Abstract
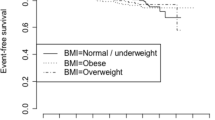
Obesity is associated with an increased risk of breast cancer (BC) and poorer outcome. We assessed the impact of body mass index (BMI) on pathological complete response (pCR), disease-free (DFS), and overall survival (OS), according to BC subtypes in patients with primary BC treated with neoadjuvant chemotherapy. 8,872 patients with primary BC from eight neoadjuvant trials were categorized according to BMI: underweight (<18.5 kg/m2), normal weight (18.5 to <25 kg/m2), overweight (25 to <30 kg/m2), obese (30 to <40 kg/m2), and very obese (≥40 kg/m2). BC subtypes were defined as luminal-like (ER/PgR-positive and HER2-negative), HER2/luminal (ER/PgR-positive and HER2-positive), HER2-like (ER/PgR-negative and HER2-positive), and triple-negative (TNBC; ER/PgR- and HER2-negative). pCR rate was higher in normal weight patients compared with all other BMI groups (P = 0.003). Mean DFS and OS were shorter in obese (87.3 months, P = 0.014 and 94.9 months, P = 0.001, respectively) and very obese (66.6 months, P < 0.001 and 75.3 months, P < 0.001, respectively) compared with normal weight patients (91.5 and 98.8 months, respectively) which was confirmed by subpopulation treatment effect pattern plot analyses and was consistent in luminal-like and TNBC. No interaction was observed between BMI and pCR. Normal weight patients experienced less non-hematological adverse events (P = 0.002) and were more likely to receive full taxane doses (P < 0.001) compared with all other BMI groups. In multivariable analysis, the dose of taxanes was predictive for pCR (P < 0.001). Higher BMI was associated with lower pCR and a detrimental impact on survival. Normal weight patients had the best compliance to chemotherapy and received the highest taxane doses, which seems to be related with treatment outcomes.


Similar content being viewed by others
References
Flegal KM, Carroll MD, Kit BK, Ogden CL (2012) Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA 307:491–497
Mokdad AH, Ford ES, Bowman BA et al (2003) Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA 289:76–79
Hossain P, Kawar B, El Nahas M (2007) Obesity and diabetes in the developing world–a growing challenge. N Engl J Med 356:213–215
Flegal KM, Kit BK, Orpana H, Graubard BI (2013) Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 309:71–82
Pfeiffer RM, Park Y, Kreimer AR et al (2013) Risk prediction for breast, endometrial, and ovarian cancer in white women aged 50 y or older: derivation and validation from population-based cohort studies. PLoS Med 10:e1001492
Harvey AE, Lashinger LM, Hursting SD (2011) The growing challenge of obesity and cancer: an inflammatory issue. Ann NY Acad Sci 1229:45–52
Hursting SD, Dunlap SM (2012) Obesity, metabolic dysregulation, and cancer: a growing concern and an inflammatory (and microenvironmental) issue. Ann NY Acad Sci 1271:82–87
Shoelson SE, Lee J, Goldfine AB (2006) Inflammation and insulin resistance. J Clin Invest 116:1793–1801
Gnant M, Pfeiler G, Stöger H et al (2013) The predictive impact of body mass index on the efficacy of extended adjuvant endocrine treatment with anastrozole in postmenopausal patients with breast cancer: an analysis of the randomised ABCSG-6a trial. Br J Cancer 109:589–596
Litton JK, Gonzalez-Angulo AM, Warneke CL et al (2008) Relationship between obesity and pathologic response to neoadjuvant chemotherapy among women with operable breast cancer. J Clin Oncol 26:4072–4077
Del Fabbro E, Parsons H, Warneke CL et al (2012) The relationship between body composition and response to neoadjuvant chemotherapy in women with operable breast cancer. Oncologist 17:1240–1245
Chen S, Chen CM, Zhou Y et al (2012) Obesity or overweight is associated with worse pathological response to neoadjuvant chemotherapy among Chinese women with breast cancer. PLoS ONE 7:e41380
Berclaz G, Li S, Price KN et al (2004) Body mass index as a prognostic feature in operable breast cancer: the International Breast Cancer Study Group experience. Ann Oncol 15:875–884
Pajares B, Pollán M, Martín M et al (2013) Obesity and survival in operable breast cancer patients treated with adjuvant anthracyclines and taxanes according to pathological subtypes: a pooled analysis. Breast Cancer Res 15:R105
Tait S, Pacheco JM, Gao F et al (2014) Body mass index, diabetes, and triple-negative breast cancer prognosis. Breast Cancer Res Treat 146:189–197
Chan DS, Vieira AR, Aune D et al (2014) Body mass index and survival in women with breast cancer–systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol 25:1901–1914
Griggs JJ, Mangu PB, Anderson H et al (2012) Appropriate chemotherapy dosing for obese adult patients with cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 30:1553–1561
Peairs KS, Barone BB, Snyder CF et al (2011) Diabetes mellitus and breast cancer outcomes: a systematic review and meta-analysis. J Clin Oncol 29:40–46
Jiralerspong S, Palla SL, Giordano SH et al (2009) Metformin and pathologic complete responses to neoadjuvant chemotherapy in diabetic patients with breast cancer. J Clin Oncol 27:3297–3302
Jiralerspong S, Kim ES, Dong W et al (2013) Obesity, diabetes, and survival outcomes in a large cohort of early-stage breast cancer patients. Ann Oncol 24:2506–2514
von Minckwitz G, Fontanella C (2013) Selecting the neoadjuvant treatment by molecular subtype: how to maximize the benefit? Breast 22(Suppl 2):S149–S151
von Minckwitz G, Untch M, Blohmer JU et al (2012) Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol 30:1796–1804
von Minckwitz G, Blohmer JU, Costa SD et al (2013) Response-guided neoadjuvant chemotherapy for breast cancer. J Clin Oncol 31:3623–3630
von Minckwitz G, Raab G, Caputo A et al (2005) Doxorubicin with cyclophosphamide followed by docetaxel every 21 days compared with doxorubicin and docetaxel every 14 days as preoperative treatment in operable breast cancer: the GEPARDUO study of the German Breast Group. J Clin Oncol 23:2676–2685
von Minckwitz G, Blohmer JU, Raab G et al (2005) In vivo chemosensitivity-adapted preoperative chemotherapy in patients with early-stage breast cancer: the GEPARTRIO pilot study. Ann Oncol 16:56–63
von Minckwitz G, Kümmel S, Vogel P et al (2008) Intensified neoadjuvant chemotherapy in early-responding breast cancer: phase III randomized GeparTrio study. J Natl Cancer Inst 100:552–562
von Minckwitz G, Kümmel S, Vogel P et al (2008) Neoadjuvant vinorelbine-capecitabine versus docetaxel-doxorubicin-cyclophosphamide in early nonresponsive breast cancer: phase III randomized GeparTrio trial. J Natl Cancer Inst 100:542–551
Untch M, Rezai M, Loibl S et al (2010) Neoadjuvant treatment with trastuzumab in HER2-positive breast cancer: results from the GeparQuattro study. J Clin Oncol 28:2024–2031
von Minckwitz G, Darb-Esfahani S, Loibl S et al (2012) Responsiveness of adjacent ductal carcinoma in situ and changes in HER2 status after neoadjuvant chemotherapy/trastuzumab treatment in early breast cancer–results from the GeparQuattro study (GBG 40). Breast Cancer Res Treat 132:863–870
von Minckwitz G, Eidtmann H, Loibl S et al (2011) Integrating bevacizumab, everolimus, and lapatinib into current neoadjuvant chemotherapy regimen for primary breast cancer. Safety results of the GeparQuinto trial. Ann Oncol 22:301–306
Untch M, Loibl S, Bischoff J et al (2012) Lapatinib versus trastuzumab in combination with neoadjuvant anthracycline-taxane-based chemotherapy (GeparQuinto, GBG 44): a randomised phase 3 trial. Lancet Oncol 13:135–144
von Minckwitz G, Eidtmann H, Rezai M et al (2012) Neoadjuvant chemotherapy and bevacizumab for HER2-negative breast cancer. N Engl J Med 366:299–309
Huober J, Fasching PA, Hanusch C et al (2013) Neoadjuvant chemotherapy with paclitaxel and everolimus in breast cancer patients with non-responsive tumours to epirubicin/cyclophosphamide (EC) ± bevacizumab—results of the randomised GeparQuinto study (GBG 44). Eur J Cancer 49:2284–2293
Untch M, Möbus V, Kuhn W et al (2009) Intensive dose-dense compared with conventionally scheduled preoperative chemotherapy for high-risk primary breast cancer. J Clin Oncol 27:2938–2945
Untch M, Fasching PA, Konecny GE et al (2011) PREPARE trial: a randomized phase III trial comparing preoperative, dose-dense, dose-intensified chemotherapy with epirubicin, paclitaxel and CMF versus a standard-dosed epirubicin/cyclophosphamide followed by paclitaxel ± darbepoetin alfa in primary breast cancer–results at the time of surgery. Ann Oncol 22:1988–1998
Untch M, Fasching PA, Konecny GE et al (2011) Pathologic complete response after neoadjuvant chemotherapy plus trastuzumab predicts favorable survival in human epidermal growth factor receptor 2-overexpressing breast cancer: results from the TECHNO trial of the AGO and GBG study groups. J Clin Oncol 29:3351–3357
Goldhirsch A, Wood WC, Gelber RD et al (2007) 10th St. Gallen conference. Progress and promise: highlights of the international expert consensus on the primary therapy of early breast cancer 2007. Ann Oncol 18:1133–1144
World Health Organization (2014) BMI classification. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed 17 December 2014
Mosteller RD (1987) Simplified calculation of body-surface area. N Engl J Med 317:1098
Hudis CA, Barlow WE, Costantino JP et al (2007) Proposal for standardized definitions for efficacy end points in adjuvant breast cancer trials: the STEEP system. J Clin Oncol 25:2127–2132
Goldhirsch A, Glick JH, Gelber RD, Senn HJ (1998) International Consensus Panel on the treatment of primary breast cancer. V: update 1998. Recent results. Cancer Res 152:481–497
Bonetti M, Gelber RD (2000) A graphical method to assess treatment-covariate interactions using the Cox model on subsets of the data. Stat Med 19:2595–2609
Houssami N, Macaskill P, von Minckwitz G et al (2012) Meta-analysis of the association of breast cancer subtype and pathologic complete response to neoadjuvant chemotherapy. Eur J Cancer 48:3342–3354
Dent S, Oyan B, Honig A et al (2013) HER2-targeted therapy in breast cancer: a systematic review of neoadjuvant trials. Cancer Treat Rev 39:622–631
von Minckwitz G, Loibl S, Untch M (2012) What is the current standard of care for anti-HER2 neoadjuvant therapy in breast cancer? Oncology (Williston Park) 26:20–26
Sparano JA, Wang M, Zhao F et al (2012) Obesity at diagnosis is associated with inferior outcomes in hormone receptor-positive operable breast cancer. Cancer 118:5937–5946
Sestak I, Distler W, Forbes JF et al (2010) Effect of body mass index on recurrences in tamoxifen and anastrozole treated women: an exploratory analysis from the ATAC trial. J Clin Oncol 28:3411–3415
Pan H, Gray RG (on behalf of the Early Breast Cancer Trialists’ Collaborative Group) (2014) Effect of obesity in premenopausal ER+ early breast cancer: EBCTCG data on 80,000 patients in 70 trials. J Clin Oncol 32:5 (suppl; abstr 503)
Pfeiler G, Königsberg R, Fesl C et al (2011) Impact of body mass index on the efficacy of endocrine therapy in premenopausal patients with breast cancer: an analysis of the prospective ABCSG-12 trial. J Clin Oncol 29:2653–2659
Simpson ER, Brown KA (2013) Minireview: obesity and breast cancer: a tale of inflammation and dysregulated metabolism. Mol Endocrinol 27:715–725
Pfeiler G, Königsberg R, Hadji P et al (2013) Impact of body mass index on estradiol depletion by aromatase inhibitors in postmenopausal women with early breast cancer. Br J Cancer 109:1522–1527
Becker MA, Ibrahim YH, Cui X et al (2011) The IGF pathway regulates ERα through a S6K1-dependent mechanism in breast cancer cells. Mol Endocrinol 25:516–528
Tinoco G, Warsch S, Glück S et al (2013) Treating breast cancer in the 21st century: emerging biological therapies. J Cancer 4:117–132
Goodwin PJ, Ennis M, Pritchard KI et al (2002) Fasting insulin and outcome in early-stage breast cancer: results of a prospective cohort study. J Clin Oncol 20:42–51
Goodwin PJ, Ennis M, Bahl M et al (2009) High insulin levels in newly diagnosed breast cancer patients reflect underlying insulin resistance and are associated with components of the insulin resistance syndrome. Breast Cancer Res Treat 114:517–525
Goodwin PJ, Ennis M, Pritchard KI et al (2012) Insulin- and obesity-related variables in early-stage breast cancer: correlations and time course of prognostic associations. J Clin Oncol 30:164–171
Irwin ML, Duggan C, Wang CY et al (2011) Fasting C-peptide levels and death resulting from all causes and breast cancer: the health, eating, activity, and lifestyle study. J Clin Oncol 29:47–53
Griggs JJ, Culakova E, Sorbero ME et al (2007) Effect of patient socioeconomic status and body mass index on the quality of breast cancer adjuvant chemotherapy. J Clin Oncol 25:277–284
Griggs JJ, Sorbero ME, Lyman GH (2005) Undertreatment of obese women receiving breast cancer chemotherapy. Arch Intern Med 165:1267–1273
Ladoire S, Dalban C, Roché H et al (2014) Effect of obesity on disease-free and overall survival in node-positive breast cancer patients in a large French population: a pooled analysis of two randomised trials. Eur J Cancer 50:506–516
Qin YY, Li H, Guo XJ et al (2011) Adjuvant chemotherapy, with or without taxanes, in early or operable breast cancer: a meta-analysis of 19 randomized trials with 30698 patients. PLoS ONE 6:e26946
Cuppone F, Bria E, Carlini P et al (2008) Taxanes as primary chemotherapy for early breast cancer: meta-analysis of randomized trials. Cancer 113:238–246
Kramer CK, Zinman B, Retnakaran R (2013) Are metabolically healthy overweight and obesity benign conditions? A systematic review and meta-analysis. Ann Intern Med 159:758–769
Conflict of interest
Jens-Uwe Blohmer: Consultant/Advisory role by ROCHE. Claus Hanusch: Consultant/Advisory role by NOVARTIS, AMGEN. All other authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fontanella, C., Lederer, B., Gade, S. et al. Impact of body mass index on neoadjuvant treatment outcome: a pooled analysis of eight prospective neoadjuvant breast cancer trials. Breast Cancer Res Treat 150, 127–139 (2015). https://doi.org/10.1007/s10549-015-3287-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-015-3287-5