Abstract
The frequent alterations of the PI3K/Akt/mTOR-growth signaling pathway are proposed mechanisms for resistance to endocrine therapy in breast cancer, partly through regulation of estrogen receptor α (ER) activity. Reliable biomarkers for treatment prediction are required for improved individualized treatment. We performed a retrospective immunohistochemical analysis of primary tumors from 912 postmenopausal patients with node-negative breast cancer, randomized to either tamoxifen or no adjuvant treatment. Phosphorylated (p) Akt-serine (s) 473, p-mTOR-s2448, and ER phosphorylations-s167 and -s305 were evaluated as potential biomarkers of prognosis and tamoxifen treatment efficacy. High expression of p-mTOR indicated a reduced response to tamoxifen, most pronounced in the ER+/progesterone receptor (PgR) + subgroup (tamoxifen vs. no tamoxifen: hazard ratio (HR), 0.86; 95 % confidence interval (CI), 0.31–2.38; P = 0.78), whereas low p-mTOR expression predicted tamoxifen benefit (HR, 0.29; 95 % CI, 0.18–0.49; P = 0.000002). In addition, nuclear p-Akt-s473 as well as p-ER at -s167 and/or -s305 showed interaction with tamoxifen efficacy with borderline statistical significance. A combination score of positive pathway markers including p-Akt, p-mTOR, and p-ER showed significant association with tamoxifen benefit (test for interaction; P = 0.029). Cross-talk between growth signaling pathways and ER-signaling has been proposed to affect tamoxifen response in hormone receptor-positive breast cancer. The results support this hypothesis, as an overactive pathway was significantly associated with reduced response to tamoxifen. A clinical pre-treatment test for cross-talk markers would be a step toward individualized adjuvant endocrine treatment with or without the addition of PI3K/Akt/mTOR pathway inhibitors.
Similar content being viewed by others
Introduction
Membrane-bound growth factor receptors, such as the four epidermal growth factor receptors and the insulin-like growth factor 1 receptor, activate the pathway phosphatidylinositol 3-kinase (PI3K)/Akt/mammalian targeted of rapamycin (mTOR) and the ras-raf-MAP kinase axis to induce essential tumor cell promoting effects such as survival, proliferation, and translation. Cross-talk and feed-back loops within the pathways make up a complex signaling network complicating development of targeted treatments and the establishment of reliable biomarkers [1].
Human epidermal growth factor receptor 2 (HER2) overexpressed simultaneously with the estrogen receptor α (ER) is a proposed mechanism of endocrine resistance [2–4]. Activation of downstream pathways, frequently represented by PIK3CA mutations in clinically HER2-negative breast cancer, leading to Akt activation, seems to play an important role for breast cancer patients relapsing after adjuvant endocrine treatment [5]. Growth factor signals promote phosphorylation of the ER, thereby altering the receptor conformation, its affinity to coregulators, and the transcriptional activity [6–8]. Ligand-independent ER phosphorylation in vitro resulted in activation of the ERE-promoter region, leading to an altered sensitivity to the selective ER modulator tamoxifen [9]. mTORC1, a highlighted protein complex regulating ER phosphorylation at serine 167 through S6 kinase 1 (S6K1), has been reported to play a central role in oncogenic maintenance by controlling growth signaling, translation, metabolism, and autophagy [10–12].
Double inhibition of ER and mTOR signaling shows promising results for patients who have progressed during endocrine treatment. For adjuvant therapy, there is a need for new biomarkers for selection of patients who may benefit from the combined therapy and those who may have excellent prognosis with endocrine monotherapy. We evaluated the p-mTOR-s2448, p-Akt-s473, and p-ER-s167/s305 status in a large series of tumors from women diagnosed with breast cancer, randomized to either adjuvant tamoxifen or local treatment alone. The single and combined targets served as markers for pathway activation and the expression was evaluated with regard to prognosis and tamoxifen response.
Materials and methods
The present study was designed and presented with regard to the reporting recommendations for tumor marker prognostic studies (REMARK) guidelines [13].
Patients and TMA construction
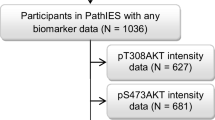
During the years 1976 through 1990, a cohort of Swedish postmenopausal breast cancer patients was included in a controlled trial to evaluate tamoxifen as adjuvant treatment [14]. Patients in the tamoxifen arm were treated for 2 years, and thereafter, randomized to continued treatment for three more years or no more treatment. In the present study, women with low-risk tumors, defined as node negative and with tumor diameter ≤30 mm, were included. Patients were treated either with modified radical mastectomy or breast-conserving therapy and radiation therapy to the breast with a total dose of 50 Gy with 2 Gy per fraction, 5 days weekly, for about 5 weeks. Patient demographic data are presented in Supplementary Fig. 1. Median period of follow-up was 18 years. Methods for tissue microarray (TMA) construction and determination of ERα status, progesterone receptor (PgR) status, and HER2 status were previously described [15]. ER- and PgR positivity was defined as 10 % or more positive tumor cells.
Immunohistochemistry
Immunohistochemistry was performed on TMAs consisting of samples from 912 tumors with three cores from each tumor, using the PT-link rinse station for deparaffinization and antigen retrieval for 20 min at 96 °C (DakoCytomation, Glostrup, Denmark). Sections were placed in 3 % H2O2 in methanol for 5 min to inactivate endogenous peroxidase, incubated with serum-free protein block (Spring Bioscience, Freemont, CA) for 10 min, and incubated with primary antibodies; p-Akt-s473 (1:33 dilution), p-mTOR-s2448 (1:300), p-ER-s167 (1:400) (Cell Signaling Technologies, Danvers, MA), and p-ER-s305, as previously described [16] (1:300) (Bethyl laboratories, Montgomery, TX) overnight at 4 °C in a moisturized chamber. All slides were washed, incubated with an anti-rabbit antibody DakoCytomation Envision + system labeled with horse radish peroxidase (DakoCytomation) for 30 min at RT. Positive staining was visualized using 3, 3-diaminobenzidine tetrahydrochloride (DAB; Vector Laboratories, CA). Nuclei were counterstained with hematoxylin before mounting. Images were generated using an Olympus SC20 camera with a Leica ×20 and ×40 objective. P-Akt whole slide images with ×200 magnification were generated from a Scanscope AT (Aperio, Vista, CA).
Scoring
Staining intensity was evaluated on three separate core biopsies for each tumor. Protein expression in tumor cells was scored by two independent observers. For dissimilar scoring, consensus was reached after a joint reevaluation of the tumor. P-mTOR was visible in the cytoplasm. Expression intensity was evaluated as negative, weak, medium, or strong. As many of the tumors showed more than one intensity grade, each intensity grade was evaluated according to percentage. P-mTOR positivity was defined as strong staining in >25 % of cells. P-Akt was visible in the cytoplasmic and in the nuclear compartments. Expression intensity in each compartment was evaluated as negative, weak, medium, or strong (0, 1, 2, and 3, respectively), and the tumors were additionally evaluated for percentage stained cells where score 0 was <1 %, score 1 was 1–25 %, score 2 was 26–75 %, and score 3 was >75 %. A histological score was calculated by adding intensity to percentage score, with a final score of 0–6. P-Akt positivity was defined as a histological score >3 in the cytoplasm and >4 in the nucleus. The intensity for p-ER-s167 was scored as negative, weak, and strong nuclear staining and nuclear positivity was defined as strong staining in >75 % of cells. P-ER-s167 cytoplasmic staining was evaluated as positive or negative. P-ER-s305 nuclear positivity was defined as visible staining in >1 % of cells and cytoplasmic staining was evaluated as negative or positive.
Antibody validation
The optimal antibody titers were assessed by staining TMA slides and choosing the concentration with the most discriminatory power, with the intensity ranging from negative-to-strong staining among different cases on the same slide. Antibody phospho-specificity was validated by dephosphorylation of proteins using λ-phosphatase (New England Biolabs). Slides were treated with 1,000 units of λ-phosphatase for 2 h at 37 °C followed by immunohistochemical staining according to the protocol used for the respective antibodies. All antibodies were phospho-specific and have been used previously in several studies [16–20].
Statistical analysis
All statistical analyses were performed using Statistica 10. Kaplan–Meier curves were plotted to describe recurrence-free survival (RFS) and differences between groups were evaluated with log-rank tests. Cox regression was used to assess hazard ratios, in univariate and multivariate models, and Pearson Chi-square tests were performed to investigate the interrelations between biological markers. A value of P < 0.05 was considered statistically significant with the exception of the test in Table 1 where the significance limit was set to P < 0.01 to compensate for the multiple testing.
Results
Expression analysis of phosphorylated mTOR and phosphorylated Akt was successful in 821 and 816 tumors, respectively. Activation of mTOR was evaluated with an antibody targeting the mTOR serine 2448 phospho-site, predominantly represented by the mTORC1, the indirect downstream target of Akt [21]. P-mTOR was visible in the extranuclear compartment, and strongly expressed in 11.8 % of tumors. Akt activation was measured by targeting the phosphorylated serine 473 residue of Akt, which is required for full activity of the kinase [1]. A high expression of p-Akt in the cytoplasm and in the nucleus was found in 59.7 and 56.1 % of tumors, respectively. Cross-talk between the PI3K/Akt/mTOR pathway and ER-signaling has been suggested as a mechanism of endocrine resistance in breast tumors; therefore, we added two phosphorylation sites on the ER to the analyses. P-mTOR correlated with nuclear expression of p-ERs167 and with PgR positivity. High cytoplasmic p-Akt was more frequent in tumors with a positive HER2 status, and with cytoplasmic p-ER. P-Akt in the nucleus correlated with small tumor size, ER-positive status, and with nuclear p-ER (Table 1).
Prognosis
For patients who received no systemic therapy, no prognostic value was detected for either p-mTOR or p-Akt, no matter of cut-off value and subgroup classification, analyzed with the end-point recurrence-free survival (RFS). A better prognosis for patients with high expression of nuclear p-ER-s167 was seen (RFS: HR, 0.71; 95 % CI, 0.45–1.13; P = 0.14) and (breast cancer survival: HR, 0.49; 95 % CI, 0.26–0.96; P = 0.037). This was not evident for cytoplasmic p-ER-s167 expression (data not shown).
Tamoxifen treatment prediction
For patients with ER-positive breast cancer, phospho-protein levels in the tumors were taken into account when comparing recurrence-free survival for tamoxifen-treated patients and patients receiving no endocrine treatment. Low p-mTOR expression was associated with treatment benefit (P = 0.00003; Fig. 1a), whereas high p-mTOR expression indicated reduced response to treatment (P = 0.55; Fig. 1b). Restricting the analysis to patients with PgR-positive tumors further strengthened the results (Fig. 1c, d) and the interaction between p-mTOR and tamoxifen efficacy showed borderline significance in the latter analysis (P = 0.064; Table 2). High expression of p-Akt in the nucleus predicted reduced response to treatment compared with low expression (Table 2; Fig. 1e, f). No treatment predictive value was detected for cytoplasmic expression of p-Akt (low p-Akt, P = 0.0036 vs. high p-Akt, P = 0.0089).
Tamoxifen efficacy in ER-positive patients grouped according to single biomarker expression, p-mTOR-s2448 (a–b), p-mTOR-s2488 in PgR-positive subgroup (c–d), nuclear p-Akt-s473 (e–f), and nuclear p-ER (s167 and/or s305) (g–h). Treatment response was reduced in case of high expression of either of the biomarkers, individually
Phosphorylations of the ER and their role in tamoxifen response and ligand-independent receptor activation have been discussed during the past few years. Previously, we showed an association of p-ER-s305 with a decreased tamoxifen efficacy [16]. In addition, the serine 167 was evaluated in the present study. Alone, the p-ER-s167 did not render significant interaction with tamoxifen efficacy comparing low and high expression. However, the data pointed toward a decreased treatment response, rather than the opposite (P (low) = 0.00018 vs. P (high) = 0.16; Table 2)). As both ER phospho-sites were associated with reduced response to tamoxifen, a p-ER variable, including either one or both of the sites, was constructed. The combined p-ER variable exhibited stronger treatment predictive value than both sites separately, showing borderline significance in the test for interaction (Table 2). The p-ER variable was also combined with the p-mTOR-s2448 and the p-Akt-s473 markers, respectively, and the two variables were further analyzed in relation to tamoxifen benefit. Both combinations indicated less benefit when both markers were positive, most evident when p-Akt was combined with p-ER (Table 2; Fig. 2).
All studied biomarkers contributed more or less to the prediction of tamoxifen resistance. Therefore, we tested a combined score, where the sum of p-Akt, p-mTOR, and p-ER status was used. The score (0–3) showed significant interaction with tamoxifen efficacy (P = 0.029; Table 2) and a comparison of patients with no positive marker, one positive marker, and those with two or three positive markers is shown in Fig. 3.
Discussion
In this study, we evaluated markers for cross-talk signaling between the PI3K/Akt/mTOR and ER-pathways and their role for prognosis and tamoxifen response in a large randomized cohort of breast cancer patients with long-term follow-up. We observed strong expression of nuclear p-Akt-s473, cytoplasmic p-mTOR-s2448, and nuclear p-ER-s167 in 56, 12, and 20 % of the tumors, respectively. Correlations between the growth signaling markers and ER phosphorylations were mostly observed as intracellular location specific. P-Akt showed stronger association with the receptor phosphorylations than p-mTOR did, possibly as a result of direct ER interaction with p-Akt and indirect with mTOR. P-mTOR was closer correlated with PgR than with ER status, supporting a functional connection between the two markers.
Bakarakos and collaborators implied that p-mTOR was related to an aggressive phenotype in invasive breast cancer [22]. In our hands, no prognostic value of p-mTOR-s2448 could be detected. The early stage of breast cancer in the present cohort may explain the distinctions between the studies. P-mTOR, as a single biomarker for tamoxifen response, showed close to significant interaction in the ER/PgR-positive subgroup. The PgR has for long been used as a marker of estrogen-dependent tumor growth and an indicator of a functional ER, even though the clinical value of PgR as an endocrine treatment predictive marker has been questioned recently [23, 24]. In vitro, mTORC1 inhibition restored tamoxifen sensitivity in Akt-induced tamoxifen resistant cell lines [25]. The mTORC1 inhibitor rapamycin induced a modest reduction of ER transcriptional activity, while a combinatorial inhibition of mTOR and MEK more significantly reduced ER activity, implying that both the PI3K- and the MAPK-pathways regulate ER driven cell growth [26]. Ongoing clinical studies, most recently the phase III BOLERO-2 trial, investigate the possibility to combine endocrine treatment with mTOR inhibitors [27–29]. Results are promising, with higher response rate in combination-therapy arms; however, it is not known what magnitude of benefit from the combined therapy that would be achieved in the adjuvant setting. To further delineate which patients have the best treatment benefit and who should be spared the side effects of a non-functional therapy, the signaling pathways need to be further investigated.
Nuclear p-Akt was associated with ER positivity, as shown in a previous publication also reporting a better prognosis for high p-Akt in the nucleus but not in the cytoplasm [30]. Spears et al. [31] recently reported a prognostic value of p-Akt1-t308 but not of p-Akt2-t309. Hence, the lack of prognostic value for p-Akt-s473 expression in the present study may reflect the balanced prognostic value of activated Akt1 and Akt2. Akt-induced tamoxifen resistance was shown in vitro and in vivo to partly depend on mTOR signaling [25]. To completely activate Akt, the serine 473 is crucial. Threonine 308 phosphorylation in the absence of serine 473 phosphorylation rendered 60 % Akt activity, seen after double inhibition of mTORC1 and mTORC2 [1]. We, therefore, chose to analyze the serine 473 phospho-expression. As a single marker, nuclear localized p-Akt tended to predict resistance to treatment. Fifteen years after surgery, the tamoxifen-treated group showed similar RFS as the untreated group, indicating that tamoxifen treatment no longer improved RFS in the p-Akt high-expressing group but remained important for the low p-Akt-expressing group. Most previous studies of activated Akt and hormone treatment resistance lack untreated control groups, complicating the search for the actual treatment effect as the prognostic value of the biomarker may bias the result [32–34]. Combining p-Akt with p-mTOR rendered similar results as p-Akt alone, with initial treatment response. Akt has mainly been studied as a kinase upstream of mTORC1. Notably, the mTORC2 is necessary for p-Akt-s473 [35]. The p-mTOR-s2448, used in this study, is mainly a marker of mTORC1 [21]. Further studies involving p-mTORC2 and p-Akt will assess whether their connection is involved in treatment response.
An improved breast cancer survival in the systemically untreated group was detected for patients with high expression of p-ER-s167 in the tumor, compared with lower expression. This finding was in line with previous studies [36, 37]. In addition, several smaller studies found p-ER-s167 to provide an improved clinical outcome in tamoxifen-treated patients [20, 38]. Skliris et al. [39] proposed p-ER-s167 to be a good factor in a cohort of tamoxifen-treated breast cancer patients, suggesting an intact estrogen-dependent targetable growth. To our knowledge, the present study was the first based on a randomized trial to analyze p-ER-s167 in the context of predicting tamoxifen response. Abundant expression of p-ER-s167 was not a marker for increased tamoxifen sensitivity. As a single marker, p-ER-s167 showed no significant interaction. An additive role in combination with other markers to detect cross-talk dependent tamoxifen resistance was noted.
The connection between growth signaling pathways and the ER is a proposed mechanism for tamoxifen resistance [40, 41]. The ER is phosphorylated at serine 167 by the mTORC1 substrate S6K1 and by the MAPK target p90 ribosomal protein S6kinase (RSK) [12]. IGF-regulated signaling phosphorylated ER at serine 167 through Akt, and the signal was rapamycin sensitive, suggesting a signal from Akt, via mTOR to ER activation [42]. Our clinical data are in line with the results from the in vitro studies and demonstrated an association between Akt/mTOR signaling and ER phosphorylation. The phosphorylations have previously in retrospective clinical studies and in vitro been reported to reduce response to tamoxifen and activate the receptor ligand-independently [3]. Combining either p-mTOR or p-Akt with p-ER led to prediction of decreased tamoxifen response. Using all the available biomarkers in combination increased the size of the subgroup populations with reduced benefit. For patients with tumors expressing no markers, the response to tamoxifen was clearly significant, while in the group expressing one marker the response to treatment tended to be reduced; and in the group with two or three positive markers, the response was non-significant. The interaction was significant when analyzing all groups together.
In conclusion, our data support the model of cross-talk between growth factor signaling and ER phosphorylation and its association with tamoxifen resistance. The PI3K/Akt pathway is frequently deregulated in breast cancer, providing a mechanism for cells to sustain growth despite endocrine treatment. Phosphorylated mTOR, as a single predictive marker of reduced tamoxifen response, may be applicable in the ER/PgR-positive subgroup. However, we suggest a multiple phospho-marker test including p-Akt-s473, p-mTOR-s2448, and p-ER-s167/s305. With at least two positive markers, untreated patients showed similar recurrence-free survival as the tamoxifen-treated patients. We suggest this pathway to be further evaluated considering PI3K/mTOR inhibitors in addition to endocrine treatment.
Abbreviations
- DAB:
-
3,3-Diaminobenzidine tetrahydrochloride
- C:
-
Celcius
- CI:
-
Confidence interval
- EGFR:
-
Epidermal growth factor receptor
- ER:
-
Estrogen receptor α
- ERE:
-
Estrogen response element
- Erk:
-
Extracellular signal-regulated kinase
- Gy:
-
Gray
- HR:
-
Hazard ratio
- HER2:
-
Human epidermal growth factor receptor 2
- IHC:
-
Immunohistochemistry
- IGF:
-
Insulin-like growth factor
- IGFR1:
-
Insulin-like growth factor 1 receptor
- mTOR:
-
Mammalian target of rapamycin
- mTORC:
-
Mammalian target of rapamycin complex
- min:
-
Minutes
- MAPK:
-
Mitogen-activated protein kinase
- MEK:
-
Mitogen-activated protein kinase extracellular signal-regulated kinase kinase
- PI3K:
-
Phosphatidylinositol 3-kinase
- PIK3CA:
-
Phosphatidylinositol 3-kinase catalytic alpha polypeptide gene
- p:
-
Phosphorylated
- PgR:
-
Progesterone receptor
- Raf:
-
Rapidly accelerated fibrosarcoma
- RFS:
-
Recurrence–free survival
- RT:
-
Room temperature
- S6K1:
-
S6 kinase 1
- s:
-
Serine
- TMA:
-
Tissue microarray
- vs:
-
Versus
References
Rodrik-Outmezguine VS, Chandarlapaty S, Pagano NC, Poulikakos PI, Scaltriti M, Moskatel E et al (2011) mTOR Kinase Inhibition Causes Feedback-Dependent Biphasic Regulation of AKT Signaling. Cancer Discov 1(3):248–259
Benz CC, Scott GK, Sarup JC, Johnson RM, Tripathy D, Coronado E et al (1992) Estrogen-dependent, tamoxifen-resistant tumorigenic growth of MCF-7 cells transfected with HER2/neu. Breast Cancer Res Treat 24(2):85–95
Shou J, Massarweh S, Osborne CK, Wakeling AE, Ali S, Weiss H et al (2004) Mechanisms of tamoxifen resistance: increased estrogen receptor-HER2/neu cross-talk in ER/HER2-positive breast cancer. J Natl Cancer Inst 96(12):926–935
Dowsett M, Houghton J, Iden C, Salter J, Farndon J, A’Hern R et al (2006) Benefit from adjuvant tamoxifen therapy in primary breast cancer patients according oestrogen receptor, progesterone receptor, EGF receptor and HER2 status. Ann Oncol 17(5):818–826
Kirkegaard T, Witton CJ, McGlynn LM, Tovey SM, Dunne B, Lyon A et al (2005) AKT activation predicts outcome in breast cancer patients treated with tamoxifen. J Pathol 207(2):139–146
Zwart W, Griekspoor A, Berno V, Lakeman K, Jalink K, Mancini M et al (2007) PKA-induced resistance to tamoxifen is associated with an altered orientation of ERalpha towards co-activator SRC-1. EMBO J 26(15):3534–3544
Houtman R, de Leeuw R, Rondaij M, Melchers D, Verwoerd D, Ruijtenbeek R et al (2012) Serine-305 phosphorylation modulates estrogen receptor alpha binding to a coregulator peptide array, with potential application in predicting responses to tamoxifen. Mol Cancer Ther 11(4):805–816
Duplessis TT, Williams CC, Hill SM, Rowan BG (2011) Phosphorylation of estrogen receptor alpha at serine 118 directs recruitment of promoter complexes and gene-specific transcription. Endocrinology 152(6):2517–2526
Tharakan R, Lepont P, Singleton D, Kumar R, Khan S (2008) Phosphorylation of estrogen receptor alpha, serine residue 305 enhances activity. Mol Cell Endocrinol 295(1–2):70–78
Meric-Bernstam F, Gonzalez-Angulo AM (2009) Targeting the mTOR signaling network for cancer therapy. J Clin Oncol 27(13):2278–2287
Holz MK, Blenis J (2005) Identification of S6 kinase 1 as a novel mammalian target of rapamycin (mTOR)-phosphorylating kinase. J Biol Chem 280(28):26089–26093
Yamnik RL, Holz MK (2010) mTOR/S6K1 and MAPK/RSK signaling pathways coordinately regulate estrogen receptor alpha serine 167 phosphorylation. FEBS Lett 584(1):124–128
McShane LM, Altman DG, Sauerbrei W, Taube SE, Gion M, Clark GM (2006) REporting recommendations for tumor MARKer prognostic studies (REMARK). Breast Cancer Res Treat 100(2):229–235
Rutqvist LE, Johansson H (2007) Long-term follow-up of the randomized Stockholm trial on adjuvant tamoxifen among postmenopausal patients with early stage breast cancer. Acta Oncol 46(2):133–145
Jansson A, Delander L, Gunnarsson C, Fornander T, Skoog L, Nordenskjold B et al (2009) Ratio of 17HSD1 to 17HSD2 protein expression predicts the outcome of tamoxifen treatment in postmenopausal breast cancer patients. Clin Cancer Res 15(10):3610–3616
Bostner J, Skoog L, Fornander T, Nordenskjold B, Stal O (2010) Estrogen receptor-alpha phosphorylation at serine 305, nuclear p21-activated kinase 1 expression, and response to tamoxifen in postmenopausal breast cancer. Clin Cancer Res 16(5):1624–1633
Sun CH, Chang YH, Pan CC (2011) Activation of the PI3K/Akt/mTOR pathway correlates with tumour progression and reduced survival in patients with urothelial carcinoma of the urinary bladder. Histopathology 58(7):1054–1063
Setsu N, Yamamoto H, Kohashi K, Endo M, Matsuda S, Yokoyama R et al (2012) The Akt/mammalian target of rapamycin pathway is activated and associated with adverse prognosis in soft tissue leiomyosarcomas. Cancer 118(6):1637–1648
Chung JY, Hong SM, Choi BY, Cho H, Yu E, Hewitt SM (2009) The expression of phospho-AKT, phospho-mTOR, and PTEN in extrahepatic cholangiocarcinoma. Clin Cancer Res 15(2):660–667
Jiang J, Sarwar N, Peston D, Kulinskaya E, Shousha S, Coombes RC et al (2007) Phosphorylation of estrogen receptor-alpha at Ser167 is indicative of longer disease-free and overall survival in breast cancer patients. Clin Cancer Res 13(19):5769–5776
Copp J, Manning G, Hunter T (2009) TORC-specific phosphorylation of mammalian target of rapamycin (mTOR): phospho-Ser2481 is a marker for intact mTOR signaling complex 2. Cancer Res 69(5):1821–1827
Bakarakos P, Theohari I, Nomikos A, Mylona E, Papadimitriou C, Dimopoulos AM et al (2010) Immunohistochemical study of PTEN and phosphorylated mTOR proteins in familial and sporadic invasive breast carcinomas. Histopathology 56(7):876–882
Horwitz KB, McGuire WL (1975) Predicting response to endocrine therapy in human breast cancer: a hypothesis. Science 189(4204):726–727
Davies C, Godwin J, Gray R, Clarke M, Cutter D, Darby S et al (2011) Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet 378(9793):771–784
deGraffenried LA, Friedrichs WE, Russell DH, Donzis EJ, Middleton AK, Silva JM et al (2004) Inhibition of mTOR activity restores tamoxifen response in breast cancer cells with aberrant Akt Activity. Clin Cancer Res 10(23):8059–8067
Ghayad SE, Bieche I, Vendrell JA, Keime C, Lidereau R, Dumontet C et al (2008) mTOR inhibition reverses acquired endocrine therapy resistance of breast cancer cells at the cell proliferation and gene-expression levels. Cancer Sci 99(10):1992–2003
Baselga J, Campone M, Piccart M, Burris HA 3rd, Rugo HS, Sahmoud T et al (2012) Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med 366(6):520–529
Bachelot T, Bourgier C, Cropet C, Ray-Coquard I, Ferrero JM, Freyer G et al (2012) Randomized phase II trial of everolimus in combination with tamoxifen in patients with hormone receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer with prior exposure to aromatase inhibitors: a GINECO study. J Clin Oncol 30(22):2718–2724
Baselga J, Semiglazov V, van Dam P, Manikhas A, Bellet M, Mayordomo J et al (2009) Phase II randomized study of neoadjuvant everolimus plus letrozole compared with placebo plus letrozole in patients with estrogen receptor-positive breast cancer. J Clin Oncol 27(16):2630–2637
Badve S, Collins NR, Bhat-Nakshatri P, Turbin D, Leung S, Thorat M et al (2010) Subcellular localization of activated AKT in estrogen receptor- and progesterone receptor-expressing breast cancers: potential clinical implications. Am J Pathol 176(5):2139–2149
Spears M, Cunningham CA, Taylor KJ, Mallon EA, Thomas JS, Kerr GR et al (2012) Proximity ligation assays for isoform-specific Akt activation in breast cancer identify activated Akt1 as a driver of progression. J Pathol 227(4):481–489
Perez-Tenorio G, Stal O (2002) Activation of AKT/PKB in breast cancer predicts a worse outcome among endocrine treated patients. Br J Cancer 86(4):540–545
Tokunaga E, Kataoka A, Kimura Y, Oki E, Mashino K, Nishida K et al (2006) The association between Akt activation and resistance to hormone therapy in metastatic breast cancer. Eur J Cancer 42(5):629–635
Beelen K, Zwart W, Linn SC (2012) Can predictive biomarkers in breast cancer guide adjuvant endocrine therapy? Nat Rev Clin Oncol 9(9):529–541
Riaz A, Zeller KS, Johansson S (2012) Receptor-specific mechanisms regulate phosphorylation of AKT at Ser473: role of RICTOR in beta1 integrin-mediated cell survival. PLoS ONE 7(2):e32081
Yamashita H, Nishio M, Toyama T, Sugiura H, Kondo N, Kobayashi S et al (2008) Low phosphorylation of estrogen receptor alpha (ERalpha) serine 118 and high phosphorylation of ERalpha serine 167 improve survival in ER-positive breast cancer. Endocr Relat Cancer 15(3):755–763
Motomura K, Ishitobi M, Komoike Y, Koyama H, Nagase H, Inaji H et al (2010) Expression of estrogen receptor beta and phosphorylation of estrogen receptor alpha serine 167 correlate with progression-free survival in patients with metastatic breast cancer treated with aromatase inhibitors. Oncology 79(1–2):55–61
Yamashita H, Nishio M, Kobayashi S, Ando Y, Sugiura H, Zhang Z et al (2005) Phosphorylation of estrogen receptor alpha serine 167 is predictive of response to endocrine therapy and increases postrelapse survival in metastatic breast cancer. Breast Cancer Res 7(5):R753–R764
Skliris GP, Nugent ZJ, Rowan BG, Penner CR, Watson PH, Murphy LC (2010) A phosphorylation code for oestrogen receptor-alpha predicts clinical outcome to endocrine therapy in breast cancer. Endocr Relat Cancer 17(3):589–597
Schiff R, Massarweh SA, Shou J, Bharwani L, Mohsin SK, Osborne CK (2004) Cross-talk between estrogen receptor and growth factor pathways as a molecular target for overcoming endocrine resistance. Clin Cancer Res 10(1 Pt 2):331S–336S
Johnston SR (2006) Clinical efforts to combine endocrine agents with targeted therapies against epidermal growth factor receptor/human epidermal growth factor receptor 2 and mammalian target of rapamycin in breast cancer. Clin Cancer Res 12(3 Pt 2):1061s–1068s
Becker MA, Ibrahim YH, Cui X, Lee AV, Yee D (2011) The IGF pathway regulates ERalpha through a S6K1-dependent mechanism in breast cancer cells. Mol Endocrinol 25(3):516–528
Acknowledgments
Special thanks to pathologist Sten Thorstensson and technician Birgitta Holmlund. This study was supported with grants from the Swedish Cancer Society, the Swedish Research Council, and King Gustaf V Jubilee Fund.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
The authors declare that the study comply with the current laws of Sweden.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
10549_2012_2376_MOESM1_ESM.tif
Supplementary fig. 1 Consort diagram for the randomized Stockholm trial and the patients included in the present study (TIFF 11200 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Bostner, J., Karlsson, E., Pandiyan, M.J. et al. Activation of Akt, mTOR, and the estrogen receptor as a signature to predict tamoxifen treatment benefit. Breast Cancer Res Treat 137, 397–406 (2013). https://doi.org/10.1007/s10549-012-2376-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2376-y