Abstract
Objective
The purpose of this study was to determine whether the epidermal growth factor receptor (EGFR), which is a classical receptor tyrosine kinase, is involved in the protective effect of morphine against ischemia/reperfusion (I/R)-induced myocardial mitochondrial damage.
Methods
Isolated rats hearts were subjected to global ischemia followed by reperfusion. Cardiac H9c2 cells were exposed to a simulated ischemia solution followed by Tyrode’s solution to induce hypoxia/reoxygenation (H/R) injury. Triphenyltetrazolium chloride (TTC) was used to measure infarct size. The mitochondrial morphological and functional changes were determined using transmission election microscopy (TEM), mitochondrial stress assay, and mitochondrial swelling, respectively. Mitochondrial fluorescence indicator JC-1, DCFH-DA, and Mitosox Red were used to determine mitochondrial membrane potential (△Ψm), intracellular reactive oxygen species (ROS) and mitochondrial superoxide. A TUNUL assay kit was used to detect the level of apoptosis. Western blotting analysis was used to measure the expression of proteins.
Results
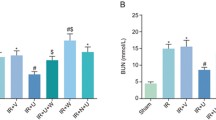
Treatment of isolated rat hearts with morphine prevented I/R-induced myocardial mitochondrial injury, which was inhibited by the selective EGFR inhibitor AG1478, suggesting that EGFR is involved in the mitochondrial protective effect of morphine under I/R conditions. In support of this hypothesis, the selective EGFR agonist epidermal growth factor (EGF) reduced mitochondrial morphological and functional damage similarly to morphine. Further study demonstrated that morphine may alleviate I/R-induced cardiac damage by inhibiting autophagy but not apoptosis. Morphine increased protein kinase B (Akt), extracellular regulated protein kinases (ERK) and signal transducer and activator of transcription-3 (STAT-3) phosphorylation, which was inhibited by AG1478, and EGF had similar effects, indicating that morphine may activate Akt, ERK, and STAT-3 via EGFR. Morphine and EGF increased intracellular reactive oxygen species (ROS) generation. This effect of morphine was inhibited by AG1478, indicating that morphine promotes intracellular ROS generation by activating EGFR. However, morphine did not increase ROS generation when cells were transfected with siRNA against EGFR. In addition, EGFR activity was markedly increased by morphine, but the effect of morphine was reversed by naltrindole. These results suggest that morphine may activate EGFR via δ-opioid receptor activation.
Conclusions
Morphine may prevent I/R-induced myocardial mitochondrial damage by activating EGFR through δ-opioid receptors, in turn increasing RISK and SAFE pathway activity via intracellular ROS. Moreover, morphine may reduce myocardial injury by regulating autophagy but not apoptosis.









Similar content being viewed by others
Availability of data and material
All data, models, or code generated or used during the study are available from the corresponding author by request.
Code Availability
No code was generated or used during the study.
References
Thind GS, Agrawal PR, Hirsh B, Saravolatz L, Chen-Scarabelli C, Narula J, et al. Mechanisms of myocardial ischemia-reperfusion injury and the cytoprotective role of minocycline: scope and limitations. Futur Cardiol. 2015;11(1):61–76.
Huang Z, Han Z, Ye B, Dai Z, Shan P, Lu Z, et al. Berberine alleviates cardiac ischemia/reperfusion injury by inhibiting excessive autophagy in cardiomyocytes. Eur J Pharmacol. 2015;762:1–10.
Chouchani ET, Pell VR, James AM, Work LM, Saeb-Parsy K, Frezza C, et al. A unifying mechanism for mitochondrial superoxide production during ischemia-reperfusion injury. Cell Metab. 2016;23(2):254–63.
Pell VR, Chouchani ET, Murphy MP, Brookes PS, Krieg T. Moving forwards by blocking back-flow: the Yin and Yang of MI therapy. Circ Res. 2016;118(5):898–906.
Wang X, Kong N, Zhou C, Mungun D, Iyan Z, Guo Y, et al. Effect of remote ischemic preconditioning on perioperative cardiac events in patients undergoing elective percutaneous coronary intervention: a meta-analysis of 16 randomized trials. Cardiol Res Pract. 2017;2017:6907167.
Zhao JJ, Xiao H, Zhao WB, Zhang XP, Xiang Y, Ye ZJ, et al. Remote ischemic postconditioning for ischemic stroke: a systematic review and meta-analysis of randomized controlled trials. Chin Med J. 2018;131(8):956–65.
Xi J, Tian W, Zhang L, Jin Y, Xu Z. Morphine prevents the mitochondrial permeability transition pore opening through NO/cGMP/PKG/Zn2+/GSK-3beta signal pathway in cardiomyocytes. Am J Physiol Heart Circ Physiol. 2010;298(2):H601–7.
Kleinbongard P, Heusch G. Extracellular signaling molecules in the ischaemic/reperfused heart - druggable and translatable for cardioprotection? Br J Pharmacol. 2015;172(8):2010–25.
Xu J, Tian W, Ma X, Guo J, Shi Q, Jin Y, et al. The molecular mechanism underlying morphine-induced Akt activation: roles of protein phosphatases and reactive oxygen species. Cell Biochem Biophys. 2011;61(2):303–11.
Zhang X, Simons M. Receptor tyrosine kinases endocytosis in endothelium: biology and signaling. Arterioscler Thromb Vasc Biol. 2014;34(9):1831–7.
Tuuminen R, Dashkevich A, Keranen MA, Raissadati A, Krebs R, Jokinen JJ, et al. Platelet-derived growth factor-B protects rat cardiac allografts from ischemia-reperfusion injury. Transplantation. 2016;100(2):303–13.
Dai W, Kloner RA. Cardioprotection of insulin-like growth factor-1 during reperfusion therapy: what is the underlying mechanism or mechanisms? Circ Cardiovasc Interv. 2011;4(4):311–3.
Dao DT, Anez-Bustillos L, Adam RM, Puder M, Bielenberg DR. Heparin-binding epidermal growth factor-like growth factor as a critical mediator of tissue repair and regeneration. Am J Pathol. 2018;188(11):2446–56.
Russo M, Crisafulli G, Sogari A, Reilly NM, Arena S, Lamba S, et al. Adaptive mutability of colorectal cancers in response to targeted therapies. Science. 2019;366(6472):1473–80.
He H, Huh J, Wang H, Kang Y, Lou J, Xu Z. Mitochondrial events responsible for morphine’s cardioprotection against ischemia/reperfusion injury. Toxicol Appl Pharmacol. 2016;290:66–73.
Zhang Y, Gao J, Sun W, Wen X, Xi Y, Wang Y, et al. H2S restores the cardioprotective effects of ischemic post-conditioning by upregulating HB-EGF/EGFR signaling. Aging (Albany NY). 2019;11(6):1745–58.
Krieg T, Cui L, Qin Q, Cohen MV, Downey JM. Mitochondrial ROS generation following acetylcholine-induced EGF receptor transactivation requires metalloproteinase cleavage of proHB-EGF. J Mol Cell Cardiol. 2004;36(3):435–43.
Deygas M, Gadet R, Gillet G, Rimokh R, Gonzalo P, Mikaelian I. Redox regulation of EGFR steers migration of hypoxic mammary cells towards oxygen. Nat Commun. 2018;9(1):4545.
Wang S, Yao T, Deng F, Yu W, Song Y, Chen J, et al. LncRNA MALAT1 promotes oxygen-glucose deprivation and reoxygenation induced cardiomyocytes injury through sponging miR-20b to enhance beclin1-mediated autophagy. Cardiovasc Drugs Ther. 2019;33(6):675–86.
Stroethoff M, Behmenburg F, Meierkord S, Bunte S, Mayer F, Mathes A, et al. Cardioprotective properties of omecamtiv mecarbil against ischemia and reperfusion injury. J Clin Med. 2019;8(3):375.
Bartekova M, Radosinska J, Pancza D, Barancik M, Ravingerova T. Cardioprotective effects of quercetin against ischemia-reperfusion injury are age-dependent. Physiol Res. 2016;65(Suppl 1):S101–7.
Borshchev YY, Minasian SM, Burovenko IY, Borshchev VY, Protsak ES, Semenova NY, et al. Effects of tetracycline on myocardial infarct size in obese rats with chemically-induced colitis. PLoS One. 2019;14(11):e0225185.
Zhang Y, Xing F, Zheng H, Xi J, Cui X, Xu Z. Roles of mitochondrial Src tyrosine kinase and zinc in nitric oxide-induced cardioprotection against ischemia/reperfusion injury. Free Radic Res. 2013;47(6–7):517–25.
Xu J, Bian X, Liu Y, Hong L, Teng T, Sun Y, et al. Adenosine A2 receptor activation ameliorates mitochondrial oxidative stress upon reperfusion through the posttranslational modification of NDUFV2 subunit of complex I in the heart. Free Radic Biol Med. 2017;106:208–18.
McIntosh R, Lee S, Ghio AJ, Xi J, Zhu M, Shen X, et al. The critical role of intracellular zinc in adenosine A(2) receptor activation induced cardioprotection against reperfusion injury. J Mol Cell Cardiol. 2010;49(1):41–7.
Cheng KC, Chang WT, Kuo FY, Chen ZC, Li Y, Cheng JT. TGR5 activation ameliorates hyperglycemia-induced cardiac hypertrophy in H9c2 cells. Sci Rep. 2019;9(1):3633.
Li W, Fang Q, Zhong P, Chen L, Wang L, Zhang Y, et al. EGFR inhibition blocks palmitic acid-induced inflammation in cardiomyocytes and prevents hyperlipidemia-induced cardiac injury in mice. Sci Rep. 2016;6:24580.
Ye Y, An Y, Wang M, Liu H, Guan L, Wang Z, et al. Expression of carboxypeptidase X M14 family member 2 accelerates the progression of hepatocellular carcinoma via regulation of the gp130/JAK2/Stat1 pathway. Cancer Manag Res. 2020;12:2353–64.
Mdaki KS, Larsen TD, Wachal AL, Schimelpfenig MD, Weaver LJ, Dooyema SD, et al. Maternal high-fat diet impairs cardiac function in offspring of diabetic pregnancy through metabolic stress and mitochondrial dysfunction. Am J Physiol Heart Circ Physiol. 2016;310(6):H681–92.
Sun Y, Zhou K, He M, Gao Y, Zhang D, Bai Y, et al. The effects of different fluorescent indicators in observing the changes of the mitochondrial membrane potential during oxidative stress-induced mitochondrial injury of cardiac H9c2 cells. J Fluoresc. 2020;30(6):1421–30.
Brand MD, Nicholls DG. Assessing mitochondrial dysfunction in cells. Biochem J. 2011;435(2):297–312.
Lee S, Chanoit G, McIntosh R, Zvara DA, Xu Z. Molecular mechanism underlying Akt activation in zinc-induced cardioprotection. Am J Physiol Heart Circ Physiol. 2009;297(2):H569–75.
Levkowitz G, Waterman H, Ettenberg SA, Katz M, Tsygankov AY, Alroy I, et al. Ubiquitin ligase activity and tyrosine phosphorylation underlie suppression of growth factor signaling by c-Cbl/Sli-1. Mol Cell. 1999;4(6):1029–40.
Basmaciyan L, Azas N, Casanova M. Calcein+/PI- as an early apoptotic feature in Leishmania. PLoS One. 2017;12(11):e0187756.
Mo D, Tian W, Zhang HN, Feng YD, Sun Y, Quan W, et al. Cardioprotective effects of galectin-3 inhibition against ischemia/reperfusion injury. Eur J Pharmacol. 2019;863:172701.
Qiao J, Arthur JF, Gardiner EE, Andrews RK, Zeng L, Xu K. Regulation of platelet activation and thrombus formation by reactive oxygen species. Redox Biol. 2018;14:126–30.
Jang Y, Xi J, Wang H, Mueller RA, Norfleet EA, Xu Z. Postconditioning prevents reperfusion injury by activating delta-opioid receptors. Anesthesiology. 2008;108(2):243–50.
Zorov DB, Juhaszova M, Sollott SJ. Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol Rev. 2014;94(3):909–50.
Shi Y, Yuan S, Tang SJ. Reactive oxygen species (ROS) are critical for morphine exacerbation of HIV-1 gp120-induced pain. J NeuroImmune Pharmacol. 2020. https://doi.org/10.1007/s11481-020-09951-6.
Kong H, Jiang CY, Hu L, Teng P, Zhang Y, Pan XX, et al. Morphine induces dysfunction of PINK1/Parkin-mediated mitophagy in spinal cord neurons implying involvement in antinociceptive tolerance. J Mol Cell Biol. 2019;11(12):1056–68.
Delbridge LMD, Mellor KM, Taylor DJ, Gottlieb RA. Myocardial stress and autophagy: mechanisms and potential therapies. Nat Rev Cardiol. 2017;14(7):412–25.
Choura M, Rebai A. Receptor tyrosine kinases: from biology to pathology. J Recept Signal Transduct Res. 2011;31(6):387–94.
Senis YA, Mazharian A, Mori J. Src family kinases: at the forefront of platelet activation. Blood. 2014;124(13):2013–24.
Williams-Pritchard G, Knight M, Hoe LS, Headrick JP, Peart JN. Essential role of EGFR in cardioprotection and signaling responses to A1 adenosine receptors and ischemic preconditioning. Am J Physiol Heart Circ Physiol. 2011;300(6):H2161–8.
Miao Y, Bi XY, Zhao M, Jiang HK, Liu JJ, Li DL, et al. Acetylcholine inhibits tumor necrosis factor alpha activated endoplasmic reticulum apoptotic pathway via EGFR-PI3K signaling in cardiomyocytes. J Cell Physiol. 2015;230(4):767–74.
Barsotti AMG, de Assis VR, Titon SCM, Titon BJ, da Silva Ferreira ZF, Gomes FR. ACTH modulation on corticosterone, melatonin, testosterone and innate immune response in the tree frog Hypsiboas faber. Comp Biochem Physiol A Mol Integr Physiol. 2017;204:177–84.
Russell PS, Beravat R, Wong GK. Helically twisted photonic crystal fibres. Philos Trans A Math Phys Eng Sci. 2017;375(2087):20150440.
Kim H, Lim HY. Novel EGFR-TK inhibitor EKB-569 inhibits hepatocellular carcinoma cell proliferation by AKT and MAPK pathways. J Korean Med Sci. 2011;26(12):1563–8.
Akhtar S, Yousif MH, Chandrasekhar B, Benter IF. Activation of EGFR/ERBB2 via pathways involving ERK1/2, P38 MAPK, AKT and FOXO enhances recovery of diabetic hearts from ischemia-reperfusion injury. PLoS One. 2012;7(6):e39066.
Lu H, Zhang H, Weng ML, Zhang J, Jiang N, Cata JP, et al. Morphine promotes tumorigenesis and cetuximab resistance via EGFR signaling activation in human colorectal cancer. J Cell Physiol. 2021;236(6):4445–54.
Huo Y, Chen W, Zheng X, Zhao J, Zhang Q, Hou Y, et al. The protective effect of EGF-activated ROS in human corneal epithelial cells by inducing mitochondrial autophagy via activation TRPM2. J Cell Physiol. 2020;235(10):7018–29.
Dong Y, Chen H, Gao J, Liu Y, Li J, Wang J. Molecular machinery and interplay of apoptosis and autophagy in coronary heart disease. J Mol Cell Cardiol. 2019;136:27–41.
Mizushima N, Levine B, Cuervo AM, Klionsky DJ. Autophagy fights disease through cellular self-digestion. Nature. 2008;451(7182):1069–75.
Velez DE, Mestre-Cordero VE, Hermann R, Perego J, Harriet S, Fernandez-Pazos MLM, et al. Rosuvastatin protects isolated hearts against ischemia-reperfusion injury: role of Akt-GSK-3beta, metabolic environment, and mitochondrial permeability transition pore. J Physiol Biochem. 2020;76(1):85–98.
Yang S, Li H, Tang L, Ge G, Ma J, Qiao Z, et al. Apelin-13 protects the heart against ischemia-reperfusion injury through the RISK-GSK-3beta-mPTP pathway. Arch Med Sci. 2015;11(5):1065–73.
Zhang G, Sheng M, Wang J, Teng T, Sun Y, Yang Q, et al. Zinc improves mitochondrial respiratory function and prevents mitochondrial ROS generation at reperfusion by phosphorylating STAT3 at Ser(727). J Mol Cell Cardiol. 2018;118:169–82.
Philipp S, Cui L, Ludolph B, Kelm M, Schulz R, Cohen MV, et al. Desferoxamine and ethyl-3,4-dihydroxybenzoate protect myocardium by activating NOS and generating mitochondrial ROS. Am J Physiol Heart Circ Physiol. 2006;290(1):H450–7.
Zhang X, Saarinen AM, Hitosugi T, Wang Z, Wang L, Ho TH, et al. Inhibition of intracellular lipolysis promotes human cancer cell adaptation to hypoxia. Elife. 2017; 6:e31132.
Li L, Tan J, Miao Y, Lei P, Zhang Q. ROS and autophagy: interactions and molecular regulatory mechanisms. Cell Mol Neurobiol. 2015;35(5):615–21.
Pinegin B, Vorobjeva N, Pashenkov M, Chernyak B. The role of mitochondrial ROS in antibacterial immunity. J Cell Physiol. 2018;233(5):3745–54.
Pashkovskaia N, Gey U, Rodel G. Mitochondrial ROS direct the differentiation of murine pluripotent P19 cells. Stem Cell Res. 2018;30:180–91.
Stefanatos R, Sanz A. The role of mitochondrial ROS in the aging brain. FEBS Lett. 2018;592(5):743–58.
Stowe DF, Camara AK. Mitochondrial reactive oxygen species production in excitable cells: modulators of mitochondrial and cell function. Antioxid Redox Signal. 2009;11(6):1373–414.
Zuo L, Zhou T, Pannell BK, Ziegler AC, Best TM. Biological and physiological role of reactive oxygen species--the good, the bad and the ugly. Acta Physiol (Oxford). 2015;214(3):329–48.
Biscardi JS, Maa MC, Tice DA, Cox ME, Leu TH, Parsons SJ. c-Src-mediated phosphorylation of the epidermal growth factor receptor on Tyr845 and Tyr1101 is associated with modulation of receptor function. J Biol Chem. 1999;274(12):8335–43.
Acknowledgments
We gratefully acknowledge Prof. Zhelong Xu from Tianjin Medical University for technical guidance. We thank Springer Nature Author Services for its linguistic assistance during the preparation of this manuscript.
Funding
This work was supported by grant 81700324 from the National Natural Science Foundation of China, grant H2018209378 from the Hebei Provincial Science Foundation of China and grant BJ2018055 from the Hebei Provincial Education Hall Top Talent Project of China.
Author information
Authors and Affiliations
Contributions
Wei Tian and Jingman Xu conceived, designed, and carried out the experiments; analyzed the data; and wrote the paper. Xiyun Bian was responsible for taking pictures using TEM and laser scanning confocal microscopy. Huanhuan Zhao performed the experimental model setting and statistical analysis. Yujie Sun and Xiaodong Li helped with cell culture. Yanyi Tian helped with the western blot and apoptosis test.
Corresponding authors
Ethics declarations
Ethics Approval
The animal experiments were approved by the ethics committee of North China University of Science and Technology (application approval number 2017023). This study conforms to the NIH Guide for the Care and Use of Laboratory Animals (NIH publication No. 85–23, revised 1996).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(JPG 1088 kb)
Rights and permissions
About this article
Cite this article
Xu, J., Bian, X., Zhao, H. et al. Morphine Prevents Ischemia/Reperfusion-Induced Myocardial Mitochondrial Damage by Activating δ-opioid Receptor/EGFR/ROS Pathway. Cardiovasc Drugs Ther 36, 841–857 (2022). https://doi.org/10.1007/s10557-021-07215-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-021-07215-w