Abstract
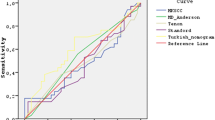
We assessed the MSKCC nomogram performance in predicting SLN metastases in a Chinese breast cancer population. A new model (the SCH nomogram) was developed with clinically relevant variables and possible advantages. Data were collected from 1,545 patients who had a successful SLN biopsy between March 2005 and November 2011. We validated the MSKCC nomogram in the modeling and validation group. Clinical and pathologic features of SLN biopsy in modeling group of 1,000 patients were assessed with multivariable logistic regression to predict the presence of SLN metastasis in breast cancer. The SCH nomogram was created from the logistic regression model and subsequently applied to 545 consecutive SLN biopsies. By multivariate analysis, age, tumor size, tumor location, tumor type, and lymphovascular invasion were identified as independent predictors of SLN metastasis. The SCH nomogram was then developed using the five variables. The new model was accurate and discriminating (with an AUC of 0.7649 in the modeling group) compared to the MSKCC nomogram (with an AUC of 0.7105 in the modeling group). The area under the ROC curve for the SCH nomogram in the validation population is 0.7587. The actual probability trends for the various deciles were comparable to the predicted probabilities. The false-negative rates of the SCH nomogram were 1.67, 3.54, and 8.20 % for the predicted probability cut-off points of 5, 10, and 15 %, respectively. Compared with the MSKCC nomogram, the SCH nomogram has a better AUC with fewer variables and has lower false-negative rates for the low-probability subgroups. The SCH nomogram could serve as a more acceptable clinical tool in preoperative discussions with patients, especially very-low-risk patients. When applied to these patients, the SCH nomogram could be used to safely avoid a SLN procedure. The nomogram should be validated in various patient populations to demonstrate its reproducibility.






Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Krag DN, Anderson SJ, Julian TB et al (2007) Technical outcomes of sentinel-lymph-node resection and conventional axillary-lymph-node dissection in patients with clinically node-negative breast cancer: results from the NSABP B-32 randomised phase III trial. Lancet Oncol 8:881–888
Mansel RE, Fallowfield L, Kissin M et al (2006) Randomized multicenter trial of sentinel node biopsy versus standard axillary treatment in operable breast cancer: the ALMANAC Trial. J Natl Cancer Inst 98:599–609
Veronesi U, Paganelli G, Viale G et al (2006) Sentinel-lymph-node biopsy as a staging procedure in breast cancer: update of a randomised controlled study. Lancet Oncol 7:983–990
Purushotham AD, Upponi S, Klevesath MB, Bobrow L, Millar K, Myles JP, Duffy SW (2005) Morbidity after sentinel lymph node biopsy in primary breast cancer: results from a randomized controlled trial. J Clin Oncol 23:4312–4321
Del Bianco P, Zavagno G, Burelli P et al (2008) Morbidity comparison of sentinel lymph node biopsy versus conventional axillary lymph node dissection for breast cancer patients: results of the sentinella–GIVOM Italian randomised clinical trial. EJSO 34:508–513
Baron RH, Fey JV, Borgen PI, Stempel MM, Hardick KR, Van Zee KJ (2007) Eighteen sensations after breast cancer surgery: a 5-year comparison of sentinel lymph node biopsy and axillary lymph node dissection. Ann Surg Oncol 14:1653–1661
Bevilacqua JL, Kattan MW, Fey JV, Cody HS 3rd, Borgen PI, Van Zee KJ (2007) Doctor, what are my chances of having a positive sentinel node? A validated nomogram for risk estimation. J Clin Oncol 25:3670–3679
Klar M, Foeldi M, Markert S, Gitsch G, Stickeler E, Watermann D (2008) Good prediction of the likelihood for sentinel lymph node metastasis by using the MSKCC nomogram in a German breast cancer population. Ann Surg Oncol 16:1136–1142
Carter CL, Allen C, Henderson DE (1989) Relation of tumour size, lymph node status and survival in 24, 740 breast cancer cases. Cancer 63:181–187
Rosen PP, Groshen S, Saigo PE, Kinne DW, Hellman S (1989) Pathologic prognostic factors in stage I (T1N0M0) and stage II (T1N1M0) breast carcinoma: a study of 644 patients with median follow up of 18 years. J Clin Oncol 7:1239–1251
Quiet CA, Ferguson DJ, Weichselbaum RR, Hellman S (1995) Natural history of node-negative breast cancer: a study of 826 patients with long-term follow-up. J Clin Oncol 13:1144–1151
Barranger E, Coutant C, Flahault A et al (2005) An axilla scoring system to predict non-sentinel lymph node status in breast cancer patients with sentinel lymph node involvement. Breast Cancer Res Treat 91:113–119
Pal A, Provenzano E, Duffy SW, Pinder SE, Purushotham AD (2008) A model for predicting non-sentinel lymph node metastatic disease when the sentinel lymph node is positive. Br J Surg 95:302–309
Kohrt HE, Olshen RA, Bermas HR et al (2008) New models and online calculator for predicting non-sentinel lymph node status in sentinel lymph node positive breast cancer patients. BMC Cancer 8:66
Van Zee KJ, Manasseh DM, Bevilacqua JL et al (2003) A nomogram for predicting the likelihood of additional nodal metastases in breast cancer patients with a positive sentinel node biopsy. Ann Surg Oncol 10:1140–1151
Katz A, Smith BL, Golshan M et al (2008) Nomogram for the prediction of having four or more involved nodes for sentinel lymph node-positive breast cancer. J Clin Oncol 26:2093–2098
Degnim AC, Reynolds C, Pantvaidya G et al (2005) Nonsentinel node metastasis in breast cancer patients: assessment of an existing and a new predictive nomogram. Am J Surg 190:543–550
Kocsis L, Svébis M, Boross G, Sinkό M, Maráz R, Rajtár M, Cserni G (2004) Use and limitations of a nomogram predicting the likelihood of non-sentinel node involvement after a positive sentinel node biopsy in breast cancer patients. Am Surg 70:1019–1024
Alran S, De Rycke Y, Fourchotte V et al (2007) Institute Curie Breast Cancer Study Group Validation and limitations of use of a breast cancer nomogram predicting the likelihood of non-sentinel node involvement after positive sentinel node biopsy. Ann Surg Oncol 14:2195–2201
Klar M, Jochmann A, Foeldi M, Stumpf M, Gitsch G, Stickeler E et al (2008) The MSKCC nomogram for prediction the likelihood of non-sentinel node involvement in a German breast cancer population. Breast Cancer Res Treat 112:523–531
Cserni G (2005) Evaluation of sentinel lymph nodes in breast cancer. Histopathology 46:697–706
Cserni G, Amendoeira I, Apostolikas N et al (2004) Discrepancies in current practice of pathological evaluation of sentinel lymph nodes in breast cancer. Results of questionnaire-based survey by the European Working Gourp for Breast Screening Pathology. J Clin Pathol 57:695–701
Weaver DL, Ashikaga T, Krag DN et al (2011) Effect of occult metastases on survival in node-negative breast cancer. N Engl J Med 364:412–421
Cserni G, Gregori D, Merletti F et al (2004) Non-sentinel node metastases associated with micrometastatic sentinel nodes in breast cancer: metaanalysis of 25 studies. Br J Surg 91:1245–1252
Chen SL, Hoehne FM, Giuliano AE (2007) The prognostic significance of micrometastases in breast cancer: a SEER population-based analysis. Ann Surg Oncol 14:3378–3384
Cserni G, Amendoeira I, Apostolikas N et al (2003) Pathological work-up of sentinel lymph nodes in breast cancer. Review of current data to be considered for the formulation of guidelines. Eur J Cancer 39:1654–1667
Fan L, Zheng Y, Yu KD et al (2009) Breast cancer in a transitional society over 18 years: trends and present status in Shanghai, China. Breast Cancer Res Treat 117:409–416
American Cancer Society (2007) Breast cancer facts and figures 2007–2008. American Cancer Society Inc, Atlanta
Son BH, Kwak BS, Kim JK et al (2006) Changing patterns in the clinical characteristics of Korean patients with breast cancer during the last 15 years. Arch Surg 141:155–160
Lyman GH, Guiliano AE, Somerfield MR et al (2005) The Americal Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early stage breast cancer. J Clin Oncol 23:7703–7720
Giuliano AE, Hunt KK, Ballman KV et al (2011) Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305:569–575
Sakorafas GH, Peros G, Cataliotti L, Vlastos G (2006) Lymphedema following axillary lymph node dissection for breast cancer. Surg Oncol 15:153–165
della Rovere GQ, Bonomi R, Ashley S, Benson JR (2006) Axillary staging in women with small invasive breast tumours. Eur J Surg Oncol 32:733–737
Acknowledgments
The authors thank the studied women for their willingness to cooperate with our study. This research was supported in part by the grants from Research Foundation of Sci-Tech Committee of Shanghai City (No. 54119524); ‘‘Shu Guang’’ Project Foundation of Education Committee of Shanghai City (No.05SG04).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jia-ying Chen and Jia-jian Chen have contributed equally to this paper.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, Jy., Chen, Jj., Yang, Bl. et al. Predicting sentinel lymph node metastasis in a Chinese breast cancer population: assessment of an existing nomogram and a new predictive nomogram. Breast Cancer Res Treat 135, 839–848 (2012). https://doi.org/10.1007/s10549-012-2219-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-012-2219-x