Abstract
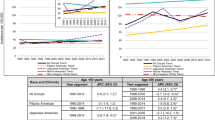
Breast cancer encompasses several distinct clinical entities of very different characteristics and behaviors, a fact which likely contributes to the higher breast cancer mortality in African-Americans (AA) despite the higher incidence in European-Americans (EA). We are interested in how incidence variability in cancer subtypes defined by combined estrogen receptor (ER) and grade contributes to racial mortality disparities. As an initial step, we compared age-specific and age-adjusted incidence rates for each ER/Grade subtype in South Carolina (SC—a southern state) with Ohio (a northern mid-western state), using state registry data for 1996–2004. Each ER/Grade subtype had a distinct incidence pattern and rate, with three striking racial/geographic differences. First, the racial incidence disparity in ER negative (ER−) cancers was mostly within the ER−/G3 subtype, of which AAs had ~65% higher incidence than did EAs; ER−/G2 was much less common, but of significantly higher incidence in AAs. Second, the racial disparity in ER positive (ER+) cancers was in the ER+/lower-grade cancers, with a marked EA excess in both states. Third, AA incidence of the ER+/lower-grade subtypes was ~26% higher in Ohio than in SC. The other subtypes (ER−/G1 and ER+/G3) varied minimally by race and state, and the latter showed a strong association with age. Age adjustment halved the racial difference in mean age at diagnosis to about 2 years younger in AAs, compared to 4 years younger in case comparisons. Use of age-adjusted and age-specific rates of breast cancer subtypes may improve understanding of racial incidence and mortality disparities over time and geography. This approach also may aid in estimating the race-specific incidence rates of triple-negative breast cancer.



Similar content being viewed by others
Abbreviations
- AA:
-
African-American
- ACoS:
-
American College of Surgeons
- CDC:
-
Centers for Disease Control and Prevention
- dk:
-
Not known or unavailable
- EA:
-
European-American
- ER:
-
Estrogen receptor
- ER+:
-
Positive ER expression status
- ER+/G1:
-
ER positive and Grade 1
- ER+/G1, 2:
-
ER positive and either Grade 1 or Grade 2
- ER−:
-
Negative ER expression status
- HER-2/neu:
-
Human epidermal growth factor receptor-2 also called HER-2
- NAACCR:
-
North American Association of Central Cancer Registries
- NPCR:
-
National Program of Cancer Registries
- PR:
-
Progesterone receptor
- SC:
-
South Carolina
- SCCCR:
-
South Carolina Central Cancer Registry
- SEER:
-
Surveillance, Epidemiology and End Results (program of the NCI)
- T-stage:
-
Tumor stage, based upon size of invasive primary tumor
- vs:
-
Versus
References
Henson DE, Chu K, Levine PH (2003) Histologic grade, stage, and survival in breast carcinoma. Comparison of African American and Caucasian women. Cancer 98:908–917
Curtis E, Quale C, Haggstrom D, Smith-Bindman R (2008) Racial and ethnic differences in breast cancer survival: how much is explained by screening, tumor severity, biology, treatment, comorbidities, and demographics? Cancer 112:171–180
American Cancer Society (2007) Breast cancer facts & figures 2007–2008. American Cancer Society, Inc, Atlanta p. 3
Fitzgibbons PL, Page DL, Weaver D, Thor AD, Allred DC, Clark GM, Ruby SG et al (2000) Prognostic factors in breast cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 124:966–978
Greene F, Page DL, Fleming ID, Fritz A, Balch DM, Haller DG, Morrow M (eds) (2002) AJCC cancer staging manual. Springer-Verlag, New York
Volpi A, Bacci F, Paradiso A, Saragoni L, Scarpi E, Ricci M et al (2004) Prognostic relevance of histologic grade and its components in node-negative breast cancer patients. Mod Pathol 17:1038–1044
Pinder SE, Murray S, Ellis IO, Trihia H, Elston CW, Gelber RD et al (1998) The importance of the histologic grade of invasive breast carcinoma and response to chemotherapy. Cancer 83:1529–1539
Page DL, Gray R, Allred DC, Dressler LG, Hatfield AK, Martino S et al (2001) Prediction of node-negative breast cancer outcome by histologic grading and S-phase analysis by flow cytometry: an Eastern Cooperative Oncology Group Study. Am J Clin Oncol 24:10–18
Sohib LH, Wittekind C (2002) TNM classification of malignant tumours: International Union Against Cancer
Cunningham JE, Butler WM (2004) Racial disparities in female breast cancer in South Carolina: clinical evidence for a biological basis even in small tumors. Breast Cancer Res Treat 88:161–176
Carey LA, Perou C, Livasy CA, Dressler LG, Cowan D, Conway K et al (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295:2492–2502
Bauer KR, Brown M, Cress RD et al (2007) Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population based study from the California cancer Registry. Cancer 109:1721–1728
United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS) (2008) Bridged-race population estimates, United States July 1st resident population by state, county, age, sex, bridged-race, and Hispanic origin, on CDC WONDER On-line Database. Vintage 2006: years 2000–2006, September 2007 online database, based on the August 16, 2007 data release. http://wonder.cdc.gov/bridged-race-v2006.html
National Center for Health Statistics (NCHS) (2008) http://www.cdc.gov/nchs/about/major/dvs/popbridge/popbridge.htm
National Cancer Institute Surveillance Research Program (2008) http://seer.cancer.gov/stdpopulations
North American Association of Central Cancer Registries (2008) http://www.cancer-rates.info/naaccr/
Jensen OM, Parkin DM, MacLennan R, Muir CS, Skeet RG (eds) (1991) Cancer registration: principles and methods. Scientific Publication No. 95. International Agency for Research on Cancer. Lyon, France, p 138 (Equations 11.11 and 11.12)
Sørlie T, Perou C, Tibshirani R, Aas T, Geisler S, Johnsen H et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98:10869–10874
Sørlie T, Wang Y, Xiao C, Johnsen H, Naume B, Samaha RR, Børresen-Dale AL (2006) Distinct molecular mechanisms underlying clinically relevant subtypes of breast cancer: gene expression analyses across three different platforms. BMC Genomics 7:127
Reis-Filho JS, Tutt A (2008) Triple negative tumours: a critical review. Histopathology 52:108–118
Rakha EA, Ellis IO (2009) Triple-negative/basal-like breast cancer: review. Pathology 41(1):40–47
Asselin-Labat ML, Shackleton M, Stingl J, Vaillant F, Forrest NC, Eaves CJ et al (2006) Steroid hormone receptor status of mouse mammary stem cells. J Natl Cancer Inst 98:1011–1014
Sims AH, Howell A, Howell SJ, Clarke RB (2007) Origins of breast cancer subtypes and therapeutic implications. Nat Clin Pract Oncol 4:516–525
Melchor L, Benitz J (2008) An integrative hypothesis about the origin and development of sporadic and familial breast cancer subtypes. Carcinogenesis 29(8):1475–1482
Bloushtain-Qimron N, Yao J, Shipitsin M, Maruyama R, Polyak K (2009) Epigenetic patterns of embryonic and adult stem cells. Cell Cycle 8(6):806–817
Abdel-Fatah TMA, Powell D, Hodi Z, Reis-Filho JS, Lee AHS, Ellis IO (2008) Morphologic and molecular evolutionary pathways of low nuclear grade invasive breast cancers and their putative precursor lesions: further evidence to support the concept of low nuclear grade breast neoplasia family. Am J Surg Pathol 32(4):513–523
Tlsty TD, Coussens LM (2006) Tumor stroma and regulation of cancer development. Ann Rev Pathol 1:119–150
Hunter KW, Crawford NP (2006) Germline polymorphism in metastatic progression. Cancer Res 66:1251–1254
Crawford NPS, Hunter K (2006) New perspectives on hereditary influences in metastatic progression. Trends Genet 22:555–561
Potter J, Cerhan JR, Sellers TA, McGovern PG, Drinkard C, Kushi LR, Folsom AR (1995) Progesterone and estrogen receptors and mammary neoplasia in the Iowa Women’s Health Study: how many types of breast cancer are there? Cancer Epidemiol Biomark Prev 4:319–326
Li CI, Malone K, Porter PL, Weiss NS, Tang M-TC, Daling JR (2003) The relationship between alcohol use and risk of breast cancer by histology and hormone receptor status among women 65–79 years of age. Cancer Epidemiol Biomark Prev 12:1061–1066
Smigal C, Jemal A, Ward E, Cokkinides V, Smith R, Howe HL, Thun M (2006) Trends in breast cancer by race and ethnicity: update 2006. CA Cancer J Clin 56:168–183
Chen WY, Colditz G (2007) Risk factors and hormone-receptor status: epidemiology, risk-prediction models and treatment implications for breast cancer. Nat Clin Pract Oncol 4:415–423
Yang XR, Sherman ME, Rimm DL, Lissowska J, Brinton LA, Peplonska B, Hewitt SM, Anderson WF, Szeszenia-Dabrowska N, Bardin-Mikolajczak A, Zatonski W, Cartun R, Mandich D, Rymkiewicz G, Ligaj M, Lukaszek S, Kordek R, Garcia-Closas M (2007) Differences in risk factors for breast cancer molecular subtypes in a population-based study. Cancer Epidemiol Biomarkers Prev 16(3):439–443
Setiawan VW, Monroe KR, Wilkens LR, Kolonel LN, Pike MC, Henderson BE (2009) Breast cancer risk factors defined by estrogen and progesterone receptor status: the multiethnic cohort study. AJE Adv Access
Stead L, Lash TL, Sobieraj J, Chi D, Westrup J, Charlot M, Blanchard R, Lee JC, King T, Rosenberg CL (2009) Triple negative breast cancers are increased in black women regardless of age or body mass index. Breast Cancer Res 11(2):R18 [Epub ahead of print.]
Karp SE, Tonin PN, Begin LR, Martinez JJ, Zhang JC, Pollak MN, Foulkes WD (1997) Influence of BRCA1 mutations on nuclear grade and estrogen receptor status of breast carcinoma in Ashkenazi Jewish women. Cancer 80:435–441
Anderson WF, Chen B, Brinton LA, Devesa SS (2007) Qualitative age interactions (or effect modification) suggest different cancer pathways for early-onset and late-onset breast cancers. Cancer Causes Control 18:1187–1198
Anderson WF, Matsuno R (2006) Breast cancer heterogeneity: a mixture of at least two main types? J Natl Cancer Inst 98:948–951
Krieger N, Chen JT, Ware JH, Kaddour A (2008) Race/ethnicity and breast cancer estrogen receptor status: impact of class, missing data and modeling assumptions. Cancer Causes Control doi: 10.1007/s10552-008-9202-1
Robert SA, Strombom I, Trentham-Dietz A et al (2004) Socioeconomic risk factors for breast cancer: distinguishing individual- and community-level effects. Epidemiology 15:442–450
Acknowledgments
We thank the following people from the South Carolina Central Cancer Registry for providing the South Carolina data: Susan Bollick-Aldrich, MSPH, CTR (director), Catishia Moseley, MSPH, and Deborah Hurley, MSPH. Special thanks are also due to Mike Byrd, PhD, MPH, LMSW, director of the Chronic Diseases Branch of the South Carolina Department of Health and Environmental Control, for his unflagging encouragement of this analysis, and to Dr. Anthony Alberg of the Medical University of South Carolina for his editorial assistance. Ohio cancer incidence data were obtained from the Ohio Cancer Incidence Surveillance System (OCISS), Ohio Department of Health (ODH), a registry participating in the National Program of Cancer Registries of the Centers for Disease Control and Prevention (CDC). Use of these data does not imply ODH or CDC either agrees or disagrees with any presentations, analyses, interpretations, or conclusions. Information about the OCISS can be obtained at: http://www.odh.ohio.gov/odhPrograms/svio/ci_surv/ci_surv1.aspx.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was performed at Division of Biostatistics and Epidemiology, Department of Medicine, Medical University of South Carolina, Charleston SC, AND at the University of South Carolina, Columbia, SC.
Rights and permissions
About this article
Cite this article
Cunningham, J.E., Montero, A.J., Garrett-Mayer, E. et al. Racial differences in the incidence of breast cancer subtypes defined by combined histologic grade and hormone receptor status. Cancer Causes Control 21, 399–409 (2010). https://doi.org/10.1007/s10552-009-9472-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-009-9472-2