Abstract
Background and Aims
Crohn’s disease (CD) can lead to work disability with social and economic impacts worldwide. In Brazil, where its prevalence is increasing, we assessed the indirect costs, prevalence, and risk factors for work disability in the state of Rio de Janeiro and in a tertiary care referral center of the state.
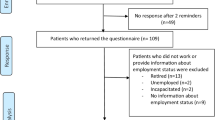
Methods
Data were retrieved from the database of the Single System of Social Security Benefits Information, with a cross-check for aid pension and disability retirement. A subanalysis was performed with CD patients followed up at the tertiary care referral center using a prospective CD database, including clinical variables assessed as possible risk factors for work disability.
Results
From 2010 to 2018, the estimated prevalence of CD was 26.05 per 100,000 inhabitants, while the associated work disability was 16.6%, with indirect costs of US$ 8,562,195.86. Permanent disability occurred more frequently in those aged 40 to 49 years. In the referral center, the prevalence of work disability was 16.7%, with a mean interval of 3 years between diagnosis and the first benefit. Risk factors for absence from work were predominantly abdominal surgery, anovaginal fistulas, disease duration, and the A2 profile of the Montreal classification.
Conclusions
In Rio de Janeiro, work disability affects one-sixth of CD patients, and risk factors are associated with disease duration and complications. In the context of increasing prevalence, as this disability compromises young patients after a relatively short period of disease, the socioeconomic burden of CD is expected to increase in the future.


Similar content being viewed by others
Abbreviations
- IBD:
-
Inflammatory bowel disease
- CD:
-
Crohn’s disease
- INSS:
-
National Institute of Social Security
- SUIBE:
-
Unified Benefits Information System
References
de Souza HS, Fiocchi C. Immunopathogenesis of IBD: current state of the art. Nat Rev Gastroenterol Hepatol. 2016;13:13–27.
Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015;12:205–217.
Spekhorst LM, Oldenburg B, van Bodegraven AA, et al. Prevalence of- and risk factors for work disability in Dutch patients with inflammatory bowel disease. World J Gastroenterol. 2017;23:8182–8192.
Burisch J, Jess T, Martinato M, Lakatos PL, EpiCom E. The burden of inflammatory bowel disease in Europe. J Crohn’s Colitis.. 2013;7:322–337.
Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2018;390:2769–2778.
Collaborators GBDIBD. The global, regional, and national burden of inflammatory bowel disease in 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet Gastroenterol Hepatol. 2020;2020(5):17–30.
Molodecky NA, Soon IS, Rabi DM, et al. Increasing incidence and prevalence of the inflammatory bowel diseases with time, based on systematic review. Gastroenterology. 2012;142:46–54 e42; quiz e30.
Parente JM, Coy CS, Campelo V, et al. Inflammatory bowel disease in an underdeveloped region of Northeastern Brazil. World J Gastroenterol. 2015;21:1197–1206.
Gasparini RG, Sassaki LY, Saad-Hossne R. Inflammatory bowel disease epidemiology in Sao Paulo State. Braz Clin Exp Gastroenterol. 2018;11:423–429.
Quaresma AB, Kaplan GG, Kotze PG. The globalization of inflammatory bowel disease: the incidence and prevalence of inflammatory bowel disease in Brazil. Curr Opin Gastroenterol. 2019;35:259–264.
Kotze PG, Underwood FE, Damiao A, et al. Progression of inflammatory bowel diseases throughout Latin America and the Caribbean: a systematic review. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2020;18:304–312.
Lima Martins A, Volpato RA, Zago-Gomes MDP. The prevalence and phenotype in Brazilian patients with inflammatory bowel disease. BMC Gastroenterol. 2018;18:87.
Victoria CR, Sassak LY, Nunes HR. Incidence and prevalence rates of inflammatory bowel diseases, in midwestern of Sao Paulo State, Brazil. Arquiv Gastroenterol. 2009;46:20–25.
da Luz Moreira A, de Campos Lobato LF, de Souza HS. IBD Epidemiology: What is going on in the developing world? Results from 163,000 patients. Gastroenterology. 2019;156:S-73.
Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory. Bowel Dis Gastroenterol. 2017;152(313–321):e312.
Bassi A, Dodd S, Williamson P, Bodger K. Cost of illness of inflammatory bowel disease in the UK: a single centre retrospective study. Gut. 2004;53:1471–1478.
Abraham BP, Sellin JH. Disability in inflammatory bowel disease. Gastroenterol Clini North Am. 2012;41:429–441.
Binder V, Hendriksen C, Kreiner S. Prognosis in Crohn’s disease–based on results from a regional patient group from the county of Copenhagen. Gut. 1985;26:146–150.
Kvien TK. Epidemiology and burden of illness of rheumatoid arthritis. PharmacoEconomics. 2004;22:1–12.
Lidgren M, Wilking N, Jonsson B. Cost of breast cancer in Sweden in 2002. Eur J Health Econ HEPAC Health Econ Prev Care.. 2007;8:5–15.
Schmid A, Pugin J, Chevrolet JC, et al. Burden of illness imposed by severe sepsis in Switzerland. Swiss Med Wkly.. 2004;134:97–102.
Pillai N, Dusheiko M, Maillard MH, et al. The evolution of health care utilisation and costs for inflammatory bowel disease over ten years. J Crohn’s Colitis. 2019;13:744–754.
Kaplan GG. The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol. 2015;12:720–727.
de SBFR, Carvalho ATP, de VCAJ, et al. The socio-economic impact of work disability due to inflammatory bowel disease in Brazil. Eur J Health Econ HEPAC Health Econ Prev Care. 2018;19:463–470.
(IBGE) BNIoGaS. IBGE releases estimates of municipal population for 2019. https://agenciadenoticias.ibge.gov.br/agencia-sala-de-imprensa/2013-agencia-de-noticias/releases/25278-ibge-divulga-as-estimativas-da-populacaodosmunicipios-para-2019. Section: Social Statistics. Accessed 29 Aug 2019.
Hoivik ML, Moum B, Solberg IC, et al. Work disability in inflammatory bowel disease patients 10 years after disease onset: results from the IBSEN Study. Gut. 2013;62:368–375.
Stjernman H, Tysk C, Almer S, Strom M, Hjortswang H. Unfavourable outcome for women in a study of health-related quality of life, social factors and work disability in Crohn’s disease. Europ J Gastroenterol Hepatol. 2011;23:671–679.
Parra RS, Chebli JMF, Amarante H, et al. Quality of life, work productivity impairment and healthcare resources in inflammatory bowel diseases in Brazil. World J Gastroenterol. 2019;25:5862–5882.
De Boer AG, Bennebroek Evertsz F, Stokkers PC, et al. Employment status, difficulties at work and quality of life in inflammatory bowel disease patients. Eur J Gastroenterol Hepatol.. 2016;28:1130–1136.
Sonnenberg A. Disability and need for rehabilitation among patients with inflammatory bowel disease. Digestion.. 1992;51:168–178.
Kawalec P, Malinowski KP. Indirect health costs in ulcerative colitis and Crohn’s disease: a systematic review and meta-analysis. Expert Rev Pharmacoecon Outcomes Res. 2015;15:253–266.
Pillai N, Lupatsch JE, Dusheiko M, et al. Evaluating the cost-effectiveness of early compared with late or no biologic treatment to manage Crohn’s disease using real-world data. J Crohn’s Colitis. 2020;14:490–500.
Kuenzig ME, Lee L, El-Matary W, et al. The impact of inflammatory bowel disease in Canada 2018: indirect costs of IBD care. J Can Assoc Gastroenterol. 2019;2:S34–S41.
Mandel MD, Balint A, Lovasz BD, et al. Work disability and productivity loss in patients with inflammatory bowel diseases in Hungary in the era of biologics. Eur J Health Econ HEPAC Health Econ Prev Care. 2014;15(Suppl 1):S121–128.
Schoepfer A, Santos J, Fournier N, et al. Systematic analysis of the impact of diagnostic delay on bowel damage in paediatric versus adult onset Crohn’s disease. J Crohn’s Colitis. 2019;13:1334–1342.
Ramos A, Calvet X, Sicilia B, et al. IBD-related work disability in the community: prevalence, severity and predictive factors. A Cross-Sect Study United Eur Gastroenterol J.. 2015;3:335–342.
Rutgeerts P, Van Assche G, Sandborn WJ, et al. Adalimumab induces and maintains mucosal healing in patients with Crohn’s disease: data from the EXTEND trial. Gastroenterology.. 2012;142(1102–1111):e1102.
Colombel JF, Rutgeerts PJ, Sandborn WJ, et al. Adalimumab induces deep remission in patients with Crohn’s disease. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc. 2014;12(414–422):e415.
Feagan BG, Vreeland MG, Larson LR, Bala MV. Annual cost of care for Crohn’s disease: a payor perspective. Am J Gastroenterol. 2000;95:1955–1960.
Neuendorf R, Harding A, Stello N, Hanes D, Wahbeh H. Depression and anxiety in patients with inflammatory bowel disease: a systematic review. J Psychosom Res. 2016;87:70–80.
Acknowledgments
This work was supported by grants from the Brazilian Research Council (CNPq) (302401/2016-4) and the FAPERJ (Fundação Carlos Chagas Filho de Amparo a Pesquisa do Estado do Rio de Janeiro) (E26/202.781/2017).
Funding
This research was supported by grants from Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro-FAPERJ and Conselho Nacional de Desenvolvimento Científico e Tecnológico–CNPq.
Author information
Authors and Affiliations
Contributions
RSBF and ADLM participated in the conception and design of the study; the acquisition, analysis and interpretation of the data; and the drafting the manuscript. AJC, RRL, JPLM, AMHBM, and CCM participated in the acquisition, analysis, and interpretation of the data and in drafting parts of the manuscript. ATC and HSPdS participated in the conception and design of the study, obtained funding, analyzed and interpreted the data, and critically revised the manuscript for important intellectual content. All authors gave final approval of the submitted version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests related to this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
de Sá Brito Fróes, R., da Luz Moreira, A., Carneiro, A.J.d. et al. Prevalence, Indirect Costs, and Risk Factors for Work Disability in Patients with Crohn’s Disease at a Tertiary Care Center in Rio de Janeiro. Dig Dis Sci 66, 2925–2934 (2021). https://doi.org/10.1007/s10620-020-06646-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06646-z