Abstract
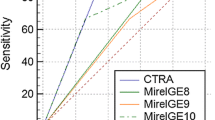
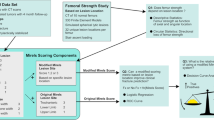
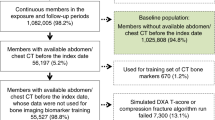
Lower limb pathological fractures caused by bone metastases can severely impair activities of daily living, so recognizing fracture risk is essential. Medial cortical involvement (MCI) in the proximal femur has been demonstrated to affect bone strength in biomechanical studies, but it has not been investigated in real patients. Between 2012 and 2019, 161 bone metastases with computed tomography (CT) images were retrospectively examined. Twenty-nine fractures were observed including 14 metastases with pathological fractures at the first examination, and prophylactic surgery was performed for 50 metastases. We extracted clinicopathological data using CT images, including patient’s background, MCI in the proximal femur, site, size, circumferential cortical involvement (CCI), pain, and nature of metastasis. Cox proportional hazard regression analyses were performed, and we created integer scores for predicting fractures. We revealed that MCI, CCI, lytic dominant lesion, and pain were significant factors by univariate analyses. By multivariable analysis, MCI and each 25% CCI were significant and integer score 1 was assigned based on hazard ratio. The full score was four points, with MCI in the proximal femur (one point) and ≥ 75% CCI (three points). With integer score two, sensitivity was 88.9% and specificity was 81.2% for predicting fracture within 60 days. In conclusion, MCI and CCI examined by CT images were the risk factors for pathological fracture. CCI ≥ 50% is a widely known risk factor, but in addition, it may be better to consider surgery if MCI in the proximal femur is observed in metastasis with 25–50% CCI.




Similar content being viewed by others
Abbreviations
- SREs:
-
Skeletal related events
- ADL:
-
Activities of daily living
- QOL:
-
Quality of life
- MCI:
-
Medial cortical involvement
- BMA:
-
Bone-modifying agent
- CT:
-
Computed tomography
- CRP:
-
C reactive protein
- Alb:
-
Albumin
- CCI:
-
Circumferential cortical involvement
- ROC:
-
Receiver Operating Characteristic
- AUC:
-
Area under the curve
- IQR:
-
Interquartile range
- HR:
-
Hazard ratio
- FE method:
-
Finite element method
References
Maemondo M, Inoue A, Kobayashi K et al (2010) Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 362:2380–2388
Robert C, Long GV, Brady B et al (2015) Nivolumab in previously untreated melanoma without BRAF mutation. N Engl J Med 372:320–330
Hage WD, Aboulafia AJ, Aboulafia DM (2000) Incidence, location, and diagnostic evaluation of metastatic bone disease. Orthop Clin N Am 31:515–528
Hosono N, Yonenobu K, Fuji T, Ebara S, Yamashita K, Ono K (1995) Orthopaedic management of spinal metastases. Clin Orthop Relat Res 312:148–159
Coleman RE (2001) Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev 27:165–167
Shinoda Y, Sawada R, Yoshikawa F et al (2019) Factors related to the quality of life in patients with bone metastases. Clin Exp Metastasis 36:441–448
Ward WG, Holsenbeck S, Dorey FJ, Spang J, Howe D (2003) Metastatic disease of the femur: surgical treatment. Clin Orthop Relat Res 415S:S230–244
Mirels H (1989) Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res 249:256–264
Van der Linden YM, Kroon HM, Dijkstra SP et al (2003) Simple radiographic parameter predicts fracturing in metastatic femoral bone lesions: results from a randomized trial. Radiother Oncol 69:21–31
Keyak JH, Kaneko TS, Skinner HB et al (2007) The effect of simulated metastatic lytic lesions on proximal femoral strength. Clin Orthop Relat Res 459:139–145
Shinoda Y, Kobayashi H, Kaneko M et al (2019) Prediction of the pathological fracture risk during stance and fall-loading configurations for metastases in the proximal femur, using a computed tomography-based finite element method. J Orthop Sci 24:1074–1080
Kawabata Y, Matsuo K, Nezu Y et al (2017) The risk assessment of pathological fracture in the proximal femur using a CT-based finite element method. J Orthop Sci 22:931–937
Sivasundaram R, Shah S, Ahmadi S et al (2013) The biomechanical effect of proximal tumor defect location on femur pathological fractures. J Orthop Trauma 27:e174–e180
Benca E, Reisinger A, Patsch JM et al (2017) Effect of simulated metastatic lesions on the biomechanical behavior of the proximal femur. J Orthop Res 35:2407–2414
Tanck E, van Aken JB, van der Linden YM et al (2009) Pathological fracture prediction in patients with metastatic lesions can be improved with quantitative computed tomography based computer models. Bone 45:777–783
Hamaoka T, Madewell JE, Podoloff DA et al (2004) Bone imaging in metastatic breast cancer. J Clin Oncol 22:2942–2953
Katagiri H, Okada R, Takagi T et al (2014) New prognostic factors and scoring system for patients with skeletal metastasis. Cancer Med 3:1359–1367
Yamaguchi T, Tamai K, Yamato M et al (1996) Intertrabecular pattern of tumors metastatic to bone. Cancer 78:1388–1394
Yamaguchi T (2001) Intertrabecular vertebral metastases: metastases only detectable on MR imaging. Semin Musculoskelet Radiol 5:171–175
Harrington KD (1982) New trends in the management of lower extremity metastases. Clin Orthop Relat Res 169:53–61
Dijkstra PD, Oudkerk M, Wiggers T (1997) Prediction of pathological subtrochanteric fractures due to metastatic lesions. Arch Orthop Trauma Surg 116:221–224
Hirai T, Shinoda Y, Tateishi R (2019) Early detection of bone metastases of hepatocellular carcinoma reduces bone fracture and paralysis. Jpn J Clin Oncol 49:529–536
Fidler M (1981) Incidence of fracture through metastases in long bones. Acta Orthop 52:623–627
Menck H, Schulze S, Larsen E (1988) Metastasis size in pathologic femoral fractures. Acta Orthop 59:151–154
Tatar Z, Soubrier M, Dillies AF et al (2014) Assessment of the risk factors for impending fractures following radiotherapy for long bone metastases using CT scan-based virtual simulation: a retrospective study. Radiat Oncol 9:227
Groenen KH, Pouw MH, Hannink G et al (2016) The effect of radiotherapy, and radiotherapy combined with bisphosphonates or RANK ligand inhibitors on bone quality in bone metastases. A systematic review. Radiother Oncol 119:194–201
Acknowledgment
We would like to thank Editage (www.editage.jp) for English language editing.
Funding
This work was supported by KAKENHI (Grants-in-Aid for Scientific Research (C)) Grant Number 15K10388.
Author information
Authors and Affiliations
Contributions
Conception and design of the study: YS, HK; Collection and assembly of data: YS, RS, YI, TA, LZ, TH, MI, KO, TO; Analysis and interpretation of data: YS, HO, HK; Drafting of the article: YS; Critical revision of the article for important intellectual content: TA, HK, TG, ST; Final approval of the article: NH.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest regarding the publication of this paper.
Ethical approval
This study was conducted according to the ethical guidelines for epidemiological research laid out by the Japanese Ministry of Education, Culture, Sports, Science and Technology, and the Ministry of Health, Labour and Welfare. The study protocol was included in a comprehensive protocol developed by the Department of Rehabilitation and the Department of Orthopaedic Surgery, the University of Tokyo Hospital. The study was approved by the University of Tokyo Medical Research Center Ethics Committee (approval number: 2373).
Consent to participate
All participants were provided a means to opt out.
Availability of data and material
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Shinoda, Y., Sawada, R., Ishibashi, Y. et al. Prediction of pathological fracture in patients with lower limb bone metastasis using computed tomography imaging. Clin Exp Metastasis 37, 607–616 (2020). https://doi.org/10.1007/s10585-020-10053-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-020-10053-z