Abstract
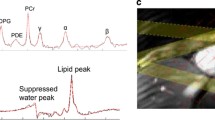
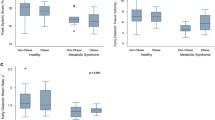
A reduced myocardial phosphocreatine/adenosine triphosphate (PCr/ATP) ratio is linked to both diastolic dysfunction and heart failure. Although obesity is well known to cause diastolic dysfunction a link to impaired cardiac energetics has only recently been established. We assessed whether or not long-term weight loss in obesity, which is known to reduce mortality, is accompanied by both improved cardiac energetics and diastolic function. Normal weight (BMI 22 ± 2; n = 18) and obese subjects (BMI 34 ± 4; n = 13) underwent cine-MRI (1.5 Tesla) to determine left ventricular diastolic function using volume-time curve analysis, and 31P-MR spectroscopy (3 Tesla) to assess cardiac energetics (PCr/ATP ratio). Obese subjects (n = 13) underwent repeat assessment after 1 year of supervised weight loss. Obesity, in the absence of identifiable cardiovascular risk factors, was associated with significantly impaired myocardial high energy phosphate metabolism (PCr/ATP ratio, normal; 2.03 ± 0.27 vs. obese; 1.58 ± 0.47, p = 0.002) and significantly lower peak diastolic filling rate (normal; 4.8 ± 0.8 vs. obese; 3.8 ± 0.7 EDV/s, p = 0.01). Weight loss (on average 9 kg, 55 % excess weight) over 1 year resulted in a 24 % increase in PCr/ATP ratio (p = 0.01) and an 18 % improvement in peak diastolic filling rate (p = 0.01). Myocardial PCr/ATP ratio remained positively correlated with peak diastolic filling rate after weight loss (r = 0.63, p = 0.02). In obesity, weight loss improves impaired cardiac energetics and myocardial relaxation. Improved myocardial energetics appear to play a key role in diastolic functional recovery accompanying weight loss.



Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Neubauer S (2007) The failing heart—an engine out of fuel. N Engl J Med 356(11):1140–1151
Ashrafian H, Frenneaux MP, Opie LH (2007) Metabolic mechanisms in heart failure. Circulation 116(4):434–448. doi:10.1161/CIRCULATIONAHA.107.702795
Opie LH (1971) Substrate utilization and glycolysis in the heart. Cardiology 56(1):2–21
Varma N, Eberli FR, Apstein CS (2000) Increased diastolic chamber stiffness during demand ischemia: response to quick length change differentiates rigor-activated from calcium-activated tension. Circulation 101(18):2185–2192
Diamant M, Lamb HJ, Groeneveld Y, Endert EL, Smit JW, Bax JJ, Romijn JA, de Roos A, Radder JK (2003) Diastolic dysfunction is associated with altered myocardial metabolism in asymptomatic normotensive patients with well-controlled type 2 diabetes mellitus. J Am Coll Cardiol 42(2):328–335
Grossman W, Momomura SI, Ingwall JS (1987) Diastolic relaxation abnormalities during ischaemia and their association with high energy phosphate depletion, intracellular pH and myocardial blood flow. Basic Res Cardiol 82(Suppl 2):289–299
Lamb HJ, Beyerbacht HP, van der Laarse A, Stoel BC, Doornbos J, van der Wall EE, de Roos A (1999) Diastolic dysfunction in hypertensive heart disease is associated with altered myocardial metabolism. Circulation 99(17):2261–2267
Neubauer S, Horn M, Cramer M, Harre K, Newell JB, Peters W, Pabst T, Ertl G, Hahn D, Ingwall JS, Kochsiek K (1997) Myocardial phosphocreatine-to-ATP ratio is a predictor of mortality in patients with dilated cardiomyopathy. Circulation 96(7):2190–2196
Rider OJ, Francis JM, Ali MK, Holloway C, Pegg T, Robson MD, Tyler D, Byrne J, Clarke K, Neubauer S (2012) Effects of catecholamine stress on diastolic function and myocardial energetics in obesity. Circulation 125(12):1511–1519. doi:10.1161/CIRCULATIONAHA.111.069518
Otto ME, Belohlavek M, Khandheria B, Gilman G, Svatikova A, Somers V (2004) Comparison of right and left ventricular function in obese and nonobese men. Am J Cardiol 93(12):1569–1572
Peterson LR, Waggoner AD, Schechtman KB, Meyer T, Gropler RJ, Barzilai B, Davila-Roman VG (2004) Alterations in left ventricular structure and function in young healthy obese women: assessment by echocardiography and tissue Doppler imaging. J Am Coll Cardiol 43(8):1399–1404
Rider OJ, Francis JM, Ali MK, Petersen SE, Robinson M, Robson MD, Byrne JP, Clarke K, Neubauer S (2009) Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J Am Coll Cardiol 54(8):718–726. doi:10.1016/j.jacc.2009.02.086
Bhatia RS, Tu JV, Lee DS, Austin PC, Fang J, Haouzi A, Gong Y, Liu PP (2006) Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med 355(3):260–269
Aljaroudi W, Alraies MC, Halley C, Rodriguez L, Grimm RA, Thomas JD, Jaber WA (2012) Impact of progression of diastolic dysfunction on mortality in patients with normal ejection fraction. Circulation 125(6):782–788. doi:10.1161/CIRCULATIONAHA.111.066423
Adams TD, Gress RE, Smith SC, Halverson RC, Simper SC, Rosamond WD, Lamonte MJ, Stroup AM, Hunt SC (2007) Long-term mortality after gastric bypass surgery. N Engl J Med 357(8):753–761. doi:10.1056/NEJMoa066603
Peterson LR, Herrero P, Schechtman KB, Racette SB, Waggoner AD, Kisrieva-Ware Z, Dence C, Klein S, Marsala J, Meyer T, Gropler RJ (2004) Effect of obesity and insulin resistance on myocardial substrate metabolism and efficiency in young women. Circulation 109(18):2191–2196
Lamb HJ, Beyerbacht HP, Ouwerkerk R, Doornbos J, Pluim BM, van der Wall EE, van der Laarse A, de Roos A (1997) Metabolic response of normal human myocardium to high-dose atropine-dobutamine stress studied by 31P-MRS. Circulation 96(9):2969–2977
Pluim BM, Lamb HJ, Kayser HW, Leujes F, Beyerbacht HP, Zwinderman AH, van der Laarse A, Vliegen HW, de Roos A, van der Wall EE (1998) Functional and metabolic evaluation of the athlete’s heart by magnetic resonance imaging and dobutamine stress magnetic resonance spectroscopy. Circulation 97(7):666–672
Boudina S, Sena S, Theobald H, Sheng X, Wright JJ, Hu XX, Aziz S, Johnson JI, Bugger H, Zaha VG, Abel ED (2007) Mitochondrial energetics in the heart in obesity-related diabetes: direct evidence for increased uncoupled respiration and activation of uncoupling proteins. Diabetes 56(10):2457–2466
Hudsmith LE, Tyler DJ, Emmanuel Y, Petersen SE, Francis JM, Watkins H, Clarke K, Robson MD, Neubauer S (2009) (31)P cardiac magnetic resonance spectroscopy during leg exercise at 3 Tesla. Int J Cardiovasc Imaging 25(8):819–826. doi:10.1007/s10554-009-9492-8
Rider OJ, Lewandowski A, Nethononda R, Petersen SE, Francis JM, Pitcher A, Holloway CJ, Dass S, Banerjee R, Byrne JP, Leeson P, Neubauer S (2012) Gender-specific differences in left ventricular remodelling in obesity: insights from cardiovascular magnetic resonance imaging. Eur Heart J. doi:10.1093/eurheartj/ehs341
Karamitsos TD, Arnold JR, Rider OJ, Francis JM, Ferrett C, Neubauer S, Becher H (2009) Massive hiatus hernia impeding transoesophageal echocardiography in a patient with swallow-syncope syndrome. Hellenic J Cardiol 50(3):216–217
Zeidan Z, Erbel R, Barkhausen J, Hunold P, Bartel T, Buck T (2003) Analysis of global systolic and diastolic left ventricular performance using volume-time curves by real-time three-dimensional echocardiography. J Am Soc Echocardiogr 16(1):29–37. doi:10.1067/mje.2003.40
Scheuermann-Freestone M, Madsen PL, Manners D, Blamire AM, Buckingham RE, Styles P, Radda GK, Neubauer S, Clarke K (2003) Abnormal cardiac and skeletal muscle energy metabolism in patients with type 2 diabetes. Circulation 107(24):3040–3046
Duncan MH, Singh BM, Wise PH, Carter G, Alaghband-Zadeh J (1995) A simple measure of insulin resistance. Lancet 346(8967):120–121
Tintera J, Harantova P, Suchanek P, Dvorakova A, Adamova M, Hajek M, Poledne R (2004) Quantification of intra-abdominal fat during controlled weight reduction: assessment using the water-suppressed breath-hold MRI technique. Physiol Res 53(2):229–234
Knaapen P, Germans T, Knuuti J, Paulus WJ, Dijkmans PA, Allaart CP, Lammertsma AA, Visser FC (2007) Myocardial energetics and efficiency: current status of the noninvasive approach. Circulation 115(7):918–927. doi:10.1161/CIRCULATIONAHA.106.660639
Taegtmeyer H (1994) Energy metabolism of the heart: from basic concepts to clinical applications. Curr Probl Cardiol 19(2):59–113
Ashrafian H, le Roux CW, Darzi A, Athanasiou T (2008) Effects of bariatric surgery on cardiovascular function. Circulation 118(20):2091–2102. doi:10.1161/CIRCULATIONAHA.107.721027
Ritov VB, Menshikova EV, He J, Ferrell RE, Goodpaster BH, Kelley DE (2005) Deficiency of subsarcolemmal mitochondria in obesity and type 2 diabetes. Diabetes 54(1):8–14
Chanseaume E, Barquissau V, Salles J, Aucouturier J, Patrac V, Giraudet C, Gryson C, Duche P, Boirie Y, Chardigny JM, Morio B (2010) Muscle mitochondrial oxidative phosphorylation activity, but not content, is altered with abdominal obesity in sedentary men: synergism with changes in insulin sensitivity. J Clin Endocrinol Metab 95(6):2948–2956. doi:10.1210/jc.2009-1938
Utz W, Engeli S, Haufe S, Kast P, Bohnke J, Haas V, Hermsdorf M, Wiesner S, Pofahl M, Traber J, Luft FC, Boschmann M, Jordan J, Schulz-Menger J (2012) Moderate dietary weight loss reduces myocardial steatosis in obese and overweight women. Int J Cardiol. doi:10.1016/j.ijcard.2012.03.104
Bakermans AJ, Geraedts TR, van Weeghel M, Denis S, Ferraz MJ, Aerts JMFG, Aten J, Nicolay K, Houten SM, Prompers JJ (2011) Fasting-induced myocardial lipid accumulation in long-chain acyl-CoA dehydrogenase knockout mice is accompanied by impaired left ventricular function. Circ Cardiovasc Imaging 4(5):558–565. doi:10.1161/Circimaging.111.963751
Acknowledgments
The study was supported by a grant from the Wellcome Trust and by the Oxford Partnership Comprehensive Biomedical Research Centre with funding from the Department of Health’s NIHR Biomedical Research Centres funding scheme. SN acknowledges support from the Oxford BHF Centre of Research Excellence.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rider, O.J., Francis, J.M., Tyler, D. et al. Effects of weight loss on myocardial energetics and diastolic function in obesity. Int J Cardiovasc Imaging 29, 1043–1050 (2013). https://doi.org/10.1007/s10554-012-0174-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-012-0174-6