study of C-X-C chemokine receptor (CXCR)3 binding with its natural agonists chemokine (C-X-C Motif) ligand (CXCL) 9, 10 and 11 and with synthetic antagonists: Insights of receptor activation towards drug design for vitiligo. Molecules 25: 4413. https://doi.org/10.3390/molecules25194413.
Akkari, L., V. Gocheva, J.C. Kester, K.E. Hunter, M.L. Quick, L. Sevenich, H.W. Wang, C. Peters, L.H. Tang, D.S. Klimstra, T. Reinheckel, and J.A. Joyce. 2014. Distinct functions of macrophage-derived and cancer cell-derived cathepsin Z combine to promote tumor malignancy via interactions with the extracellular matrix. Genes & Development 28: 2134–2150. https://doi.org/10.1101/gad.249599.114.
Li, X., M.J. Large, C.J. Creighton, R.B. Lanz, J.W. Jeong, S.L. Young, B.A. Lessey, W.A. Palomino, S.Y. Tsai, and F.J. Demayo. 2013. COUP-TFII regulates human endometrial stromal genes involved in inflammation. Molecular Endocrinology 27: 2041–2054. https://doi.org/10.1210/me.2013-1191.
Chen, P.H., H. Yao, and L.J. Huang. 2017. Cytokine receptor endocytosis: New kinase activity-dependent and -independent roles of PI3K. Frontiers in Endocrinology (Lausanne) 8: 78. https://doi.org/10.3389/fendo.2017.00078.
Maas, N.L., and J.A. Diehl. 2015. Molecular pathways: The PERKs and pitfalls of targeting the unfolded protein response in cancer. Clinical Cancer Research 21 (4): 675–679. https://doi.org/10.1158/1078-0432.CCR-13-3239.
Nagelkerke, A., H. Mujcic, J. Bussink, B.G. Wouters, H.W. van Laarhoven, F.C. Sweep, and P.N. Span. 2011. Hypoxic regulation and prognostic value of LAMP3 expression in breast cancer. Cancer 117: 3670–3681. https://doi.org/10.1002/cncr.25938.
Liu, S., J. Yue, W. Du, J. Han, and W. Zhang. 2018. LAMP3 plays an oncogenic role in osteosarcoma cells partially by inhibiting TP53. Cellular & Molecular Biology Letters 11 (23): 33. https://doi.org/10.1186/s11658-018-0099-8. PMID:30008754;PMCID:PMC6042264
Liao, X., Y. Chen, D. Liu, F. Li, X. Li, and W. Jia. 2015. High expression of LAMP3 is a novel biomarker of poor prognosis in patients with esophageal squamous cell carcinoma. International Journal of Molecular Sciences 16: 17655–17667. https://doi.org/10.3390/ijms160817655.
Kanao, H., T. Enomoto, T. Kimura, M. Fujita, R. Nakashima, Y. Ueda, Y. Ueno, T. Miyatake, T. Yoshizaki, G.S. Buzard, A. Tanigami, K. Yoshino, and Y. Murata. 2005. Overexpression of LAMP3/TSC403/DC-LAMP promotes metastasis in uterine cervical cancer. Cancer Research 65: 8640–8645. https://doi.org/10.1158/0008-5472.CAN-04-4112.
Liu, K., Q. He, G. Liao, and J. Han. 2015. Identification of critical genes and gene interaction networks that mediate osteosarcoma metastasis to the lungs. Experimental and Therapeutic Medicine 10: 1796–1806. https://doi.org/10.3892/etm.2015.2767.
Kosti, A., P.R. de Araujo, W.Q. Li, G.D.A. Guardia, J. Chiou, C. Yi, D. Ray, F. Meliso, Y.M. Li, T. Delambre, M. Qiao, S.S. Burns, F.K. Lorbeer, F. Georgi, M. Flosbach, S. Klinnert, A. Jenseit, X. Lei, C.R. Sandoval, K. Ha, H. Zheng, R. Pandey, A. Gruslova, Y.K. Gupta, A. Brenner, E. Kokovay, T.R. Hughes, Q.D. Morris, P.A.F. Galante, S. Tiziani, and L.O.F. Penalva. 2020. The RNA-binding protein SERBP1 functions as a novel oncogenic factor in glioblastoma by bridging cancer metabolism and epigenetic regulation. Genome Biology 21: 195. https://doi.org/10.1186/s13059-020-02115-y.
Alessandrini, F., L. Pezzè, D. Menendez, M.A. Resnick, and Y. Ciribilli. 2018. ETV7-mediated DNAJC15 repression leads to doxorubicin resistance in breast cancer cells. Neoplasia 20: 857–870. https://doi.org/10.1016/j.neo.2018.06.008.
Wang, C., B. Qi, C. Zhang, and J. Cheng. 2017. Identification of key genes influenced by fixation stability in early fracture hematoma and elucidation of their roles in fracture healing. Experimental and Therapeutic Medicine 14: 4633–4638. https://doi.org/10.3892/etm.2017.5192.
Hundsdorfer, B., H.F. Zeilhofer, K.P. Bock, P. Dettmar, M. Schmitt, and H.H. Horch. 2004. Prognostische Bedeutung des Plasminogenaktivators vom Urokinasetyp (uPA) und des Plasminogenaktivator-Inhibitors (PAI-1) beim primär resezierten Plattenepithelkarzinom der Mundhöhle [The prognostic importance of urinase type plasminogen activators (uPA) and plasminogen activator inhibitors (PAI-1) in the primary resection of oral squamous cell carcinoma]. Mund Kiefer Gesichtschir 8:173–179. German. https://doi.org/10.1007/s10006-003-0520-x.
Annecke, K., M. Schmitt, U. Euler, M. Zerm, D. Paepke, S. Paepke, G. von Minckwitz, C. Thomssen, and N. Harbeck. 2008. uPA and PAI-1 in breast cancer: Review of their clinical utility and current validation in the prospective NNBC-3 trial. Advances in Clinical Chemistry 45: 31–45. https://doi.org/10.1016/s0065-2423(07)00002-9.
Harbeck, N., M. Schmitt, S. Paepke, H. Allgayer, and R.E. Kates. 2007. Tumor-associated proteolytic factors uPA and PAI-1: Critical appraisal of their clinical relevance in breast cancer and their integration into decision-support algorithms. Critical Reviews in Clinical Laboratory Sciences 44: 179–201. https://doi.org/10.1080/10408360601040970.
Cariello, M., E. Piccinin, R. Zerlotin, M. Piglionica, C. Peres, C. Divella, A. Signorile, G. Villani, G. Ingravallo, C. Sabbà, and A. Moschetta. 2021. Adhesion of platelets to colon cancer cells is necessary to promote tumor development in xenograft, genetic and inflammation models. Cancers (Basel) 13: 4243. https://doi.org/10.3390/cancers13164243.
Koltsova, E.K., P. Sundd, A. Zarpellon, H. Ouyang, Z. Mikulski, A. Zampolli, Z.M. Ruggeri, and K. Ley. 2014. Genetic deletion of platelet glycoprotein Ib alpha but not its extracellular domain protects from atherosclerosis. Thrombosisa and Haemostasis 112(6):1252–63. https://doi.org/10.1160/TH14-02-0130. Epub 2014 Aug 7. PMID: 25104056; PMCID: PMC4429870.
Song, Y., J.A. Aglipay, J.D. Bernstein, S. Goswami, and P. Stanley. 2010. The bisecting GlcNAc on N-glycans inhibits growth factor signaling and retards mammary tumor progression. Cancer Research 70 (8): 3361–3371. https://doi.org/10.1158/0008-5472. CAN-09-2719.PMID:20395209;PMCID:PMC2856092
Zhang, X., W. Chen, N. Yin, L. Dong, M. Fu, Q. Zhan, and T. Tong. 2019. Regulation of OLC1 protein expression by the anaphase-promoting complex. Oncology Letters 17: 2639–2646. https://doi.org/10.3892/ol.2019.9881.
Zhang, E., and Y. Wu. 2014. Dual effects of miR-155 on macrophages at different stages of atherosclerosis: LDL is the key? Medical Hypotheses 83: 74–78. https://doi.org/10.1016/j.mehy.2014.04.004.
Horiguchi, S., H. Shiraha, T. Nagahara, J. Kataoka, M. Iwamuro, M. Matsubara, S. Nishina, H. Kato, A. Takaki, K. Nouso, T. Tanaka, K. Ichimura, T. Yagi, and K. Yamamoto. 2013. Loss of runt-related transcription factor 3 induces gemcitabine resistance in pancreatic cancer. Molecular Oncology 7: 840–849. https://doi.org/10.1016/j.molonc.2013.04.004.
Tekin, C., H.L. Aberson, C. Waasdorp, G.K.J. Hooijer, O.J. de Boer, F. Dijk, M.F. Bijlsma, and C.A. Spek. 2020. Macrophage-secreted MMP9 induces mesenchymal transition in pancreatic cancer cells via PAR1 activation. Cellular Oncology (Dordrecht) 43: 1161–1174. https://doi.org/10.1007/s13402-020-00549-x.
García-Sáenz, M., D. Uribe-Cortés, C. Ramírez-Rentería, and A. Ferreira-Hermosillo. 2018. Difficult-to-diagnose diabetes in a patient treated with cyclophosphamide - the contradictory roles of immunosuppressant agents: A case report. Journal of Medical Case Reports 12 (1): 364. https://doi.org/10.1186/s13256-018-1925-3. PMID:30526658;PMCID:PMC6287356.
Gelsomino, L., G.D. Naimo, R. Malivindi, G. Augimeri, S. Panza, C. Giordano, I. Barone, D. Bonofiglio, L. Mauro, S. Catalano, and S. Andò. 2020. Knockdown of leptin receptor affects macrophage phenotype in the tumor microenvironment inhibiting breast cancer growth and progression. Cancers (Basel) 12: 2078. https://doi.org/10.3390/cancers12082078.
Zhang, L., H. Liang, H. Guan, and H. Liu. 2015. Study of the association between CD28/CTLA-4 expression and disease activity in juvenile idiopathic arthritis. Experimental and Therapeutic Medicine 9: 1733–1738. https://doi.org/10.3892/etm.2015.2295.
Sabanathan, D., J.J. Park, M. Marquez, L. Francisco, N. Byrne, and H. Gurney. 2017. Cure in advanced renal cell cancer: Is it an achievable goal? The Oncologist 22: 1470–1477. https://doi.org/10.1634/theoncologist.2017-0159.
Smith, M.A., C.C. Chiang, K. Zerrouki, S. Rahman, W.I. White, K. Streicher, W.A. Rees, A. Schiffenbauer, L.G. Rider, F.W. Miller, Z. Manna, S. Hasni, M.J. Kaplan, R. Siegel, D. Sinibaldi, M.A. Sanjuan, and K.A. Casey. 2020. Using the circulating proteome to assess type I interferon activity in systemic lupus erythematosus. Science and Reports 10: 4462. https://doi.org/10.1038/s41598-020-60563-9.
Brunel, A., G. Bégaud, C. Auger, S. Durand, S. Battu, B. Bessette, and M. Verdier. 2021. Autophagy and extracellular vesicles, connected to rabGTPase family, support aggressiveness in cancer stem cells. Cells 10: 1330. https://doi.org/10.3390/cells10061330.
Almahmoud, S., and H.A. Zhong. 2019. Molecular modeling studies on the binding mode of the PD-1/PD-L1 Complex Inhibitors. International Journal of Molecular Sciences 20: 4654. https://doi.org/10.3390/ijms20184654.
ACKNOWLEDGEMENTS
Acknowledgments to the TCGA and ICGC databases for providing researchable patient data.
Funding
This study was supported by (1) Key Laboratory of Tumor Precision Medicine, Hunan Colleges and Universities Project (2019–379), (2) a project supported by Scientific Research Fund of Hunan Provincial Education Department (19a458), and (3) Scientific Research Project of Hunan Provincial Health Commission (20201718).
Author information
Authors and Affiliations
Contributions
Zu-Liang Deng, Ding-Zhong Zhou, Su-Juan Cao, and Hui Xie: substantial contributions to the conception and design of the work; Zu-Liang Deng, Ding-Zhong Zhou, Su-Juan Cao, Qing Li, Jian-Fang Zhang, and Hui Xie: the acquisition, analysis, and interpretation of data for the work; Zu-Liang Deng, Ding-Zhong Zhou, and Su-Juan Cao: drafting the work; Hui Xie: revising it critically for important intellectual content; Zu-Liang Deng, Ding-Zhong Zhou, Su-Juan Cao, Qing Li, Jian-Fang Zhang, and Hui Xie: final approval of the version to be published; Zu-Liang Deng, Ding-Zhong Zhou, Su-Juan Cao, Qing Li, Jian-Fang Zhang, and Hui Xie: agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
N/A.
Consent for Publication
N/A.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Deng, ZL., Zhou, DZ., Cao, SJ. et al. Development and Validation of an Inflammatory Response-Related Gene Signature for Predicting the Prognosis of Pancreatic Adenocarcinoma. Inflammation 45, 1732–1751 (2022). https://doi.org/10.1007/s10753-022-01657-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10753-022-01657-6