Abstract
Background
Obesity may negatively affect survival in breast cancer (BC), but studies are conflicting, and associations may vary by tumor subtypes and race/ethnicity groups.
Methods
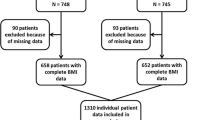
In a retrospective review, we identified 273 women with invasive BC administered Adriamycin/Taxane-based neoadjuvant chemotherapy from 2004 to 2016 with body mass index (BMI) data at diagnosis. Obesity was defined as BMI ≥30. Associations between obesity and event-free survival (EFS), using STEEP events, and overall survival (OS), using all-cause mortality, were assessed overall and stratified by tumor subtype [[Hormone Receptor Positive (HR+)/HER2−, HER2+, and Triple-Negative Breast Cancer (TNBC])] in our diverse population.
Results
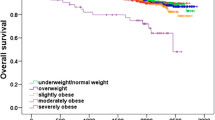
Median follow-up was 32.6 months (range 5.7–137.8 months). Overall, obesity was associated with worse EFS (HR 1.71, 95% CI 1.03–2.84, p = 0.04) and a trend towards worse OS (p = 0.13). In HR+/HER2− disease (n = 135), there was an interaction between obesity and hormonal therapy with respect to OS but not EFS. In those receiving tamoxifen (n = 33), obesity was associated with worse OS (HR 9.27, 95% CI 0.96–89.3, p = 0.05). In those receiving an aromatase inhibitor (n = 89), there was no association between obesity and OS. In TNBC (n = 44), obesity was associated with worse EFS (HR 2.62, 95% CI 1.03–6.66, p = 0.04) and a trend towards worse OS (p = 0.06). In HER2+ disease (n = 94), obesity was associated with a trend towards worse EFS (HR 3.37, 95% CI 0.97–11.72, p = 0.06) but not OS. Race/ethnicity was not associated with survival in any subtype, and there were no interactions with obesity on survival.
Conclusions
Obesity may negatively impact survival, with differences among tumor subtypes.



Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- NAC:
-
Neoadjuvant chemotherapy
- HR+:
-
Hormone receptor positive
- TNBC:
-
Triple-negative breast cancer
- pCR:
-
Pathologic complete response
- EFS:
-
Event-free survival
- OS:
-
Overall survival
References
Bhaskaran K, Douglas I, Forbes H, dos-Santos-Silva I, Leon DA, Smeeth L (2014) Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet 384(9945):755–765
Tsai AG, Williamson DF, Glick HA (2011) Direct medical cost of overweight and obesity in the USA: a quantitative systematic review. Obesity Rev 12(1):50–61
Gathirua-Mwangi WG, Zollinger TW, Murage MJ, Pradhan KR, Champion VL (2015) Adult BMI change and risk of breast cancer: National Health and Nutrition Examination Survey (NHANES) 2005–2010. Breast Cancer 22(6):648–656
Jiralerspong S, Goodwin PJ (2016) Obesity and breast cancer prognosis: evidence, challenges, and opportunities. J Clin Oncol 34(35):4203–4216
Chan DS, Vieira AR, Aune D et al (2014) Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol 25(10):1901–1914
Niraula S, Ocana A, Ennis M, Goodwin PJ (2012) Body size and breast cancer prognosis in relation to hormone receptor and menopausal status: a meta-analysis. Breast Cancer Res Treat 134(2):769–781
Protani M, Coory M, Martin JH (2010) Effect of obesity on survival of women with breast cancer: systematic review and meta-analysis. Breast Cancer Res Treat 123(3):627–635
Allott EH, Hursting SD (2015) Obesity and cancer: mechanistic insights from transdisciplinary studies. Endocr Relat Cancer 22(6):R365–R386
Pfeiler G, Konigsberg R, Fesl C et al (2011) Impact of body mass index on the efficacy of endocrine therapy in premenopausal patients with breast cancer: an analysis of the prospective ABCSG-12 trial. J Clin Oncol 29(19):2653–2659
Sestak I, Distler W, Forbes JF, Dowsett M, Howell A, Cuzick J (2010) Effect of body mass index on recurrences in tamoxifen and anastrozole treated women: an exploratory analysis from the ATAC trial. J Clin Oncol 28(21):3411–3415
Dignam JJ, Wieand K, Johnson KA, Fisher B, Xu L, Mamounas EP (2003) Obesity, tamoxifen use, and outcomes in women with estrogen receptor-positive early-stage breast cancer. J Natl Cancer Inst 95(19):1467–1476
Sparano JA, Wang M, Zhao F et al (2012) Obesity at diagnosis is associated with inferior outcomes in hormone receptor-positive operable breast cancer. Cancer 118(23):5937–5946
Crozier JA, Moreno-Aspitia A, Ballman KV, Dueck AC, Pockaj BA, Perez EA (2013) Effect of body mass index on tumor characteristics and disease-free survival in patients from the HER2-positive adjuvant trastuzumab trial N9831. Cancer 119(13):2447–2454
Hao S, Liu Y, Yu KD, Chen S, Yang WT, Shao ZM (2015) Overweight as a prognostic factor for triple-negative breast cancers in chinese women. PLoS ONE 10(6):e0129741
Mazzarella L, Disalvatore D, Bagnardi V et al (2013) Obesity increases the incidence of distant metastases in oestrogen receptor-negative human epidermal growth factor receptor 2-positive breast cancer patients. Eur J Cancer 49(17):3588–3597
Widschwendter P, Friedl TW, Schwentner L et al (2015) The influence of obesity on survival in early, high-risk breast cancer: results from the randomized SUCCESS A trial. Breast Cancer Res 17:129
Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 307(5):491–497
Bandera EV, Maskarinec G, Romieu I, John EM (2015) Racial and ethnic disparities in the impact of obesity on breast cancer risk and survival: a global perspective. Adv. Nutr. 6(6):803–819
Hunt BR, Hurlbert MS (2016) Black:white disparities in breast cancer mortality in the 50 largest cities in the United States, 2005–2014. Cancer epidemiology. 45:169–173
Tichy JR, Deal AM, Anders CK, Reeder-Hayes K, Carey LA (2015) Race, response to chemotherapy, and outcome within clinical breast cancer subtypes. Breast Cancer Res Treat 150(3):667–674
Warner ET, Ballman KV, Strand C et al (2016) Impact of race, ethnicity, and BMI on achievement of pathologic complete response following neoadjuvant chemotherapy for breast cancer: a pooled analysis of four prospective Alliance clinical trials (A151426). Breast Cancer Res Treat 159(1):109–118
Hall IJ, Newman B, Millikan RC, Moorman PG (2000) Body size and breast cancer risk in black women and white women: the Carolina Breast Cancer Study. Am J Epidemiol 151(8):754–764
Karatas F, Erdem GU, Sahin S et al (2016) Obesity is an independent prognostic factor of decreased pathological complete response to neoadjuvant chemotherapy in breast cancer patients. Breast 32:237–244
Fontanella C, Lederer B, Gade S et al (2015) Impact of body mass index on neoadjuvant treatment outcome: a pooled analysis of eight prospective neoadjuvant breast cancer trials. Breast Cancer Res Treat 150(1):127–139
Erbes T, Stickeler E, Rucker G et al (2016) BMI and pathologic complete response to neoadjuvant chemotherapy in breast cancer: a study and meta-analysis. Clin Breast Cancer 16(4):e119–e132
WHO (1995) Physical status: the use and interpretation of anthropometry. WHO, Geneva
Du Bois D, Du Bois EF (1989) A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition 5(5):303–311 discussion 312–303
Hammond ME, Hayes DF, Wolff AC, Mangu PB, Temin S (2010) American society of clinical oncology/college of american pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Oncol Pract/Am Soc Clin Oncol 6(4):195–197
Tchrakian N, Flanagan L, Harford J, Gannon JM, Quinn CM (2015) New ASCO/CAP guideline recommendations for HER2 testing increase the proportion of reflex in situ hybridization tests and of HER2 positive breast cancers. Virchows Archiv 468:207–211
Zhang C, Wang S, Israel HP et al (2015) Higher locoregional recurrence rate for triple-negative breast cancer following neoadjuvant chemotherapy, surgery and radiotherapy. SpringerPlus 4:386
Hudis CA, Barlow WE, Costantino JP et al (2007) Proposal for standardized definitions for efficacy end points in adjuvant breast cancer trials: the STEEP system. J Clin Oncol 25(15):2127–2132
Luen SJ, Salgado R, Fox S et al (2017) Tumour-infiltrating lymphocytes in advanced HER2-positive breast cancer treated with pertuzumab or placebo in addition to trastuzumab and docetaxel: a retrospective analysis of the CLEOPATRA study. Lancet Oncol 18(1):52–62
Verma S, Miles D, Gianni L et al (2012) Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med 367(19):1783–1791
Matthews SB, Thompson HJ (2016) The obesity-breast cancer conundrum: an analysis of the issues. Int J Mol Sci 17(6):989
Renehan AG, Zwahlen M, Egger M (2015) Adiposity and cancer risk: new mechanistic insights from epidemiology. Nat Rev Cancer 15(8):484–498
Ford NA, Lashinger LM, Allott EH, Hursting SD (2013) Mechanistic targets and phytochemical strategies for breaking the obesity-cancer link. Front Oncol 3:209
Lashinger LM, Ford NA, Hursting SD (2014) Interacting inflammatory and growth factor signals underlie the obesity-cancer link. J Nutr 144(2):109–113
Hair BY, Troester MA, Edmiston SN et al (2015) Body mass index is associated with gene methylation in estrogen receptor-positive breast tumors. Cancer Epidemiol Biomark Prevent 24(3):580–586
Rossi EL, de Angel RE, Bowers LW et al (2016) Obesity-associated alterations in inflammation, epigenetics, and mammary tumor growth persist in formerly obese mice. Cancer Prevent Res 9(5):339–348
Goodwin PJ (2013) Obesity and endocrine therapy: host factors and breast cancer outcome. Breast 22(Suppl2):S44–S47
Ewertz M, Gray KP, Regan MM et al (2012) Obesity and risk of recurrence or death after adjuvant endocrine therapy with letrozole or tamoxifen in the breast international group 1-98 trial. J Clin Oncol 30(32):3967–3975
Subbaramaiah K, Howe LR, Bhardwaj P et al (2011) Obesity is associated with inflammation and elevated aromatase expression in the mouse mammary gland. Cancer Prevent Res 4(3):329–346
Hubalek M, Oberguggenberger A, Beer B et al (2014) Does obesity interfere with anastrozole treatment? Positive association between body mass index and anastrozole plasma levels. Clin Breast Cancer 14(4):291–296
Diorio C, Lemieux J, Provencher L, Hogue JC, Vachon E (2012) Aromatase inhibitors in obese breast cancer patients are not associated with increased plasma estradiol levels. Breast Cancer Res Treat 136(2):573–579
Sini V, Lunardi G, Cirillo M et al (2014) Body mass index and circulating oestrone sulphate in women treated with adjuvant letrozole. Br J Cancer 110(5):1133–1138
Phipps AI, Ichikawa L, Bowles EJA et al (2010) Defining menopausal status in epidemiologic studies: a comparison of multiple approaches and their effects on breast cancer rates. Maturitas 67(1):60–66
George SM, Bernstein L, Smith AW et al (2014) Central adiposity after breast cancer diagnosis is related to mortality in the health, eating, activity, and lifestyle study. Breast Cancer Res Treat 146(3):647–655
Sun X, Nichols HB, Robinson W, Sherman ME, Olshan AF, Troester MA (2015) Post-diagnosis adiposity and survival among breast cancer patients: influence of breast cancer subtype. Cancer Causes Control 26(12):1803–1811
Liu YL, Saraf A, Catanese B et al (2017) Obesity and survival in the neoadjuvant breast cancer setting: role of tumor subtype in an ethnically diverse population. Breast Cancer Res Treat. doi:10.1007/s10549-017-4507-y
Funding
This study was funded by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number KL2 TR000081.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author EC has received funding from Merck and has served as a consultant for Eisai. Author KK has served as a consultant for Lilly, Biotheranostics, Amgen, Eisai, and Novartis. All other authors have no conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, Y.L., Saraf, A., Catanese, B. et al. Obesity and survival in the neoadjuvant breast cancer setting: role of tumor subtype in an ethnically diverse population. Breast Cancer Res Treat 167, 277–288 (2018). https://doi.org/10.1007/s10549-017-4507-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-017-4507-y