Abstract
Background
Gastric food residue frequently is observed on endoscopy despite fasting.
Aims
To delineate factors promoting endoscopic food retention in the stomach.
Methods
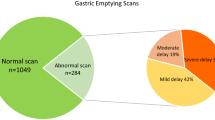
Two series of analyses were performed. Magnitudes of retained food in 834 patients from an endoscopy database were related to obstructive versus non-obstructive etiologies and gastric emptying findings. Emptying delays in 619 patients from a scintigraphy database were associated with endoscopic food retention, gastroparesis etiologies, and medications that modify gastric transit.
Results
On endoscopy, 310 (37 %) had large, 338 (41 %) showed medium, and 103 (12 %) exhibited small amounts of retained food in the stomach. Of 433 patients with definable etiologies of food retention, 106 (24 %) had obstructive causes. One hundred three of 327 (31 %) with non-obstructive conditions underwent scintigraphy showing mean 52 ± 29 % 4-h retention. From the scintigraphy database, 164/619 patients (26 %) with delayed emptying exhibited food retention on endoscopy. Four-hour scintigraphic retention was greater with versus without retained food (41 ± 25 vs. 32 ± 22 %, P < 0.001). Retained food occurred more frequently with postsurgical (28/69, 41 %) versus diabetic (33/139, 24 %) and idiopathic (65/294, 22 %) gastroparesis (P = 0.006). Opiate use was more prevalent with increasing food retention (P = 0.02), while other medications that delay or accelerate emptying did not relate to retained food.
Conclusions
Gastric food retention has obstructive and non-obstructive causes, and is found in one-quarter of gastroparesis, especially postsurgical cases. Gastric emptying delays correlate with amounts of retained food on endoscopy. Retention is influenced by opiates, but not other medications. These analyses delineate pathogenic factors promoting gastric food retention.



Similar content being viewed by others
References
Sander R, Frankenberger U. The use of endoscopy in patients with gastrointestinal motility problems. J Clin Gastroenterol. 2001;33:185–190.
ASGE Standards of Practice Committee, Fukami N, Anderson MA, et al. The role of endoscopy in gastroduodenal obstruction and gastroparesis. Gastrointest Endosc. 2011;74:13–21.
Parkman HP, Schwartz SS. Esophagitis and gastroduodenal disorders associated with diabetic gastroparesis. Arch Intern Med. 1987;147:1477–1480.
Maddern GJ, Chatterton BE, Collins PJ, Horowitz M, Shearman DJ, Jamieson GG. Solid and liquid gastric emptying in patients with gastro-oesophageal reflux. Br J Surg. 1985;72:344–347.
Watanabe H, Adachi W, Koide N, Yazawa I. Food residue at endoscopy in patients who have previously undergone distal gastrectomy: risk factors and patient preparation. Endoscopy. 2003;35:397–401.
Ahn YH, Maturu P, Steinheber FU, Goldman JM. Association of diabetes mellitus with gastric bezoar formation. Arch Intern Med. 1987;147:527–528.
Tohdo H, Haruma K, Kitadai Y, et al. Gastric emptying and bezoars in Japanese: report of five cases. Dig Dis Sci. 1993;38:1422–1425.
Goldstein HM, Cohen LE, Hagan RO, Wells RF. Gastric bezoars: a frequent complication in the postoperative ulcer patient. Radiology. 1973;107:341–344.
Hewitt AN, Levine MS, Rubesin SE, Laufer I. Gastric bezoars: reassessment of clinical and radiologic findings in 19 patients. Br J Radiol. 2009;82:901–907.
Zamir D, Goldblum C, Linova L, Polychuck I, Reitblat T, Yoffe B. Phytobezoars and trichobezoars: a 10-year experience. J Clin Gastroenterol. 2004;38:873–876.
Brady PG. Gastric phytobezoars consequent to delayed gastric emptying. Gastrointest Endosc. 1978;24:159–161.
Buchholz RR, Haisten AS. Phytobezoars following gastric surgery for duodenal ulcer. Surg Clin North Am. 1972;52:341–352.
Myer GW, Clark RD, Brotman M. Gastric phytobezoar and hypoglycemia: medical management. Cal Med. 1973;118:66–67.
Kuiper D. Gastric bezoar in a patient with myotonic dystrophy. Am J Dig Dis. 1971;16:529–534.
Kirks DR, Szemes GC. Autovagotomy and gastric bezoar. Gastroenterology. 1971;61:96–98.
Calabuig R, Navarro S, Carrio I, Artigas V, Mones J, Puig LaCalle J. Gastric emptying and bezoars. Am J Surg. 1989;157:287–290.
Knopp H, Halm U, Lamberts R, et al. Incidental and ablation-induced findings during upper gastrointestinal endoscopy in patients after ablation of atrial fibrillation: a retrospective study of 425 patients. Heart Rhythm. 2014;11:574–578.
Choi SW, Kang SH, Kwon OS, et al. A case of severe gastroparesis: indigestion and weight loss after catheter ablation of atrial fibrillation. PACE. 2012;35:e59–e61.
Tougas G, Eaker EY, Abell TL, et al. Assessment of gastric emptying using a low fat meal: establishment of international control values. Am J Gastroenterol. 2000;95:1456–1462.
Abell TL, Camilleri M, Donohoe K, et al. Consensus recommendations for gastric emptying scintigraphy: a joint report of the American Neurogastroenterology and Motility Society and the Society of Nuclear Medicine. Am J Gastroenterol. 2008;103:753–763.
Abell TL, Bernstein VK, Cutts T, et al. Treatment of gastroparesis: a multidisciplinary clinical review. Neurogastroenterol Motil. 2006;18:263–283.
Kuo B, McCallum RW, Koch KL, et al. Comparison of gastric emptying of a nondigestible capsule to a radio-labelled meal in healthy and gastroparetic subjects. Aliment Pharmacol Ther. 2008;27:186–196.
Rao SS, Camilleri M, Hasler WL, et al. Evaluation of gastrointestinal transit in clinical practice: position paper of the American and European Neurogastroenterology and Motility Societies. Neurogastroenterol Motil. 2011;23:8–23.
Hasler WL, Coleski R, Chey WD, et al. Differences in intragastric pH in diabetic vs. idiopathic gastroparesis: relation to degree of gastric retention. Am J Physiol Gastrointest Liver Physiol. 2008;294:G1384–G1391.
Gaddipati KV, Simonian HP, Kresge KM, Boden GH, Parkman HP. Abnormal ghrelin and pancreatic polypeptide responses in gastroparesis. Dig Dis Sci. 2006;51:1339–1346.
Parkman HP, Yates K, Hasler WL, et al. Similarities and differences between diabetic and idiopathic gastroparesis. Clin Gastroenterol Hepatol. 2011;9:1056–1064.
Park SE, Ahn JY, Jung HY, et al. Clinical outcomes associated with treatment modalities for gastrointestinal bezoars. Gut Liver. 2014;8:400–407.
Wang YG, Seitz U, Li ZL, Soehendra N, Qiao XA. Endoscopic management of huge bezoars. Endoscopy. 1998;30:371–374.
Pasricha PJ, Colvin R, Yates K, et al. Characteristics of patients with chronic unexplained nausea and vomiting and normal gastric emptying. Clin Gastroenterol Hepatol. 2011;9:567–576.
Olausson EA, Alpsten M, Larsson A, Mattsson H, Andersson H, Attvall S. Small particle size of a solid meal increases gastric emptying and late postprandial glycemic response in diabetic subjects with gastroparesis. Diabetes Res Clin Pract. 2008;80:231–237.
Olausson EA, Storsrud S, Grundin H, Isaksson M, Attvall S, Simren M. A small particle size diet reduces upper gastrointestinal symptoms in patients with diabetic gastroparesis: a randomized controlled trial. Am J Gastroenterol. 2014;109:375–385.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict to interest
None.
Rights and permissions
About this article
Cite this article
Coleski, R., Baker, J.R. & Hasler, W.L. Endoscopic Gastric Food Retention in Relation to Scintigraphic Gastric Emptying Delays and Clinical Factors. Dig Dis Sci 61, 2593–2601 (2016). https://doi.org/10.1007/s10620-016-4173-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4173-7