Abstract
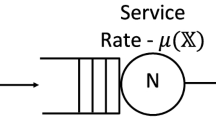
The stochastic nature of both patient arrivals and lengths of stay leads inevitably to periodic bed shortages in healthcare units. Physicians are challenged to fit demand to service capacity. If all beds are occupied eligible patients are usually referred to another ward or hospital and scheduled surgeries may be cancelled. Lack of beds may also have consequences for patients, who may be discharged in advance when the number of occupied beds is so high as to compromise the medical care of new incoming patients. In this paper we deal with the problem of obtaining efficient bed-management policies. We introduce a queuing control problem in which neither the arrival rates nor the number of servers can be modified. Bed occupancy control is addressed by modifying the service time rates, to make them dependent on the state of the system. The objective functions are two quality-of-service components: to minimize patient rejections and to minimize the length of stay shortening. The first objective has a clear mathematical formulation: minimize the probability of rejecting a patient. The second objective admits several formulations. Four different expressions, all leading to nonlinear optimization problems, are proposed. The solutions of these optimization problems define different control policies. We obtain the analytical solutions by adopting Markov-type assumptions and comparing them in terms of the two quality-of-service components. We extend these results to the general case using optimization with simulation, and propose a way to simulate general length of stay distributions enabling the inclusion of state-dependent service rates.





Similar content being viewed by others
References
Ahmed MA, Alkhamis TM (2009) Simulation optimization for an emergency department healthcare unit in Kuwait. Eur J Oper Res 198:936–942
Anderson D, Price C, Golden B, Jank G, Wasil E (2011) Examining the discharge practices of surgeons at a large medical center. Health Care Manag Sci 14:338–347
Azcárate C, Mallor F, Gafaro A (2008) Multiobjective optimization in health care management. A metaheuristic and simulation approach. Algorithm Oper Res 3:186–202
Bowers J (2013) Balancing operating theatre and bed capacity in a cardiothoracic centre. Health Care Manag Sci. doi:10.1007/s10729-013-9221-7
Brailsford SC, Gutjahr W, Rauner MS, Zeppelzauer W (2007) Optimal screen policies for diabetic retinopathy using a new combined discrete event simulation and ant colony optimization approach. Comput Manag Sci 4:59–83
Brailsford SC, Harper PR, Patel B, Pidd M (2009) An analysis of the academic literature on simulation and modelling in health care. J Simul 3:130–140
Capuzzo M, Moreno RP, Alvisi R (2010) Admission and discharge of critically ill patients. Curr Opin Crit Care 16:499–504
Chan CW, Farias VF, Bambos N, Escobar G (2012) Optimizing intensive care unit discharge decisions with patient readmissions. Oper Res 60:1323–1341
Chan CW, Yom-Tov G, Escobar G (2014) When to use speedup: an examination of service systems with return. Oper Res 62:462–482
Cochran JK, Roche K (2008) A queuing-based decision support methodology to estimate hospital inpatient bed demand. J Oper Res Soc 59:1471–1482
Costa AX, Ridley SA, Shahani AK, Harper PR, De Senna V, Nielsen MS (2003) Mathematical modelling and simulation for planning critical care capacity. Anaesthesia 58:320–327
de Angelis V, Felici G, Impelluso P (2003) Integrating simulation and optimisation in health care center management. Eur J Oper Res 50:101–114
de Bruin AM, van Rossum AC, Viseer MC, Koole GM (2007) Modeling the emergency cardiac in-patient flow: an application of queuing theory. Health Care Manag Sci 10:125–137
de Bruin AM, Bekker R, van Zanten L, Koole GM (2010) Dimensioning hospital wards using the Erlang loss model. Ann Oper Res 178:23–43
Eldabi T, Paul RJ, Young T (2007) Simulation modelling in healthcare: reviewing legacies and investigating futures. J Oper Res Soc 58:262–270
Fu MC, Glover FW, April J (2005) Simulation optimization: a review, new developments and applications. In: Proceedings of the 2005 winter simulation conference, pp 83–95
Green LV (2002) How many hospital beds? Inquiry 39:400–412
Griffiths JD, Price-Lloyd N, Smithies M, Williams JE (2005) Modelling the requirement for supplementary nurses in an intensive care unit. J Oper Res Soc 56:126–133
Griffiths JD, Price-Lloyd N, Smithies M, Williams J (2006) A queueing model of activities in an intensive care unit. IMA J Manag Math 17:277–288
Griffiths JD, Knight V, Komenda I (2013) Bed management in a critical care unit. IMA J Manag Math 24:137–153
Gross D, Harris CM (2008) Fundamentals of queueing theory. Wiley, New York
Günal MM, Pidd M (2010) Discrete event simulation for the performance modelling in health care: a review of the literature. J Simul 4:42–51
Katsaliaki K, Mustafee N (2011) Applications of simulation within the healthcare context. J Oper Res Soc 62:1431–1451
Kc D, Terwiesch C (2009) Impact of workload on service time and patient safety: and econometric analysis of hospital operations. Manag Sci 55:1486–1498
Kim SC, Horowitz I, Young K, Buckley TA (1999) Analysis of capacity management of the intensive care unit in a hospital. Eur J Oper Res 115:36–46
Kim SC, Horowitz I, Young K, Buckley TA (2000) Flexible bed allocation and performance in the intensive care unit. J Oper Manag 18:427–443
Kolker A (2009) Process modeling of ICU patient flow: effect of daily load leveling of elective surgeries on ICU diversion. J Med Syst 33:27–40
Lakshmi C, Sivakumar A (2013) Application of queueing theory in health care: A literature review. Operations Research for Health Care 2:25–39
Leleu H, Moises J, Valdmanis V (2012) Optimal productive size of hospital’s intensive care units. Int J Prod Econ 136:297–305
Lin RC, Sir M, Pasupathy KS (2013) Multi-objective simulation optimization using data envelopment analysis and genetic algorithm: specific application to determining optimal resource levels in surgical services. Omega 41:881–892
Litvak N, van Rijsbergen M, Boucherie RJ, van Houdenhoven M (2008) Managing the overflow of intensive care patients. Eur J Oper Res 185:998–1010
Mallor F, Azcárate C (2014) Combining optimization with simulation to obtain credible models for intensive care units. Ann Oper Res 221:255–271
Marshall A, Vasilakis C, El-Zardi E (2005) Length of stay-based patient flow models: recent developments and future directions. Health Care Manag Sci 8:213–220
Masterson BJ, Mihara TG, Miller G, Randolph SC, Forkner E, Crouter AL (2004) Using models and data to support optimization of the military health system: a case study in an intensive care unit. Health Care Manag Sci 7:217–224
McManus ML, Long MC, Cooper A, Litvak E (2004) Queueing theory accurately models the need for critical care resources. Anesthesiology 100:1271–1276
Rauner MS, Zeiles A, Schaffhauser-Linzattti MM, Hornik K (2003) Modelling the effects of the Austrian inpatient reimbursement system on length-of-stay distributions. OR Spectrum 25:183–206
Ridge JC, Jones SK, Nielsen MS, Shahani AK (1998) Capacity planning for intensive care units. Eur J Oper Res 105:346–355
Shmueli A, Sprug CL, Kaplan E (2003) Optimizing admissions to an intensive care unit. Health Care Manag Sci 6:131–136
Sinuff T, Kahnamoui K, Cook DJ et al (2004) Rationing critical care beds: a systematic review. Crit Care Med 32:1588–1597
Stidham S (2002) Analysis, design and control of queueing systems. Oper Res 50:197–216
Terekhov D, Beck JC (2008) A constraint programming approach for solving a queueing control problem. J Art Int Res 32:123–167
Troy PM, Rosenberg L (2009) Using simulation to determine the need for ICU beds for surgery patients. Surgery 146:608–617
Vallentin A, Ferdinandi P (2011) Recommendations on basic requirements for intensive care units: structural and organizational aspects. Intensive Care Med. doi:10.1007/s00134-011-2300-7
Vasilakis C, Marshall AH (2005) Modelling nationwide hospital length of stay: opening the black box. J Oper Res Soc 56:862–869
Zhu Z, Hen BH, Teow KL (2012) Estimating ICU bed capacity using discrete event simulation. International Journal of Health Care Quality Assurance 25:134–144
Zimmerman JE, Kramer AA, McNair DS, Malila FM, Shaffer VL (2006) Intensive care unit length of stay: benchmarking based on acute physiology and chronic health evaluation (APACHE) IV. Crit Care Med 34:2517–2529
Acknowledgments
This paper has been in part supported by Grant MTM2012-36025.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mallor, F., Azcárate, C. & Barado, J. Control problems and management policies in health systems: application to intensive care units. Flex Serv Manuf J 28, 62–89 (2016). https://doi.org/10.1007/s10696-014-9209-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10696-014-9209-8