Abstract
Persistent genital arousal disorder/genitopelvic dysesthesia (PGAD/GPD) is characterized by persistent, unwanted physiological genital arousal (i.e., sensitivity, fullness, and/or swelling) in the absence of sexual excitement or desire which can persist for hours to days and causes significant impairment in psychosocial well-being (e.g., distress) and daily functioning. The etiology and course of PGAD/GPD is still relatively unknown and, unsurprisingly, there are not yet clear evidence-based treatment recommendations for those suffering from PGAD/GPD. We present the case of a 58-year-old woman with acquired persistent genital arousal disorder, which began in March 2020; she believed she developed PGAD/GPD due to a period of significant distress and anxiety related to the COVID-19 pandemic. After seeking medical diagnosis and treatment from multiple healthcare providers and trying a combination of pharmacological and medical treatment modalities, she presented for psychological treatment. An integrative therapy approach (3 assessment sessions, 11 treatment sessions), which included cognitive behavior therapy, distress tolerance and emotion regulation skills from dialectical behavior therapy, and mindfulness practice, was utilized. The patient reported improvements anecdotally (e.g., decreased impact on occupational and social functioning, greater self-compassion, less frequent and shorter duration of PGAD/GPD flare-ups, improved ability to cope with PGAD/GPD symptoms, and decreased need for sleeping medication) and on self-report measures (e.g., lower PGAD/GPD catastrophizing, lower anxiety and depression, and greater overall quality of life).We report the use of an integrative (i.e., psychoeducational, cognitive behavioral, dialectical behavioral, and mindfulness-based) intervention, which may be an effective psychological treatment for PGAD/GPD.




Similar content being viewed by others
Availability of Data and Materials
Not applicable.
Code Availability
Not applicable.
Notes
All healthcare treatment occurred in British Columbia, Canada, which has a publicly funded universal health care system.
Existing literature has suggested that the nervous system, including the autonomic nervous system, may be involved in the etiology and/or maintenance of PGAD/GPD (Goldstein et al., 2021; Jackowich et al., 2016; Leiblum et al., 2007). Additionally, factors such as stress have been linked to the onset of PGAD/GPD symptoms (Goldstein et al., 2021). Since the autonomic nervous system responses to stress can include physiological changes such as increased blood pressure, nausea, and vomiting (Ziegler, 2012), it is possible that some of her symptoms which seem unusual with PGAD/GPD are better explained by her response to the stress of the COVID-19 pandemic. Further, several other studies mention similar symptoms (e.g., nausea, vomiting, weight loss, hypertension) being present in PGAD/GPD patients (Goldmeier & Leiblum, 2008; Kamatchi & Ashley-Smith, 2013; Oaklander et al., 2020; Scantlebury & Lucas, 2023).
References
Anderson, F. G., Sweezy, M., & Schwartz, R. C. (2017). Internal Family System: Skills training manual trauma-informed treatment for anxiety, depression, PTSD, & substance abuse. PESI Publishing & Media.
Aswath, M., Pandit, L. V., Kashyap, K., & Ramnath, R. (2016). Persistent genital arousal disorder. Indian Journal of Psychological Medicine, 38(4), 341–343. https://doi.org/10.4103/0253-7176.185942
Beck, A. T., & Steer, R. A. (1993). Beck Anxiety Inventory Manual. New York: Psychological Corporation.
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck Depression Inventory (BDI-II): Manual and questionnaire. New York: Psychological Corporation.
Bergeron, S., Khalifé, S., Dupuis, M.-J., & McDuff, P. (2016). A randomized clinical trial comparing group cognitive-behavioral therapy and a topical steroid for women with dyspareunia. Journal of Consulting and Clinical Psychology, 84(3), 259–268. https://doi.org/10.1037/ccp0000072
Bilal, A., & Cerniglia, L. (2020). Treatment of persistent genital arousal disorder: Single case study. Cogent Psychology, 7(1), 1–8. https://doi.org/10.1080/23311908.2020.1849949
Boerner, K. E., & Rosen, N. O. (2015). Acceptance of vulvovaginal pain in women with provoked vestibulodynia and their partners: Associations with pain, psychological, and sexual adjustment. Journal of Sexual Medicine, 12(6), 1450–1462. https://doi.org/10.1111/jsm.12889
Brotto, L. A., Basson, R., & Luria, M. (2008). A mindfulness-based group psychoeducational intervention targeting sexual arousal disorder in women. Journal of Sexual Medicine, 5(7), 1646–1659. https://doi.org/10.1111/j.1743-6109.2008.00850.x
Brotto, L. A., Bergeron, S., Zdaniuk, B., Driscoll, M., Grabovac, A., Sadownik, L. A., Smith, K. B., & Basson, R. (2019). A comparison of mindfulness-based cognitive therapy vs cognitive behavioral therapy for the treatment of provoked vestibulodynia in a hospital clinic setting. Journal of Sexual Medicine, 16(6), 909–923. https://doi.org/10.1016/j.jsxm.2019.04.002
Brotto, L. A., Stephenson, K. R., & Zippan, N. (2022). Feasibility of an online mindfulness-based intervention for women with sexual interest/arousal disorder. Mindfulness, 13(3), 647–659. https://doi.org/10.1007/s12671-021-01820-4
Crowe, S., Cresswell, K., Robertson, A., Huby, G., Avery, A., & Sheikh, A. (2011). The case study approach. BMC Medical Research Methodology, 11, 100. https://doi.org/10.1186/1471-2288-11-100
Curran, K. A. (2019). Case report: Persistent genital arousal disorder in an adolescent woman. Journal of Pediatric and Adolescent Gynecology, 32(2), 186–188. https://doi.org/10.1016/j.jpag.2018.11.009
Davis, S. N. P., Bergeron, S., Bois, K., Sadikaj, G., Binik, Y. M., & Steben, M. (2015). A prospective 2-year examination of cognitive and behavioral correlates of provoked vestibulodynia outcomes. Clinical Journal of Pain, 31(4), 333–341. https://doi.org/10.1097/AJP.0000000000000128
Dèttore, D., & Pagnini, G. (2020). Persistent genital arousal disorder: A study on an Italian group of female university students. Journal of Sex & Marital Therapy, 47(1), 60–79. https://doi.org/10.1080/0092623X.2020.1804022
Dunkley, C. R., & Brotto, L. A. (2016). Psychological treatments for provoked vestibulodynia: Integration of mindfulness-based and cognitive behavioral therapies. Journal of Clinical Psychology, 72(7), 637–650. https://doi.org/10.1002/jclp.22286
Eibye, S., & Jensen, H. M. (2014). Persistent genital arousal disorder: Confluent patient history of agitated depression, paroxetine cessation, and a tarlov cyst. Case Reports in Psychiatry, 2014. https://doi.org/10.1155/2014/529052
Elkins, G. R., Ramsey, D., & Yu, Y. (2014). Hypnotherapy for persistent genital arousal disorder: A case study. International Journal of Clinical and Experimental Hypnosis, 62(2), 215–223. https://doi.org/10.1080/00207144.2014.869136
Garvey, L. J., West, C., Latch, N., Leiblum, S., & Goldmeier, D. (2009). Report of spontaneous and persistent genital arousal in women attending a sexual health clinic. International Journal of STD & AIDS, 20(8), 519–521. https://doi.org/10.1258/ijsa.2008.008492
Goldfinger, C., Pukall, C. F., Thibault-Gagnon, S., McLean, L., & Chamberlain, S. (2016). Effectiveness of cognitive-behavioral therapy and physical therapy for provoked vestibulodynia: A randomized pilot study. Journal of Sexual Medicine, 13(1), 88–94. https://doi.org/10.1016/j.jsxm.2015.12.003
Goldmeier, D., & Leiblum, S. L. (2008). Interaction of organic and psychological factors in persistent genital arousal disorder in women: A report of six cases. International Journal of STD & AIDS, 19(7), 488–490. https://doi.org/10.1258/ijsa.2007.007298
Goldstein, I., Komisaruk, B. R., Pukall, C. F., Kim, N. N., Goldstein, A. T., Goldstein, S. W., Hartzell-Cushanick, R., Kellogg-Spadt, S., Kim, C. W., Jackowich, R. A., Parish, S. J., Patterson, A., Peters, K. M., & Pfaus, J. G. (2021). International Society for the Study of Women’s Sexual Health (ISSWSH) review of epidemiology and pathophysiology, and a consensus nomenclature and process of care for the management of persistent genital arousal disorder/genito-pelvic dysesthesia (PGAD/GPD). Journal of Sexual Medicine, 18(4), 665–697. https://doi.org/10.1016/j.jsxm.2021.01.172
Hiller, J., & Hekster, B. (2007). Couple therapy with cognitive behavioural techniques for persistent sexual arousal syndrome. Sexual and Relationship Therapy, 22(1), 91–96. https://doi.org/10.1080/14681990600815285
Hofmann, S. G., Sawyer, A. T., Witt, A. A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169–183. https://doi.org/10.1037/a0018555
Hryńko, M., Kotas, R., Pokryszko-Dragan, A., Nowakowska-Kotas, M., & Podemski, R. (2017). Persistent genital arousal disorder–a case report. Psychiatria Polska, 51(1), 117–124. https://doi.org/10.12740/PP/64869
Jackowich, R. A., Pink, L., Gordon, A., Poirier, É., & Pukall, C. F. (2018). An online cross-sectional comparison of women with symptoms of persistent genital arousal, painful persistent genital arousal, and chronic vulvar pain. Journal of Sexual Medicine, 15(4), 558–567. https://doi.org/10.1016/j.jsxm.2018.02.007
Jackowich, R. A., Pink, L., Gordon, A., & Pukall, C. F. (2016). Persistent gential arousal disorder: A review of its conceptualizations, potential origins, impact, and treatment. Sexual Medicine Reviews, 4(4), 329–342. https://doi.org/10.1016/j.sxmr.2016.06.003
Jackowich, R. A., & Pukall, C. F. (2020a). Persistent genital arousal disorder: A biopsychosocial framework. Current Sexual Health Reports, 12(3), 127–135. https://doi.org/10.1007/s11930-020-00268-2
Jackowich, R. A., & Pukall, C. F. (2020b). Prevalence of persistent genital arousal disorder in 2 North American samples. Journal of Sexual Medicine, 17(12), 2408–2416. https://doi.org/10.1016/j.jsxm.2020.09.004
Jette, A. M., Davies, A. R., Cleary, P. D., Calkins, D. R., Rubenstein, L. V., Fink, A., Kosecoff, J., Young, R. T., Brook, R. H., & Delbanco, T. L. (1986). The functional status questionnaire. Journal of General Internal Medicine, 1(3), 143–149. https://doi.org/10.1007/BF02602324
Kamatchi, R., & Ashley-Smith, A. (2013). Persistent genital arousal disorder in a male: A case report and analysis of the cause. British Journal of Medical Practitioners, 6(1), a605.
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., Chapleau, M.-A., Paquin, K., & Hofmann, S. G. (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763–771. https://doi.org/10.1016/j.cpr.2013.05.005
Leiblum, S., Seehuus, M., Goldmeier, D., & Brown, C. (2007). Psychological, medical, and pharmacological correlates of persistent genital arousal disorder. Journal of Sexual Medicine, 4(5), 1358–1366. https://doi.org/10.1111/j.1743-6109.2007.00575.x
Linehan, M. M. (1993). Dialectical behavior therapy for treatment of borderline personality disorder: Implications for the treatment of substance abuse. NIDA Research Monograph, 137, 201–216.
Linehan, M. M. (2015). DBT: Skills training manual. New York: Guilford Publications.
Linehan, M. M., Armstrong, H. E., Suarez, A., Allmon, D., & Heard, H. L. (1991). Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Archives of General Psychiatry, 48(12), 1060–1064. https://doi.org/10.1001/archpsyc.1991.01810360024003
Linehan, M. M., Korslund, K. E., Harned, M. S., Gallop, R. J., Lungu, A., Neacsiu, A. D., McDavid, J., Comtois, K. A., & Murray-Gregory, A. M. (2015). Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: A randomized clinical trial and component analysis. JAMA Psychiatry, 72(5), 475–482. https://doi.org/10.1001/jamapsychiatry.2014.3039
Linton, S. J., & Fruzzetti, A. E. (2014). A hybrid emotion-focused exposure treatment for chronic pain: A feasibility study. Scandinavian Journal of Pain, 5(3), 151–158. https://doi.org/10.1016/j.sjpain.2014.05.008
Martín-Vivar, M., Villena-Moya, A., Mestre-Bach, G., Hurtado-Murillo, F., & Chiclana-Actis, C. (2022). Treatments for persistent genital arousal disorder in women: A scoping review. Journal of Sexual Medicine, 19(6), 961–974. https://doi.org/10.1016/j.jsxm.2022.03.220
Norman-Nott, N., Wilks, C. R., Hesam-Shariati, N., Schroeder, J., Suh, J., Czerwinski, M., Briggs, N. E., Quidé, Y., McAuley, J., & Gustin, S. M. (2022). The No Worries Trial: Efficacy of online dialectical behaviour therapy skills training for chronic pain (iDBT-Pain) using a single case experimental design. Journal of Pain, 23(4), 558–576. https://doi.org/10.1016/j.jpain.2021.10.003
Oaklander, A. L., Sharma, S., Kessler, K., & Price, B. H. (2020). Persistent genital arousal disorder: A special sense neuropathy. Pain Reports, 5(1), e801. https://doi.org/10.1097/PR9.0000000000000801
Pease, E. R., Ziegelmann, M., Vencill, J. A., Kok, S. N., Collins, S., & Betcher, H. K. (2022). Persistent genital arousal disorder (PGAD): A clinical review and case series in support of multidisciplinary management. Sexual Medicine Reviews, 10(1), 53–70. https://doi.org/10.1016/j.sxmr.2021.05.001
Pukall, C., Komisaruk, B. R., & Goldberg, A. E. (2022). Persistent genital arousal disorder/genitopelvic dysesthesia. In Y. Reisman, L. Lowenstein, & F. Tripodi (Eds.), Textbook of rare sexual medicine conditions (1st ed., pp. 37–49). Springer. https://doi.org/10.1007/978-3-030-98263-8
Rashedi, S., Maasoumi, R., Vosoughi, N., & Haghani, S. (2022). The effect of mindfulness-based cognitive-behavioral sex therapy on improving sexual desire disorder, sexual distress, sexual self-disclosure and sexual function in women: A randomized controlled clinical trial. Journal of Sex & Marital Therapy, 48(5), 475–488. https://doi.org/10.1080/0092623X.2021.2008075
Scantlebury, M., & Lucas, R. (2023). Persistent genital arousal disorder: Two case studies and exploration of a novel treatment modality. Women’s Health Reports, 4(1), 84–88. https://doi.org/10.1089/whr.2022.0097
Sullivan, M. J., Bishop, S. R., & Pivik, J. (1995). The pain catastrophizing scale: Development and validation. Psychological Assessment, 7(4), 524–532. https://doi.org/10.1037/1040-3590.7.4.524
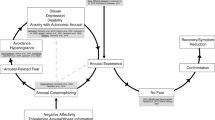
Thomtén, J., & Linton, S. J. (2013). A psychological view of sexual pain among women: Applying the fear-avoidance model. Women’s Health, 9(3), 251–263. https://doi.org/10.2217/whe.13.19
Wohl, A., & Kirschen, G. W. (2018). Betrayal of the body: Group approaches to hypo-sexuality for adult female sufferers of childhood sexual abuse. Journal of Child Sexual Abuse, 27(2), 154–160. https://doi.org/10.1080/10538712.2018.1435597
Ziegler, M. G. (2012). Psychological stress and the autonomic nervous system. In D. Robertson, I. Biaggioni, G. Burnstock, P. A. Low, & J. F. R. Paton (Eds.), Primer on the autonomic nervous system (3rd ed., pp. 291–293). Academic Press. https://doi.org/10.1016/B978-0-12-386525-0.00061-5
Acknowledgements
We would like to express our gratitude to the patient for her openness, willingness, and bravery; thank you for trusting us to tell your story. We would also like to acknowledge Dr. Melanie Altas for her guidance and support.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Not applicable.
Ethical Approval
This is an observational study. The Vancouver Coastal Health Research Ethics Committee has confirmed that no ethical approval is required.
Consent to Participate
Written informed consent was obtained for the patient presented in this case study. Verbal consent was provided during the final treatment session and written consent for the case study was obtained several months after the treatment had ended.
Consent for Publication
The patient provided written informed consent regarding the submission and publication of this case report. The patient also reviewed the final draft of the manuscript and was given the opportunity to provide feedback prior to the manuscript being submitted for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Merwin, K.E., Brotto, L.A. Psychological Treatment of Persistent Genital Arousal Disorder/Genitopelvic Dysesthesia Using an Integrative Approach. Arch Sex Behav 52, 2249–2260 (2023). https://doi.org/10.1007/s10508-023-02617-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-023-02617-3