Abstract
Background and Aims
Socioeconomic status, race, and insurance can impact healthcare delivery and utilization in several chronic disease states. The primary aim of our study was to determine whether race and insurance status are predictors of having an appropriate workup for celiac disease and inflammatory bowel disease (IBD) when presenting with iron deficiency anemia (IDA) and chronic diarrhea.
Methods
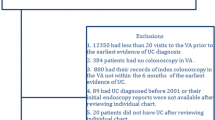
Medical records of patients seen at the University of Chicago Medical Center between January 1, 2006, and September 20, 2017, were reviewed. Patients with two separate encounters within 6 months associated with the diagnosis codes for both IDA and chronic diarrhea were identified. Patients without a diagnosis code for IBD and celiac disease were further grouped as those that had an “appropriate” workup and those that did not. Factors associated with the appropriate evaluation were analyzed by univariate and multivariate logistic regression.
Results
In total, 899,701 records were searched. A total of 83 patients fit inclusion into the study (8 IBD, 3 CD, 72 neither IBD or CD). Black race was associated with a 91% decreased odds of having the appropriate workup on univariate (OR 0.090, 95%CI 0.017–0.475, p = 0.005) and age-adjusted multivariate analysis (OR 0.095, 95% CI 0.017–0.527, p = 0.007). Public insurance status was significantly associated with a 90% decreased odds of appropriate workup on univariate (OR 0.102, 95% CI 0.024–0.438, p = 0.002) and age-adjusted multivariate analysis (OR 0.104, 95% CI 0.021–0.513, p = 0.005).
Conclusions
Black race and public insurance were significantly associated with not having an appropriate workup for IBD and celiac disease when presenting with iron deficiency and chronic diarrhea.


Similar content being viewed by others
References
Gasche C, Lomer MC, Cavill I, Weiss G. Iron, anaemia, and inflammatory bowel diseases. Gut. 2004;53:1190–1197.
Rubio-Tapia A, Hill ID, Kelly CP, Calderwood AH, Murray JA, Gastroenterology ACo. ACG clinical guidelines: diagnosis and management of celiac disease. Am J Gastroenterol. 2013;108:656–676.
Schiller LR, Pardi DS, Sellin JH. Chronic diarrhea: diagnosis and management. Clin Gastroenterol Hepatol.. 2017;15:182–193.e183.
World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. 2011.
Mahadev S, Laszkowska M, Sundström J, et al. Prevalence of celiac disease in patients with iron deficiency anemia-a systematic review with meta-analysis. Gastroenterology. 2018;155:374–382.e371.
Eriksson C, Henriksson I, Brus O, et al. Incidence, prevalence and clinical outcome of anaemia in inflammatory bowel disease: a population-based cohort study. Aliment Pharmacol Ther. 2018.
Goddard AF, James MW, McIntyre AS, Scott BB, Gastroenterology BSo. Guidelines for the management of iron deficiency anaemia. Gut. 2011;60:1309–1316.
Smalley W, Falck-Ytter C, Carrasco-Labra A, Wani S, Lytvyn L, Falck-Ytter Y. AGA clinical practice guidelines on the laboratory evaluation of functional diarrhea and diarrhea-predominant irritable bowel syndrome in adults (IBS-D). Gastroenterology. 2019;157:851–854.
Baumgart DC, Sandborn WJ. Crohn’s disease. Lancet. 2012;380:1590–1605.
Sewell JL, Velayos FS. Systematic review: The role of race and socioeconomic factors on IBD healthcare delivery and effectiveness. Inflamm Bowel Dis. 2013;19:627–643.
Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283:2579–2584.
Institute of Medicine (U.S.). Committee on the Consequences of Uninsurance. Care without coverage: too little, too late. Washington, D.C.: National Academy Press; 2002.
Mardini HE, Westgate P, Grigorian AY. Racial differences in the prevalence of celiac disease in the US population: National Health and Nutrition Examination Survey (NHANES) 2009–2012. Dig Dis Sci. 2015;60:1738–1742.
Thia KT, Sandborn WJ, Harmsen WS, Zinsmeister AR, Loftus EV. Risk factors associated with progression to intestinal complications of Crohn’s disease in a population-based cohort. Gastroenterology. 2010;139:1147–1155.
Freeman HJ. Adult celiac disease and its malignant complications. Gut Liver. 2009;3:237–246.
Bottaro G, Cataldo F, Rotolo N, Spina M, Corazza GR. The clinical pattern of subclinical/silent celiac disease: an analysis on 1026 consecutive cases. Am J Gastroenterol. 1999;94:691–696.
Lo W, Sano K, Lebwohl B, Diamond B, Green PH. Changing presentation of adult celiac disease. Dig Dis Sci. 2003;48:395–398.
Harper JW, Holleran SF, Ramakrishnan R, Bhagat G, Green PH. Anemia in celiac disease is multifactorial in etiology. Am J Hematol. 2007;82:996–1000.
Gisbert JP, Gomollón F. Common misconceptions in the diagnosis and management of anemia in inflammatory bowel disease. Am J Gastroenterol. 2008;103:1299–1307.
Abu Daya H, Lebwohl B, Lewis SK, Green PH. Celiac disease patients presenting with anemia have more severe disease than those presenting with diarrhea. Clin Gastroenterol Hepatol. 2013;11:1472–1477.
Koutroubakis IE, Ramos-Rivers C, Regueiro M, et al. Persistent or recurrent anemia is associated with severe and disabling inflammatory bowel disease. Clin Gastroenterol Hepatol. 2015;13:1760–1766.
Sofia MA, Rubin DT, Hou N, Pekow J. Clinical presentation and disease course of inflammatory bowel disease differs by race in a large tertiary care hospital. Dig Dis Sci. 2014;59:2228–2235.
Anyane-Yeboa A, Yamada A, Haider H, et al. A comparison of the risk of postoperative recurrence between African–American and Caucasian patients with Crohn’s disease. Aliment Pharmacol Ther. 2018.
Dotson JL, Kappelman MD, Chisolm DJ, Crandall WV. Racial disparities in readmission, complications, and procedures in children with Crohn’s disease. Inflamm Bowel Dis. 2015;21:801–808.
Dotson JL, Cho M, Bricker J, et al. Race differences in initial presentation, early treatment, and 1-year outcomes of pediatric Crohn’s disease: results from the improvecarenow network. Inflamm Bowel Dis.. 2017;23:767–774.
Fiscella K, Sanders MR. Racial and ethnic disparities in the quality of health care. Annu Rev Public Health. 2016;37:375–394.
Marrast LM, Zallman L, Woolhandler S, Bor DH, McCormick D. Minority physicians’ role in the care of underserved patients: diversifying the physician workforce may be key in addressing health disparities. JAMA Intern Med. 2014;174:289–291.
Author information
Authors and Affiliations
Contributions
AAY was involved in drafting of manuscript, data acquisition, analysis and interpretation, revision of manuscript, and drafting of tables and figures; BL was involved in data acquisition, drafting of manuscript, and tables and figures; CT was involved in data analysis and interpretation, and critical revision of manuscript; AIE was involved in data analysis and interpretation, and critical revision of manuscript; PS was involved in data analysis and interpretation, drafting of tables and figures, and critical revision of manuscript; VR was involved in data analysis and interpretation, drafting of tables and figures, and critical revision of manuscript; DTR was involved in study concept and design, drafting of manuscript, critical revision of manuscript, and final approval of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anyane-Yeboa, A., Li, B., Traboulsi, C. et al. Black Race and Public Insurance Are Predictive of Inappropriate Evaluation of Iron Deficiency Anemia and Diarrhea. Dig Dis Sci 66, 2200–2206 (2021). https://doi.org/10.1007/s10620-020-06434-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06434-9