Abstract
Purpose
Suboptimal diet is a preventable cause of cancer. We aimed to estimate the economic burden of diet-associated cancer among US adults.
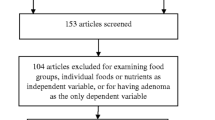
Methods
We used a Comparative Risk Assessment model to quantify the number of new cancer cases attributable to seven dietary factors among US adults ages 20 + years. A Markov cohort model estimated the 5-year medical costs for 15 diet-associated cancers diagnosed in 2015. We obtained dietary intake from 2013 to 2016 National Health and Nutrition Examination Survey, cancer incidence, and survival from 2008 to 2014 Surveillance, Epidemiology, and End Results (SEER) program, and medical costs from 2007 to 2013 linked SEER-Medicare data.
Results
The estimated 5-year medical costs of new diet-associated cancer cases diagnosed in 2015 were $7.44 (2018 US$). Colorectal cancer had the largest diet-related 5-year medical costs of $5.32B. Suboptimal consumption of whole grains ($2.76B), dairy ($1.82B), and high consumption of processed meats ($1.5B) accounted for the highest medical costs. Per-person medical costs attributable to suboptimal diet vary by gender, race, and age group.
Conclusions
Suboptimal diet contributes substantially to the economic burden of diet-associated cancers among US adults. This study highlights the need to implement population-based strategies to improve diet and reduce cancer burden in the US.
Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
The codes used during the current study are available from the corresponding author on reasonable request.
References
Warren JL, Yabroff KR, Meekins A, Topor M, Lamont EB, Brown ML (2008) Evaluation of trends in the cost of initial cancer treatment. J Natl Cancer Inst 100(12):888–897
Mariotto AB, Yabroff RK, Shao Y, Feuer EJ, Brown ML (2011) Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst 103(2):117–128
Winn AN, Ekwueme DU, Guy GP, Neumann PJ (2016) Cost-utility analysis of cancer prevention, treatment, and control. Am J Prev Med 50(2):241–248
Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE, Mullany E et al (2018) The state of US health, 1990–2016: burden of diseases, injuries, and risk factors among US states. JAMA 319(14):1444–1472
World Cancer Research Fund/American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective: Amer Inst for Cancer Research; 2007.
Zhang FF, Cudhea F, Shan Z, Michaud DS, Imamura F, Eom H et al (2019) preventable cancer burden associated with poor diet in the United States. JNCI Cancer Spectrum. https://doi.org/10.1093/jncics/pkz034
(NCHS). CfDCaPCNCfHS. National Health and Nutrition Examination Survey Data. In: Department of Health and Human Services CfDCaP, editor. Hyattsville, MD2013–2014 and 2015–2016.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H et al (2012) A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet 380(9859):2224–2260
World Cancer Research Fund International. Continuous Update Project 2018 [Available from: https://wcrf.org/int/continuous-update-project/about-continuous-update-project.
Udwadia F, Singh S (2019) Starting the conversation: CRISPR’s role in India. Indian J Med Ethics 4:300–303
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K (2016) Body fatness and cancer-viewpoint of the IARC working group. N Engl J Med 375(8):794–798
National Cancer Institute Surveillance Epidemiology and End Results Program. Registry Groupings in SEER Data and Statistics 2018 [Available from: https://seer.cancer.gov/registries/terms.html.
National Cancer Institute Surveillance Epidemiology and End Results Program. ICD-0–3 SEER SITE/HISTOLOGY VALIDATION LIST 2018 [Available from: https://seer.cancer.gov/icd-o-3/sitetype.icdo3.20180117.pdf.
Mariotto AB, Warren JL, Zeruto C, Coughlan D, Barrett MJ, Zhao L et al (2020) Cancer-attributable medical costs for colorectal cancer patients by phases of care: what is the effect of a prior cancer history? JNCI Monographs 2020(55):22–30
Mariotto AB, Robin Yabroff K, Shao Y, Feuer EJ, Brown ML (2011) Projections of the cost of cancer care in the United States: 2010–2020. J Natl Cancer Inst 103(2):117–128
Yabroff KR, Lamont EB, Mariotto A, Warren JL, Topor M, Meekins A et al (2008) Cost of care for elderly cancer patients in the United States. J Natl Cancer Inst 100(9):630–641
Brown ML, Riley GF, Schussler N, Etzioni R. Estimating health care costs related to cancer treatment from SEER-Medicare data. Medical care. 2002; 40:IV104-IV17.
Fireman BH, Quesenberry CP, Somkin CP, Jacobson AS, Baer D, West D et al (1997) Cost of care for cancer in a health maintenance organization 18(4):51
Mant J, Hicks NJB (1995) Detecting differences in quality of care: the sensitivity of measures of process and outcome in treating acute myocardial infarction 311(7008):793–796
Micha R, Peñalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian DJJ (2017) Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA 317(9):912–924
Dietary Guidelines Advisory Committee. Dietary guidelines for Americans 2015–2020: Government Printing Office; 2015.
Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D (2016) Dietary intake among US adults, 1999–2012. JAMA 315(23):2542–2553
Shan ZR, C.D.; Rogers, G.; Ruan, M.; Wang, D.D.; Hu, F.B.; Mozaffarian, D.; Zhang, F.F.; Bhupathiraju, S.N. Trends in dietary carbohydrate, protein, and fat intake and diet quality among US adults, 1999–2016. JAMA. 2019;322(12):1178–87.
Zeng L, Ruan M, Liu J, Wilde P, Naumova EN, Mozaffarian D, et al. (2019) Trends in processed meat, unprocessed red meat, poultry, and fish consumption in the United States, 1999–2016. J Acad Nut Dietetics. 119(7):1085–98.
Dammann K, Hauge D, Rosen R, Schroeder N, Marquart L. Consumption and consumer challenges of wholegrain foods. Fibre-Rich and Wholegrain Foods: Improving Quality: Elsevier Ltd; 2013. p. 120–49.
Lee Y, Mozaffarian D, Sy S, Huang Y, Liu J, Wilde PE, et al. Cost-effectiveness of financial incentives for improving diet and health through Medicare and Medicaid: A microsimulation study. 2019;16(3):e1002761.
Mozaffarian D, Liu J, Sy S, Huang Y, Rehm C, Lee Y et al (2018) Cost-effectiveness of financial incentives and disincentives for improving food purchases and health through the US Supplemental Nutrition Assistance Program (SNAP): A microsimulation study. PLoS Med 15(10):e1002661
Mozaffarian D, Afshin A, Benowitz NL, Bittner V, Daniels SR, Franch HA et al (2012) Population approaches to improve diet, physical activity, and smoking habits: a scientific statement from the American Heart Association. Circulation 126(12):1514–1563
Mozaffarian D, Angell SY, Lang T, Rivera JAJB (2018) Role of government policy in nutrition—barriers to and opportunities for healthier eating. BMJ 361:2426
Hiza HA, Casavale KO, Guenther PM (2013) Davis CAJJotAoN, Dietetics. Diet quality of Americans differs by age, sex, race/ethnicity, income, and education level 113(2):297–306
Matsuda T, Saika KJJ (2013) The 5-year relative survival rate of stomach cancer in the USA, Europe and Japan. Japanese J Clin Oncol 43(11):1157–1158
DeSantis C, Siegel R, Bandi P, Jemal AJC (2011) Breast cancer statistics, 2014. CA A Cancer J Clin 61(6):408–418
Siegel R, DeSantis C, Jemal AJC (2014) Colorectal cancer statistics, 2014. CA A Cancer J Clin. 64(2):104–117
Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. 2009;6(4):e1000058.
Weir HK, Thompson TD, Soman A, Møller B, Leadbetter S, White MCJP (2020) Peer reviewed: meeting the healthy people 2020 objectives to Reduce Cancer Mortality. Prev Chronic Dis. https://doi.org/10.5888/pcd12.140482
Guy Jr GP, Thomas CC, Thompson T, Watson M, Massetti GM, Richardson LCJMM, et al. Vital signs: melanoma incidence and mortality trends and projections—United States, 1982–2030. 2015;64(21):591.
Acknowledgments
We acknowledge Dr. Angela Mariotto from the Division of Cancer Control and Population Sciences, National Cancer Institute for providing valuable data inputs related to direct medical costs of cancer care. We acknowledge Dr. Trevor Thompson from the Division of Cancer Prevention and Control, Centers for Disease Control and Prevention for modeling guidance. These individuals received no compensation for this work.
Funding
Drs. Zhang, Mozaffarian, Cudhea, Ruan, and Shan were supported by NIH/R01MD011501.
Author information
Authors and Affiliations
Contributions
Jaya Shankar Khushalani (J.S.K), Fang Fang Zhang (F.Z), and Donatus Ekwueme (D.E) designed research; J.S.K and Frederick Cudhea (F.C.) conducted research; J.S.K, F.C, Zhilei Shan (Z.S), and Mengyuan Ruan (M.R) analyzed data. J.S.K wrote the first draft and all authors commented on the previous versions of the manuscript. J.S.K had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Mozaffarian reports honoraria or consulting from AstraZeneca, Acasti Pharma, GOED, Haas Avocado Board, Nutrition Impact, Pollock Communications, Boston Heart Diagnostics, and Bunge; scientific advisory board, Omada Health and Elysium Health; chapter royalties from UpToDate, and research funding from National Institutes for Health and Gates Foundation. All other authors have no financial disclosures. The authors have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Khushalani, J.S., Cudhea, F.P., Ekwueme, D.U. et al. Estimated economic burden of cancer associated with suboptimal diet in the United States. Cancer Causes Control 33, 73–80 (2022). https://doi.org/10.1007/s10552-021-01503-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-021-01503-4