Abstract
Background and Aim
Roux-En-Y gastric bypass (RYGB) is associated with risk of alcohol use disorder. The impact of RYGB among patients with alcohol-associated liver disease (ALD) remains unknown.
Methods
A retrospective cohort from National Inpatient Sample (01/2006–09/2015) database on 421,156 admissions with alcohol-associated cirrhosis (AC) was stratified for non-primary discharge diagnosis of previous RYGB. Admissions with RYGB (cases) were matched 1:3 to without RYGB (controls) based on propensity score on demographics, calendar year, socioeconomic status (insurance and zip code income quartile), obesity, diabetes, anxiety, and alcohol use disorder. Primary outcome was concomitant discharge diagnosis of alcoholic hepatitis (AH) or development of acute on chronic liver failure (ACLF).
Results
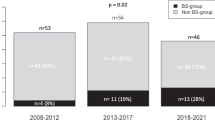
Of 10,168 admissions (mean age 49 yrs., 75% females, 79% whites), cases (N = 2542) vs. controls had higher prevalence of concomitant AH (18.8 vs. 17%, P = 0.032), hepatic encephalopathy (31 vs. 25%), infection (28 vs. 24%), and grade 3 ACLF (13 vs. 5%), P < 0.001. Conditional logistic regression models showed higher odds for AH, hepatic encephalopathy, and infection among cases. In-hospital mortality of 6.3% (43% in ACLF) was lower in cases, but similar in the sub-cohorts of AH (N = 1768) or ACLF (N = 768). Results were similar in a sensitivity analysis of matched cohort of 2016 hospitalizations (504 cases) with primary discharge diagnosis of AC.
Conclusion
Among patients with AC, previous RYGB is associated with increased likelihood of concomitant AH, hepatic encephalopathy, and infection, but similar in-hospital mortality. Prospective studies are needed to validate, determine causality, and understand mechanisms of these findings among patients with alcohol-associated cirrhosis.



Similar content being viewed by others
References
Singal AK, Mathurin P. diagnosis and management of alcohol-associated liver disease: a review. JAMA 2021;326:165–176.
Collaborators GBDC. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:245–266.
Global status report on alcohol and health. Geneva: World Health Organization, 2018.
Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999–2016: observational study. BMJ 2018;362:k2817.
Singal AK, Arsalan A, Dunn W et al. Alcohol-associated liver disease in the US is associated with severe forms of disease among young, females and Hispanics. Aliment Pharmacol Ther. 2021. https://doi.org/10.1111/apt.16461.
Singal AK, Arora S, Wong RJ et al. Increasing burden of acute-on-chronic liver failure among alcohol-associated liver disease in the young population in the United States. Am J Gastroenterol. 2020;115:88–95.
Salameh H, Raff E, Erwin A et al. PNPLA3 gene polymorphism is associated with predisposition to and severity of alcoholic liver disease. Am J Gastroenterol. 2015;110:846–856.
Singal AK, Kuo YF, Anand BS. Hepatitis C virus infection in alcoholic hepatitis: prevalence patterns and impact on in-hospital mortality. Eur J Gastroenterol Hepatol. 2012;24:1178–1184.
Singal AK, Kodali S, Vucovich LA, Darley-Usmar V, Schiano TD. Diagnosis and treatment of alcoholic hepatitis: a systematic review. Alcohol Clin Exp Res. 2016;40:1390–1402.
Axley PD, Richardson CT, Singal AK. Epidemiology of alcohol consumption and societal burden of alcoholism and alcoholic liver disease. Clin Liver Dis. 2019;23:39–50.
Kwo PY, Cohen SM, Lim JK. ACG Clinical Guideline: evaluation of abnormal liver chemistries. Am J Gastroenterol. 2017;112:18–35.
Heymsfield SB, Wadden TA. Mechanisms, pathophysiology, and management of obesity. N Engl J Med. 2017;376:254–266.
Arterburn DE, Telem DA, Kushner RF, Courcoulas AP. Benefits and risks of bariatric surgery in adults: a review. JAMA 2020;324:879–887.
Mechanick JI, Youdim A, Jones DB et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient–2013 update: cosponsored by American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric. Surgery. Obesity (Silver Spring) 2013;21:S1-27.
English WJ, DeMaria EJ, Hutter MM et al. American Society for Metabolic and Bariatric Surgery 2018 estimate of metabolic and bariatric procedures performed in the United States. Surg Obes Relat Dis 2020;16:457–463.
King WC, Chen JY, Mitchell JE et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA 2012;307:2516–2525.
Svensson PA, Anveden A, Romeo S et al. Alcohol consumption and alcohol problems after bariatric surgery in the Swedish obese subjects study. Obesity (Silver Spring) 2013;21:2444–2451.
Conason A, Teixeira J, Hsu CH, Puma L, Knafo D, Geliebter A. Substance use following bariatric weight loss surgery. JAMA Surg. 2013;148:145–150.
Ostlund MP, Backman O, Marsk R et al. Increased admission for alcohol dependence after gastric bypass surgery compared with restrictive bariatric surgery. JAMA Surg. 2013;148:374–377.
Spadola CE, Wagner EF, Dillon FR, Trepka MJ, De La Cruz-Munoz N, Messiah SE. Alcohol and drug use among postoperative bariatric patients: a systematic review of the emerging research and its implications. Alcohol Clin Exp Res 2015;39:1582–1601.
Kim HP, Jiang Y, Farrell TM, Peat CM, Hayashi PH, Barritt ASt. Roux-en-Y gastric bypass is associated with increased hazard for de novo alcohol-related complications and liver disease. J Clin Gastroenterol. 2021. https://doi.org/10.1097/MCG.0000000000001506.
Serrano OK, Peterson KJ, Vock DM et al. Clinical impact of antecedent bariatric surgery on liver transplant outcomes: a retrospective matched case-control study. Transplantation 2021;105:1280–1284.
Singal AK, Ahmed Z, Axley P et al. Hospitalizations for acute on chronic liver failure at academic compared to non-academic centers have higher mortality. Dig Dis Sci. 2020;66:1306.
Bajaj JS. Defining acute-on-chronic liver failure: will East and West ever meet? Gastroenterology. 2013;144:1337–1339.
Waleed M, Abdallah MA, Kuo YF, Arab JP, Wong R, Singal AK. Higher frequency of hospital-acquired infections but similar in-hospital mortality among admissions with alcoholic hepatitis at academic vs. non-academic centers. Front Physiol. 2020;11:594138.
Davis JF, Tracy AL, Schurdak JD et al. Roux en Y gastric bypass increases ethanol intake in the rat. Obes Surg. 2013;23:920–930.
King WC, Chen JY, Courcoulas AP et al. Alcohol and other substance use after bariatric surgery: prospective evidence from a U.S. multicenter cohort study. Surg Obes Relat Dis. 2017;13:1392–1402.
Steffen KJ, Engel SG, Pollert GA, Li C, Mitchell JE. Blood alcohol concentrations rise rapidly and dramatically after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2013;9:470–473.
Ivezaj V, Benoit SC, Davis J et al. Changes in alcohol use after metabolic and bariatric surgery: predictors and mechanisms. Curr Psychiatry Rep. 2019;21:85.
Chalasani N, Younossi Z, Lavine JE et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67:328–357.
Pose E, Trebicka J, Mookerjee RP et al. Statins: old drugs as new therapy for liver diseases? J Hepatol. 2019;70:194–202.
Jinjuvadia R, Liangpunsakul S, Translational R. Evolving alcoholic hepatitis treatment C. trends in alcoholic hepatitis-related hospitalizations, financial burden, and mortality in the United States. J Clin Gastroenterol. 2015;49:506–511.
Funding
The study did not receive any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yarra, P., Dunn, W., Younossi, Z. et al. Association of Previous Gastric Bypass Surgery and Patient Outcomes in Alcohol-Associated Cirrhosis Hospitalizations. Dig Dis Sci 68, 1026–1034 (2023). https://doi.org/10.1007/s10620-022-07591-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-022-07591-9