Avoid common mistakes on your manuscript.
Introduction
Gastroenterology (GI) fellows are equipped during training with the knowledge of when more permanent routes of enteral feeding are indicated and how to place percutaneous endoscopic gastrostomy (PEG) tubes. Though there are prior reviews and guides [1] to assist GI fellows further in the logistics of this procedure, many practical questions arise regarding PEG tubes from patients and their healthcare teams for which clear evidence-based answers are more difficult to locate. In particular, GI fellows are less likely to learn about the management and removal of gastrostomy tubes than they are about their insertion.
This guide was created to help GI fellows more confidently and efficiently answer commonly asked questions from patients, families, and healthcare team members regarding the management and removal of PEG tubes. We end with suggestions for improvements in clinical documentation, patient education, and interdisciplinary communication that can help reduce confusion regarding PEG tube insertion and management.
The following are examples of questions that might be asked from the providers, the care team, the patient, and their family.
From the Nurse or Registered Dietician: The Primary Team Has Ordered Tube Feeds for a Patient Who Had a PEG Placed Today...How Soon Can We Start the Tube Feeds?
Traditionally, though the initiation of PEG tube feeding is delayed to 12–24 h after tube placement, a meta-analysis and multiple randomized controlled trials reported that patients started on earlier feedings (within 3 h of PEG placement) had no difference in complications, death within 72 h, or the amount of significant gastric residual volume after one day when compared with patients who were started on tube feeds the day after tube placement [2]. There is no standard of practice regarding the timing of feeding initiation. Since there is no current national consensus, each center or institution has their own practice guidelines. In order to prevent the tube from getting clogged, it should be flushed after each feed as well as before and after administrating any medications.
From the Patient’s Facility: How Tight Should the PEG Tube’s External Bolster Be Maintained?
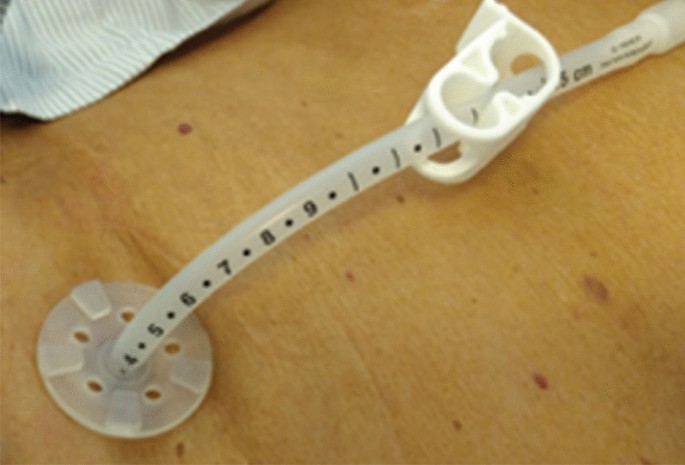
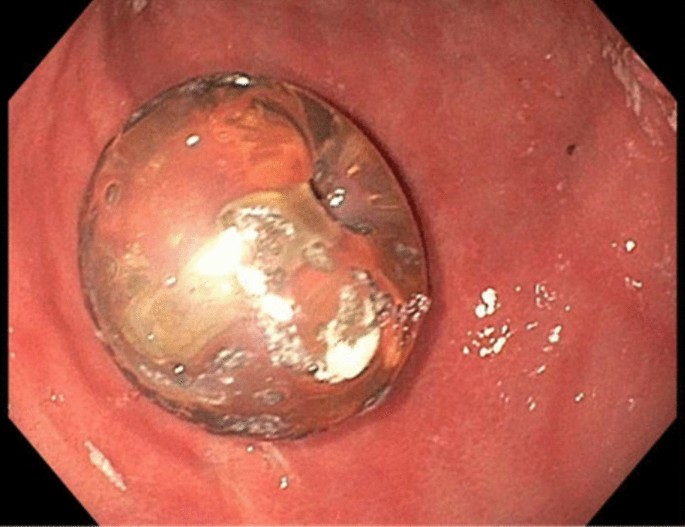
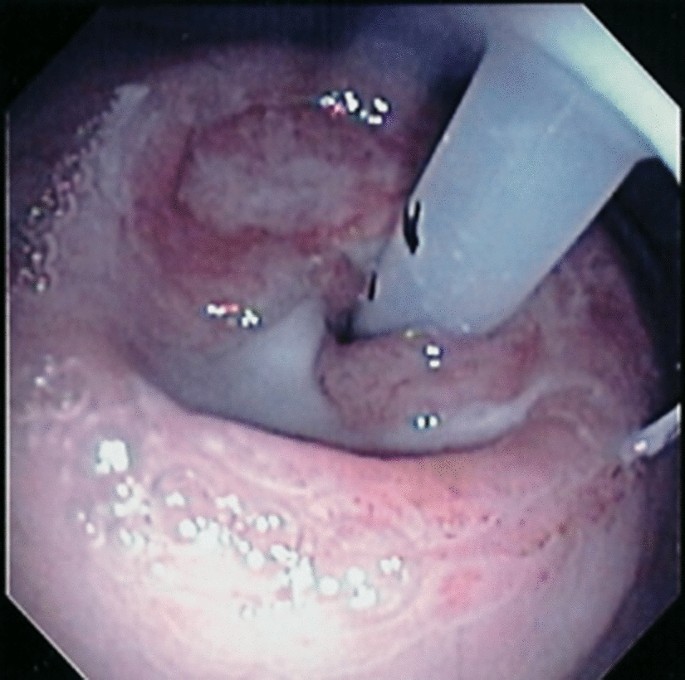
The external bolster of the PEG tube should be positioned loosely enough to allow for 1–2 cm of in-and-out movement of the tube (see Fig. 1 for appropriate tube positioning, Fig. 2 for PEG tube internal balloon-type bolster, and Fig. 3 for too-tight tube positioning leading to the buried bumper syndrome) [3]. Tissue compression between the internal and external bolsters can lead to pressure necrosis or breakdown of the gastrostomy tract. This loose positioning does not cause leakage around the tube, since a tract forms quickly due to tissue edema and inflammation.
Appropriate PEG tube positioning. Permission for image use obtained from the Journal of Digestive Endoscopy [15].
It is also important to document the initial location of the external bolster after placement in order to guide tube replacement when needed. Ideally, the initial location of the external bolster should be documented in the operative or procedure note on the date of placement and in all follow-up notes regarding the PEG tube. At our institution, we routinely place orders guiding tube care for the nursing staff after PEG placement. We round on all inpatients one day after PEG tube placement in order to ensure that the tube can freely rotate 360˚ and to tighten or loosen the tube if necessary. In the note, we document tube placement date, skin disc level, and the type of tube. We indicate whether or not it is safe to start tube feeds and document that the head of the bed should be elevated ≥ 30° during feedings and for 60 min thereafter. Moreover, we include the title of an institutional patient-focused handout that can be provided to patients upon discharge with further instructions for PEG tube care.
From the Inpatient Nurse: The Patient’s PEG Tube Is Clogged… How Do We Fix It?
Clogging is one of the most common complications of PEG tubes. If possible, all medications should be given in liquid form or dissolved in liquid in attempt to minimize clogging. Furthermore, bulking agents such as psyllium fiber should never be put through the tube. Water (15–30 cc) should be flushed through the tube before and after all medications and after all tube feeds.
If the tube becomes obstructed, it can be flushed with a higher volume syringe (for example, a 60 cc). It is best to use warm water for irrigation [4]. Coca Cola® has also been cited as a possible alternative to water for flushing since it may help prevent tube clogging and is of similar efficacy to water; nevertheless, evidence for Coca Cola® for resolution of existing clogs is limited and has not been reproducible [5]. If this does not work, pancreatic enzymes dissolved in bicarbonate can be left to dwell inside the tube [6]. As a last resort, the tube may be cleared with a brush.
From the Pharmacist: The Formulation of the Medication that Was Ordered Cannot Be Crushed or Administered Through the PEG… Does the Patient Really Need the Medication?
Oral medications need to be prepared properly for administration through the PEG tube. Tablets must be crushed and diluted, and capsules must be opened with the contents diluted. Many liquid forms of medications should also be further diluted prior to enteral administration through the PEG [7]. Many of the immediate-release tablets can be crushed and diluted before administration through the tube. Sublingual, enteric-coated, extended-release, or delayed-release medications should not be crushed since crushing these medications destroys the drug’s protective coating. Furthermore, crushed enteric-coated tablets may clump and clog PEG tubes [7]. Crushing these sublingual, extended-release, or delayed-release medications may lead to unpredictable blood levels and dangerous side effects. If it is unclear whether a medication is safe to be crushed and administered through a PEG tube, it should be discussed with a pharmacist prior to its use. Alternative non-enteric-coated or immediate-release options should be substituted when available.
From the Primary Team: The PEG Tube Looks Damaged and Is Leaking… How Do We Remove and Replace It?
Due to the corrosive actions of gastric acid and digestive enzymes, PEG tubes may deteriorate over time. Some signs of tube deterioration include tube discoloration, beading, and foul odor. Though these complications alone will not harm the patient, if the tube breaks and leaks, continuing tube feeds may be challenging or even impossible. In general, the lifespan of a PEG tube is about one year although PEG tubes may last much longer for many patients. One single center retrospective study found that PEG tube lifespan was 1 year for 95.1% of patients and five years for 68.5%. Younger age was associated with earlier PEG failure. [8]
PEG tubes may also develop peristomal leakage, which usually occurs in the first few days after tube placement but can also occur in patients with a mature gastrostomy tract. Loosening the external bolster may help, as well as improving malnutrition and hyperglycemia. Placing a larger PEG tube through the same tract will only distend the tract further and worsen leakage. In patients who already have a mature tract and develop peristomal leakage, the tube should be fully removed, allowing the tract to completely close, with placement of a new tube at another location.
Since the method of PEG tube removal depends on the type of tube present, it is essential to know which type of tube is in place before attempting to remove it. The term “PEG” should only be used to describe endoscopically placed tubes that initially have a soft internal bolster (bumper) that is located within the stomach and an external bolster, which is placed over the tube, external to the abdominal wall. The internal bolster can deform to enable the tube to be removed through the tract when firm and steady traction is applied, with most tubes designed to withstand 10–14 pounds of external pull force. Radiologically or surgically placed gastrostomy tubes and replacement tubes are removed endoscopically or percutaneously after balloon deflation. Tubes with an internal balloon can be identified by the presence of a printed balloon capacity, generally 5–10 cc, and tube diameter, usually 12–20 Fr., on or near the valve. The balloon is deflated by inserting a straight tip (not Luer Lock®) syringe into the valve and removing as much fluid as possible, after which the tube should slide out easily. If there is any question regarding the type of tube, the patient’s medical record should be searched for operative or procedural notes detailing when the tube was placed and by whom. If the type of tube is incorrectly documented as a PEG tube, confusion and misguided attempts at removal may occur. If the type of tube cannot be determined based on exam and the patient’s medical record, an endoscopy should be performed to determine which type of internal bolster is present. After the tube is removed, the site should be covered with a clean dressing until the tract closes, which typically takes 24–72 h after removal.
Though replacement tubes have a balloon at the distal tip, they should only be placed once the tract has matured, which may take up to 4 weeks after placement. The balloon is inflated after placement with water or saline using a straight tip (not Luer Lock®), with an external bolster placed to secure the tube. If the patient had an internal bolster balloon, and it was deflated early leading to dislodgement of the tube, a replacement tube with a soft bumper rather than an internal balloon should be used.
From the Emergency Department: This Patient’s PEG Tube Was Accidentally Removed… What Do We Do?
PEG tubes may be accidentally removed due to excess traction, especially by patients who are agitated or confused. If this occurs when the tract is mature (at least 4 weeks old), a replacement tube can be placed through the tract. If the appropriate tube is not available, a Foley catheter may be temporarily used. The catheter is placed through the gastrostomy tract after which the balloon at the distal tip is inflated. To create an external bolster, a 2–3-cm piece of tubing can be cut from a second Foley catheter. A hole can be cut into the middle of this piece of tubing, and the tubing of the replacement tube passed through the hole.
Since the gastrostomy tract starts to close within hours, replacement of the tube should occur as soon as possible. If the tube is accidentally removed within the first 4 weeks after placement, it should not be replaced blindly, since the gastric and abdominal walls may have separated in an immature tract, with the possibility of intraperitoneal insertion. If there is concern this may have occurred, a water-soluble contrast dye study through the tube should be obtained emergently to confirm correct positioning before using the tube for feeding to prevent potentially serious complications.
From the Patient’s Caregiver: Buried Bumper Syndrome Sounds Frightening… How Do We Prevent It?
Buried bumper syndrome is a late complication due to the external bolster of the PEG tube being too-tight against the abdominal wall [9]. Over time, the internal bolster erodes into the gastric wall due to the tension on the tract with consequent pain and the inability to give feeds through the tube. Endoscopy will show that the internal bolster is buried within the gastric wall.
Prevention requires good PEG site care and patient education. It is important to leave enough space between the external bolster and abdominal wall. Gauze pads should only be placed over the external bolster since placing them underneath the bolster can create excess pressure on the gastrostomy tract. The tube itself should be pushed into the wound slightly and rotated during daily tube care, ensuring that the internal bumper does not become buried. It should then be placed back into the initial position.
From the Patient: Can I Go Swimming with a PEG Tube?
Patients may shower with their PEG tube in place as long as they pat the surrounding skin dry afterwards. They should wait for 4 weeks before submerging their PEG tube underwater in a bathtub. Though there is no evidence-based recommendation regarding swimming with a PEG tube, there are, however, multiple patient resource and support group websites discussing this topic. According to the Feeding Tube Awareness Foundation, for example, it is safe to go swimming with a PEG tube as long as the stoma has matured [10]. Swimming in well-maintained chlorinated or saltwater pools and oceans is preferred over lakes and rivers due to the possibility of unsafe water quality. Hot tubs are also ill-advised, since they often harbor bacteria. If the tube site is exposed to sand or other suspended debris, covering the tube it in a clear, protective dressing or plastic wrap with waterproof tape is recommended.
Infections are one of the more common PEG tube complications. Though most are minor, severe infections such as peritonitis or necrotizing fasciitis may occur [11]. Signs of possible wound infection include erythema around the tube site, tenderness, and/or purulence. Most of these infections will respond to antibiotics (either a first-generation cephalosporin or fluoroquinolone). If there are signs of a more severe infection, the tube should be removed after which additional antibiotics are started. Necrotizing fasciitis is a rare complication of PEG tube placement, for which patients with diabetes, wound infections, malnutrition, and immunocompromise are at increased risk. Patients should use increased caution with swimming and exposure of their PEG site to water. Maintaining sufficient space between the external bolster and abdominal wall may help to prevent this as well. [12]
From the Home Health Nurse: The Patient Has a PEG Tube for Venting... How Does This Work?
PEG tubes may be used for venting rather than feeding in patients with chronic nausea, vomiting, and abdominal pain related to gastrointestinal obstruction. Gastric decompression through a venting PEG tube can palliate symptoms [13]. Venting a PEG tube removes air and drains gastric juice in order to improve the above symptoms. When symptoms are under control, the PEG tube can be kept clamped or closed. When the patient becomes nauseated, the tube can be unclamped and allowed to drain until the symptoms improve. After the symptoms have gone away, the tube can again be clamped and eventually removed.
From the Primary Team: The Patient Has a PEG Tube... Can It Be Converted to a PEG-J?
Yes – a PEG tube may be converted endoscopically to a jejunal extension tube (PEG-J). Placement of a PEG-J placement, typically a two-step procedure, is used in patients who cannot tolerate gastric feeding. The first step is placement of the PEG tube, and the second step is insertion of a J extension tube through the PEG tube. Once this is inserted, the J extension tube is grasped with tools placed into the endoscope. The J extension tube is then guided through the stomach, pylorus, and small bowel until it is in position in the jejunum, distal to the ligament of Treitz. The jejunal extension tube may then be clipped to the mucosa [14].
Conclusions
Although GI fellows may know how to place PEG tubes, they may lack knowledge regarding the nuances of PEG tube management. It is important to know the type of PEG tube and internal bolster present before attempting to remove it. If a PEG tube falls out and needs replacement, it should be done as quickly as possible, given the tract can start to close within hours. Additionally, tube positioning is extremely important; the external bolster should be positioned loosely enough to allow for 1–2 cm of in-and-out movement in order to prevent complications such as buried bumper syndrome.
The common questions included in this article regarding the proper management of PEG tubes come from patients, their caregivers, and their healthcare teams. We hope this guide will help answer some of these frequently asked questions. Notably, improved documentation in patients’ medical records, communication with, and educational resources for patients, families, and members of the healthcare team can help to answer some of these questions up front.
References
Abdelfattah T, Kaspar M. Gastroenterologist’s guide to gastrostomies. Dig Dis Sci. 2022;67:3488–3496.
Szary NM, Arif M, Matteson ML et al. Enteral feeding within three hours after percutaneous endoscopic gastrostomy placement: a meta-analysis. J Clin Gastroenterol. 2011;45:e34–e38.
Gupta A, Singh AK, Goel D et al. Mittal S Percutaneous endoscopic gastrostomy tube placement: a single center experience. Journal of Digestive Endoscopy. 2019. https://doi.org/10.1055/s-0039-3401391.
Metheny N, Eisenberg P, McSweeney M. Effect of feeding tube properties and three irrigants on clogging rates. Nurs Res. 1988;37:165.
Dandeles LM, Lodolce AE. Efficacy of agents to prevent and treat enteral feeding tube clogs. Ann Pharmacother. 2011;45:676–680.
Sriram K, Jayanthi V, Lakshmi RG et al. Prophylactic locking of enteral feeding tubes with pancreatic enzymes. JPEN J Parenter Enteral Nutr. 1997;21:353.
Grissinger M. Preventing errors when drugs are given via enteral feeding tubes. P T. 2013;38:575–576.
Siau K, Troth T, Gibson E et al. Fisher NC How long do percutaneous endoscopic gastrostomy feeding tubes last? A retrospective analysis. Postgrad Med J. 2018;94:469–474.
Klein S, Heare BR, Soloway RD. The “buried bumper syndrome”: a complication of percutaneous endoscopic gastrostomy. Am J Gastroenterol 1990;85:448.
Swimming, traveling, and camping. Feeding Tube Awareness Foundation; [Accessed 2022 Dec 28]. http://www.feedingtubeawareness.org/swimming/
Sharma VK, Howden CW. Meta-analysis of randomized, controlled trials of antibiotic prophylaxis before percutaneous endoscopic gastrostomy. Am J Gastroenterol 2000;95:3133.
Hucl T, Spicak J. Complications of percutaneous endoscopic gastrostomy. Best Pract Res Clin Gastroenterol 2016;30:769.
Teriaky A, Gregor J, Chande N. Percutaneous endoscopic gastrostomy tube placement for end-stage palliation of malignant gastrointestinal obstructions. Saudi J Gastroenterol 2012;18:95–98.
Simons-Linares CR, Milano R, Bartel MJ. PEG-J tube placement with optimization of J tube insertion. VideoGIE. 2021;6:112–113.
Gupta A, Singh AK, Goel D et al. Percutaneous endoscopic gastrostomy tube placement: a single center experience. J Digest Endosc 2019;10:150–154.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ley, D., Saha, S. Everything that You Always Wanted to Know About the Management of Percutaneous Endoscopic Gastrostomy (PEG) Tubes (but Were Afraid to Ask). Dig Dis Sci 68, 2221–2225 (2023). https://doi.org/10.1007/s10620-023-07944-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-023-07944-y