Abstract
Purpose
All vascular access strategies foradministering chemotherapy in early stage breast cancer (EBC) are associated with risks and benefits. As the most effective type of access is unknown a feasibility trial, prior to conducting a large pragmatic trial, was undertaken.
Methods
The trial methodology utilized broad eligibility criteria and the integrated consent model incorporating oral consent. EBC patients receiving non-trastuzumab-containing chemotherapy were randomized to peripheral access or central line insertion. The a priori definition of feasibility was: > 25% of patients approached agreed to randomisation and > 25% of physicians approached patients. Secondary outcomes included rates of line-associated complications.
Results
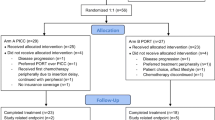
Of 159 patients approached, 150 (94.3%) agreed to randomisation, 77 (51.3%) were randomized to peripheral and 73 (48.7%) to central access. 6/26 (23.1%) of medical oncologists approached patients. Rates of complications per chemotherapy cycles in the peripheral vs central access groups with risk difference (RD) (95% CI) were: thrombotic events requiring anticoagulation [1 (0.3%) vs. 3 (1.0%), RD − 0.7(− 1.9,0.5)], line infections [0 (0%) vs. 1 (0.3%), RD − 0.3(− 0.9,0.3)], phlebitis [2 (0.6%) vs. 0 (0%), RD 0.3(− 0.3,0.8)], and tissue infiltrations [4 (1.1%) vs. 1 (0.3%), RD 0.8(− 0.4,2.1)]. Overall, 8.0% (6/75) and 7.7% (5/65) of patients had at least one of these complications in the peripheral and central access arms respectively [RD − 0.9(− 9.4,7.6)]. The study was terminated early due to slow accrual.
Conclusion
While meeting its a priori feasibility criteria for patient engagement, the slow accrual means that conducting a large pragmatic trial would require overcoming the barriers to physician recruitment.
TRIAL REGISTRATION: NCT02688998

Similar content being viewed by others
References
Lipitz-Snyderman A et al (2015) Complications associated with use of long-term central venous catheters among commercially insured women with breast cancer. J Oncol Pract 11(6):505–510
Chopra V et al (2013) Risk of venous thromboembolism associated with peripherally inserted central catheters: a systematic review and meta-analysis. Lancet 382(9889):311–325
LeVasseur N et al (2018) Optimizing vascular access for patients receiving intravenous systemic therapy for early-stage breast cancer-a survey of oncology nurses and physicians. Curr Oncol 25(4):e298–e304
LeVasseur N et al (2018) Perceptions of vascular access for intravenous systemic therapy and risk factors for lymphedema in early-stage breast cancer—a patient survey. Curr Oncol 25(4):e305–e310
Krein SL et al (2019) Patient-reported complications related to peripherally inserted central catheters: a multicentre prospective cohort study. BMJ Qual Saf 28(7):574
Hilton J et al (2016) Novel methodology for comparing standard-of-care interventions in patients with cancer. J Oncol Pract 12:e1016–e1024
ClinicalTrials.gov. REaCT-vascular access Her2 negative vascular access strategies for (Neo) adjuvant breast cancer treatment without trastuzumab (OTT 15-07). 2017 [cited 2017 April 18]; https://clinicaltrials.gov/ct2/show/NCT02688998
Robinson A et al (2018) Optimal vascular access strategies for patients receiving chemotherapy for early-stage breast cancer: a systematic review. Breast Cancer Res Treat 171:1–14
Kim SY, Miller FG (2014) Informed consent for pragmatic trials–the integrated consent model. N Engl J Med 370(8):769–772
Sugarman J, Califf RM (2014) Ethics and regulatory complexities for pragmatic clinical trials. JAMA 311(23):2381–2382
Doellman D et al (2009) Infiltration and extravasation: update on prevention and management. J Infus Nurs 32(4):203–211
Singh KR et al (2014) Morbidity of chemotherapy administration and satisfaction in breast cancer patients: a comparative study of totally implantable venous access device (TIVAD) versus peripheral venous access usage. World J Surg 38(5):1084–1092
Di Carlo I et al (2001) Totally implantable venous access devices implanted surgically: a retrospective study on early and late complications. Arch Surg 136(9):1050–1053
Ozyuvaci E, Kutlu F (2006) Totally implantable venous access devices via subclavian vein: a retrospective study of 368 oncology patients. Adv Ther 23(4):574–581
Piran S et al (2014) Incidence and risk factors of symptomatic venous thromboembolism related to implanted ports in cancer patients. Thromb Res 133(1):30–33
Vescia S et al (2008) Management of venous port systems in oncology: a review of current evidence. Ann Oncol 19(1):9–15
Aw A et al (2012) Incidence and predictive factors of symptomatic thrombosis related to peripherally inserted central catheters in chemotherapy patients. Thromb Res 130(3):323–326
Showalter SL et al (2013) Lifestyle risk factors associated with arm swelling among women with breast cancer. Ann Surg Oncol 20(3):842–849
Acknowledgements
We are grateful for patients and their families for their assistance with this study. Accrual by physician was: Clemons (142), Robinson (3), Mates (2), Parulekar (2) and Joy (1). We are grateful to Sheryl McDiarmid RN, Drs Chris Booth, Nathalie Levasseur and Matthew McInnes for their insight into protocol development.
Funding
This study was funded through the Rethinking Clinical Trials (REaCT) program.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Dr. Awan reports participating in the Novartis Canada Advisory Board on the use of Ribociclib. Dr. Hutton reports personal fees from Cornerstone Research, outside the submitted work. The remaining authors declare that they have no conflicts of interest (Robinson, Stober, Fergusson, Kehoe, Bedard, MacDonald, Brunet, Saunders, Mazzarello, Vandermeer, Joy, Basulaiman, Mallick, and Clemons).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Robinson, A., Stober, C., Fergusson, D. et al. A multicentre, randomized pilot trial comparing vascular access strategies for early stage breast cancer patients receiving non-trastuzumab containing chemotherapy. Breast Cancer Res Treat 178, 337–345 (2019). https://doi.org/10.1007/s10549-019-05388-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-019-05388-5