Abstract
Purpose
Theoretical frameworks are useful tools to explain the dynamics of behavioral change, develop, and implement intervention studies. The purpose of this systematic review and meta-analysis is to evaluate the application of theoretical frameworks and models to HPV vaccination intervention studies in the United States (US) from January 2006 to December 2019.
Methods
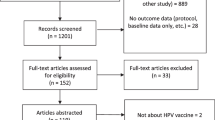
A comprehensive search across databases, including PubMed, EMBASE, ERIC, CINAHL, Academic Search Complete, Scopus, Web of Science, and PsycINFO, was conducted. Articles were included in the systematic analysis if at least one theory was used to develop the intervention phase. All intervention studies targeting populations in the US without restrictions of age, income, sex, and ethnicity were included. Articles were included in the meta-analysis if vaccine uptake and/or vaccine completion was addressed.
Results
The Health Belief Model, Motivational Interviewing, Theory of Planned Behavior, and Information–Motivation–Behavioral Skills were the most used theories. Based on theory integrity, theory rationale, and theory operationalization, most of the studies (60%) were rated high for the application of the theoretical frameworks. Our results suggest a preference for theoretical frameworks targeting individual change rather than community change and the existence of gender disparities in the application of theoretical frameworks. The association between theory and increase of likelihood in vaccine uptake and completion was not supported.
Conclusion
This review spotlights common issues in the application of theoretical frameworks in HPV vaccine interventions in the US. Our results suggest we are still in a developmental phase on several aspects of theory application to HPV vaccination.





Similar content being viewed by others
Data availability
As this is a systematic review and meta-analysis, this is not applicable. Data used are available in the published papers included in their respective journals.
Code availability
Not applicable.
References
Centers for Disease Control and Prevention (2019) About HPV. Available at https://www.cdc.gov/hpv/index.html. Accessed 10 May, 2019
World Health Organization (2017) Human papillomavirus vaccines: WHO position paper, May 2017-recommendations. Vaccine 35(43):5753–5755. https://doi.org/10.1016/j.vaccine.2017.05.069
Centers for Disease Control and Prevention (2019) Human papillomavirus vaccination for adults: updated recommendations of the Advisory Committee on immunization practices. Available at https://www.cdc.gov/mmwr/volumes/68/wr/mm6832a3.htm. Accessed 27 Mar, 2021
Peterson CE, Dykens JA, Brewer NT, Buscemi J, Watson K, Comer-Hagans D, Ramamonjiarivelo Z, Fitzgibbon M (2016) Society of behavioral medicine supports increasing HPV vaccination uptake: an urgent opportunity for cancer prevention. Transl Behav Med 6(4):672–675. https://doi.org/10.1007/s13142-016-0441-5
Healthy people 2020 (2019) Immunization and infectious diseases. Available at https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives. Accessed 23 Aug, 2019
National Library of Medicine (2018) Strengthening the effectiveness of National, State, and local efforts to improve HPV vaccination coverage in the United States: recommendations from the National Vaccine Advisory Committee. Public Health Rep 133(5):543–550. https://doi.org/10.1177/0033354918793629
Glanz K, Rimer BK, Viswanath K (2015) Health behavior: theory, research, and practice, 5th edn. Wiley, New York
European Centre for Disease Prevention and Control (2013) Systematic literature review to examine the evidence for the effectiveness of interventions that use theories and models of behaviour change: towards the prevention and control of communicable diseases: insights into health communication. Luxembourg. https://doi.org/10.2900/73931
Priest HM, Knowlden AP (2015) Systematic review of primary prevention human papillomavirus interventions targeting college students. Int J Sex Health 27(2):1–20. https://doi.org/10.1080/19317611.2014.945631
Allen JD, Coronado GD, Williams RS, Glenn B, Escoffery C, Fernandez M, Tuff RA, Wilson KM, Mullen PD (2010) A systematic review of measures used in studies of human papillomavirus (HPV) vaccine acceptability. Vaccine 28(24):4027–4037. https://doi.org/10.1016/j.vaccine.2010.03.063
Fu LY, Bonhomme L-A, Cooper SC, Joseph JG, Zimet GD (2014) Educational interventions to increase HPV vaccination acceptance: a systematic review. Vaccine 32(17):1901–1920. https://doi.org/10.1016/j.vaccine.2014.01.091
Walling EB, Benzoni N, Dornfeld J, Bhandari R, Sisk BA, Garbutt J, Colditz G (2016) Interventions to improve HPV vaccine uptake: a systematic review. Pediatrics 138(1):e20153863. https://doi.org/10.1542/peds.2015-3863
Smulian EA, Mitchell KR, Stokley S (2016) Interventions to increase HPV vaccination coverage: a systematic review. Hum Vaccines Immunother 12:1566. https://doi.org/10.1080/21645515.2015.1125055
Mrklas KJ, Macdonald S, Shea-Budgell MA, Bedingfield N, Ganshorn H, Glaze S, Bill L, Healy B, Healy C, Guichon J, Colquhoun A, Bell C, Richardson R, Henderson R, Kellner J, Barnabe C, Bednarczyk RA, Letendre A, Nelson GS (2018) Barriers, supports, and effective interventions for uptake of human papillomavirus- and other vaccines within global and Canadian Indigenous peoples: a systematic review protocol. Syst Rev 7(1):40–40. https://doi.org/10.1186/s13643-018-0692-y
Francis DB, Cates JR, Wagner KPG, Zola T, Fitter JE, Coyne-Beasley T (2017) Communication technologies to improve HPV vaccination initiation and completion: a systematic review. Patient Educ Couns 100(7):1280–1286. https://doi.org/10.1016/j.pec.2017.02.004
Niccolai LM, Hansen CE (2015) Practice- and community-based interventions to increase human papillomavirus vaccine coverage: a systematic review. JAMA Pediatr 169(7):686–692. https://doi.org/10.1001/jamapediatrics.2015.0310
Brewer NT, Fazekas KI (2007) Predictors of HPV vaccine acceptability: a theory-informed, systematic review. Prev Med 45(2–3):107–114. https://doi.org/10.1016/j.ypmed.2007.05.013
Ferrer HB, Audrey S, Trotter C, Hickman M (2015) An appraisal of theoretical approaches to examining behaviours in relation to Human Papillomavirus (HPV) vaccination of young women. Prev Med 81:122
Ratanasiripong NT (2012) A review of human papillomavirus (HPV) infection and HPV vaccine-related attitudes and sexual behaviors among college-aged women in the United States. J Am Coll Health 60(6):461–470. https://doi.org/10.1080/07448481.2012.684365
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clin Res Ed) 339(7716):b2535–b2535. https://doi.org/10.1136/bmj.b2535
Lockhart S, Dempsey AF, Pyrzanowski J, O’Leary ST, Barnard JG (2018) Provider and parent perspectives on enhanced communication tools for human papillomavirus vaccine-hesitant parents. Acad Pediatr 18(7):776–782. https://doi.org/10.1016/j.acap.2018.05.012
Gerend MA, Shepherd JE (2012) Predicting human papillomavirus vaccine uptake in young adult women: comparing the health belief model and theory of planned behavior. Ann Behav Med Publ Soc Behav Med 44(2):171–180. https://doi.org/10.1007/s12160-012-9366-5
Sanderson M, Canedo JR, Khabele D, Fadden MK, Harris C, Beard K, Burress M, Pinkerton H, Jackson C, Mayo-Gamble T, Hargreaves MK, Hull PC (2017) Pragmatic trial of an intervention to increase human papillomavirus vaccination in safety-net clinics. BMC Public Health 17(1):158. https://doi.org/10.1186/s12889-017-4094-1
Gerend MA, Shepherd MA, Lustria MLA (2013) Increasing human papillomavirus vaccine acceptability by tailoring messages to young adult women’s perceived barriers. Sex Transm Dis 40(5):401–405. https://doi.org/10.1097/OLQ.0b013e318283c8a8
Chan A, Brown B, Sepulveda E, Teran-Clayton L (2015) Evaluation of fotonovela to increase human papillomavirus vaccine knowledge, attitudes, and intentions in a low-income Hispanic community. BMC Res Notes 8:615. https://doi.org/10.1186/s13104-015-1609-7
Hopfer S, Hopfer S (2012) Effects of a narrative HPV vaccination intervention aimed at reaching college women: a randomized controlled trial. Prev Sci 13(2):173–182. https://doi.org/10.1007/s11121-011-0254-1
Gargano LM, Herbert NL, Painter JE, Sales JM, Vogt TM, Morfaw C, Jones LM, Murray D, DiClemente RJ, Hughes JM (2014) Development, theoretical framework, and evaluation of a parent and teacher-delivered intervention on adolescent vaccination. Health Promot Pract 15(4):556–567. https://doi.org/10.1177/1524839913518222
Spleen AM, Kluhsman BC, Clark AD, Dignan MB, Lengerich EJ, Force AHCT (2012) An increase in HPV-related knowledge and vaccination intent among parental and non-parental caregivers of adolescent girls, age 9–17 years, in Appalachian Pennsylvania. J Cancer Educ Off J Am Assoc Cancer Educ 27(2):312–319. https://doi.org/10.1007/s13187-011-0294-z
Cassidy B, Braxter B, Charron-Prochownik D, Schlenk EA (2014) A quality improvement initiative to increase HPV vaccine rates using an educational and reminder strategy with parents of preteen girls. J Pediatr Health Care Off Publ Natl Assoc Pediatr Nurse Assoc Pract 28(2):155–164. https://doi.org/10.1016/j.pedhc.2013.01.002
Vanderpool RC, Cohen E, Crosby RA, Jones MG, Bates W, Casey BR, Collins T (2013) “1-2-3 Pap” intervention improves HPV vaccine series completion among Appalachian women. J Commun 63(1):95–115. https://doi.org/10.1111/jcom.12001
Reno JE, O’Leary ST, Pyrzanowski J, Lockhart S, Thomas J, Dempsey AF (2018) Evaluation of the implementation of a multicomponent intervention to improve health care provider communication about human papillomavirus vaccination. Acad Pediatr 18(8):882–888. https://doi.org/10.1016/j.acap.2018.08.004
Lee H, Kim M, Cooley ME, Kiang PNC, Kim D, Tang S, Shi L, Thiem L, Kan P, Peou S, Touch C, Chea P, Allison J (2018) Using narrative intervention for HPV vaccine behavior change among Khmer mothers and daughters: a pilot RCT to examine feasibility, acceptability, and preliminary effectiveness. Appl Nurs Res 40:51–60. https://doi.org/10.1016/j.apnr.2017.12.008
Malo TL, Hall ME, Brewer NT, Lathren CR, Gilkey MB (2018) Why is announcement training more effective than conversation training for introducing HPV vaccination? A theory-based investigation. Implement Sci IS 13(1):57. https://doi.org/10.1186/s13012-018-0743-8
Diclemente RJ, Murray CC, Graham T, Still J (2015) Overcoming barriers to HPV vaccination: a randomized clinical trial of a culturally-tailored, media intervention among African American girls. Hum Vaccin Immunother 11(12):2883–2894. https://doi.org/10.1080/21645515.2015.1070996
Sweeney JB, McAnulty RD, Reeve C, Cann A (2015) An intervention for HPV risk reduction based on the theory of planned behavior: an exploratory study with college-aged women. Am J Sex Educ 10(3):199–217
Mehta P, Sharma M, Lee RC (2013) Designing and evaluating a health belief model-based intervention to increase intent of HPV vaccination among College Males. Int Q Community Health Educ 34(1):101–117. https://doi.org/10.2190/IQ.34.1.h
Carcioppolo N, Jensen JD, Wilson SR, Collins WB, Carrion M, Linnemeier G (2013) Examining HPV threat-to-efficacy ratios in the extended parallel process model. Health Commun 28(1):20–28. https://doi.org/10.1080/10410236.2012.719478
Hee Yun L, Koopmeiners JS, McHugh J, Raveis VH, Ahluwalia JS (2016) mHealth Pilot study: text messaging intervention to promote HPV vaccination. Am J Health Behav 40(1):67–76. https://doi.org/10.5993/AJHB.40.1.8
Molokwu J, Dwivedi A, Mallawaarachchi I, Hernandez A, Shokar N, Mallawaarach I (2019) Tiempo de Vacunarte (time to get vaccinated): outcomes of an intervention to improve HPV vaccination rates in a predominantly Hispanic community. Prev Med 121:115–120. https://doi.org/10.1016/j.ypmed.2019.02.004
Reno JE, O’Leary S, Garrett K, Pyrzanowski J, Lockhart S, Campagna E, Barnard J, Dempsey AF (2018) Improving provider communication about HPV vaccines for vaccine-hesitant parents through the use of motivational interviewing. J Health Commun 23(4):313–320. https://doi.org/10.1080/10810730.2018.1442530
National Collaborating Centre for Methods and Tools (2019) Quality assessment tool for quantitative studies method. Available at https://www.nccmt.ca/knowledge-repositories/search/15. Accessed 23 Nov, 2019
Michie S, Prestwich A (2010) Are interventions theory-based? Development of a theory coding scheme. Health Psychol 29(1):1–8. https://doi.org/10.1037/a0016939
Evans WD, Blitstein J, Hersey JC, Renaud J, Yaroch AL (2008) Systematic review of public health branding. J Health Commun 13(8):721–741. https://doi.org/10.1080/10810730802487364
Centers for Disease Control and Prevention (2011) Recommendations on the use of quadrivalent human papillomavirus vaccine in males—Advisory Committee on Immunization Practices (ACIP), 2011. Available at https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6050a3.htm. Accessed 30 Aug, 2019
Jin PF, Prestage CG, Kippax MS, Pell JC, Donovan MB, Templeton ED, Kaldor EJ, Grulich EA (2007) Risk factors for genital and anal warts in a prospective cohort of HIV-negative homosexual men: the HIM study. Sex Transm Dis 34(7):488–493. https://doi.org/10.1097/01.olq.0000245960.52668.e5
Chin-Hong PV, Palefsky JM (2002) Natural history and clinical management of anal human papillomavirus disease in men and women infected with human immunodeficiency virus. Clin Infect Dis Off Publ Infect Dis Soc Am 35(9):1127–1134. https://doi.org/10.1086/344057
Machalek D, Poynten M, Jin FY, Fairley C, Farnsworth A, Garland SM, Hillman R, Petoumenos K, Roberts J, Tabrizi S, Templeton D, Grulich AE (2012) Anal human papillomavirus infection and associated neoplastic lesions in men who have sex with men: a systematic review and meta-analysis. Lancet Oncol 13(5):487–500. https://doi.org/10.1016/S1470-2045(12)70080-3
Painter J, Borba C, Hynes M, Mays D, Glanz K (2008) The use of theory in health behavior research from 2000 to 2005: a systematic review. Ann Behav Med 35(3):358–362. https://doi.org/10.1007/s12160-008-9042-y
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
CCC conceptualized and designed the project, conducted data collection, data analysis, and interpretation, and wrote the first draft. MP conducted data analysis and interpretation and contributed to the manuscript writing. MA oversaw the project and contributed with critical revision of the manuscript for important intellectual content. All authors contributed with critical revision of the manuscript for important intellectual content. All authors attest they meet the ICMJE criteria for authorship.
Corresponding author
Ethics declarations
Conflict of interests
The authors declare they have no affiliations or involvement in an organization or entity with a financial or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors grant consent over all information in this article to be published and disseminated at the journal’s best convenience.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cotache-Condor, C., Peterson, M. & Asare, M. Application of theoretical frameworks on human papillomavirus vaccine interventions in the United States: systematic review and meta-analysis. Cancer Causes Control 33, 15–24 (2022). https://doi.org/10.1007/s10552-021-01509-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-021-01509-y