Abstract
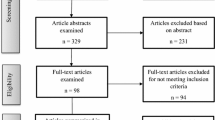
There is a disproportionately high HIV incidence among Black men who have sex with men (MSM) despite equal or lower levels of HIV risk behaviors compared to White MSM. Due to high levels of racial segregation in the U.S., Black MSM have an elevated likelihood of living in neighborhoods that contain psychosocial stressors, which, in turn, may increase behaviors promoting HIV infection. We examined associations between perceived neighborhood problems and sexual behaviors among Black MSM in the Deep South, a population at highest risk of HIV. Data came from the MARI Study, which included Black MSM ages 18–66 years recruited from the Jackson, MS, and Atlanta, GA, metropolitan areas (n = 377). Participants completed questions about neighborhood problems (e.g., excessive noise, heavy traffic/speeding cars and trash/litter) and sexual behaviors (e.g., condomless sex and drug use before or during sex). We used Poisson’s regression model with robust standard errors to estimate the adjusted prevalence ratio (aPR; 95% confidence intervals [CI]) of neighborhood problems (coded as tertiles [tertile 1 = low neighborhood problems, tertile 2 = medium neighborhood problems, tertile 3 = high neighborhood problems] as well as continuously) with sexual behaviors, after adjustment for sociodemographic characteristics and other variables. About one-fourth of the sample reported at least one neighborhood problem, with the most common (31.6%) being no/poorly maintained sidewalks, which indicates an infrastructural problem. In multivariable models, compared to those in the lowest tertile, those reporting more neighborhood problems (tertile 2: aPR = 1.49, 95% CI = 1.04, 2.14 and tertile 3: aPR = 1.53, 95% CI = 1.05, 2.24) reported more drug use before or during sex (p for trend = .027). Neighborhood problems may promote behaviors (e.g., drug use before or during sex) conducive to HIV infection. Structural interventions could improve community infrastructure to reduce neighborhood problems (e.g., no/poorly maintained sidewalks and litter). These interventions may help to reduce HIV incidence among Black MSM in the Deep South.
Similar content being viewed by others
References
Bauermeister, J. A., Connochie, D., Eaton, L., Demers, M., & Stephenson, R. (2017). Geospatial indicators of space and place: A review of multilevel studies of HIV prevention and care outcomes among young men who have sex with men in the United States. Journal of Sex Research,54(4–5), 446–464.
Bauermeister, J. A., Eaton, L., Andrzejewski, J., Loveluck, J., VanHemert, W., & Pingel, E. S. (2015). Where you live matters: Structural correlates of HIV risk behavior among young men who have sex with men in metro detroit. AIDS and Behavior,19(12), 2358–2369.
Bauermeister, J., Eaton, L., & Stephenson, R. (2016). A multilevel analysis of neighborhood socioeconomic disadvantage and transactional sex with casual partners among young men who have sex with men living in metro Detroit. Behavioral Medicine,42(3), 197–204.
Behrens, T., Taeger, D., Wellmann, J., & Keil, U. (2004). Different methods to calculate effect estimates in cross-sectional studies: A comparison between prevalence odds ratio and prevalence ratio. Methods Archive,43(5), 505–509.
Bjornstrom, E. E. S., Ralston, M. L., & Kuhl, D. C. (2013). Social cohesion and self-rated health: The moderating effect of neighborhood physical disorder. American Journal of Community Psychology,52(3–4), 302–312. https://doi.org/10.1007/s10464-013-9595-1.
Boardman, J. D., Finch, B. K., Ellison, C. G., Williams, D. R., & Jackson, J. S. (2001). Neighborhood disadvantage, stress, and drug use among adults. Journal of Health and Social Behavior,42(2), 151–165. https://doi.org/10.2307/3090175.
Bronfenbrenner, U. (1979). The ecology of human development: Experiments by nature and design. Cambridge, MA: Harvard University Press.
Brown, S. C., Mason, C. A., Lombard, J. L., Martinez, F., Plater-Zyberk, E., Spokane, A. R., et al. (2009). The relationship of built environment to perceived social support and psychological distress in hispanic elders: The role of “eyes on the street”. Journals of Gerontology Series B-Psychological Sciences and Social Sciences,64(2), 234–246. https://doi.org/10.1093/geronb/gbn011.
Burdette, H. L., Wadden, T. A., & Whitaker, R. C. (2006). Neighborhood safety, collective efficacy, and obesity in women with young children. Obesity,14(3), 518–525. https://doi.org/10.1038/oby.2006.67.
Buttram, M. E., & Kurtz, S. P. (2013). Risk and protective factors associated with gay neighborhood residence. American Journal of Men’s Health,7(2), 110–118. https://doi.org/10.1177/1557988312458793.
Carpiano, R. M., Kelly, B. C., Easterbrook, A., & Parsons, J. T. (2011). Community and drug use among gay men: The role of neighborhoods and networks. Journal of Health and Social Behavior,52(1), 74–90. https://doi.org/10.1177/0022146510395026.
Centers for Disease Control and Prevention. (2015). Diagnoses of HIV infection in the United States and dependent areas, 2013 (Vol. 25). HIV Surveillance Report. https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2013-vol-25.pdf.
Christian, H., Zubrick, S. R., Foster, S., Giles-Corti, B., Bull, F., Wood, L., et al. (2015). The influence of the neighborhood physical environment on early child health and development: A review and call for research. Health & Place,33, 25–36. https://doi.org/10.1016/j.healthplace.2015.01.005.
Duncan, D. T., Callander, D., Bowleg, L., Park, S. H., Brinkley-Rubinstein, L., Theall, K. P., et al. (in press). An intersectional analysis of life stress, incarceration and sexual health risk practices among cisgender Black gay, bisexual and other men who have sex with men in the Deep South of the United States: The MARI Study. Sexual Health. https://www.publish.csiro.au/SH/justaccepted/SH19062.
Duncan, D. T., Chaix, B., Regan, S. D., Park, S. H., Draper, C., Goedel, W. C., et al. (2018a). Collecting mobility data with GPS methods to understand the HIV environmental riskscape among young black men who have sex with men: A multi-city feasibility study in the deep south. AIDS and Behavior,22(9), 3057–3070. https://doi.org/10.1007/s10461-018-2163-9.
Duncan, D. T., Kapadia, F., & Halkitis, P. N. (2014a). Examination of spatial polygamy among young gay, bisexual, and other men who have sex with men in New York City: The P18 cohort study. International Journal of Environmental Research and Public Health,11(9), 8962–8983. https://doi.org/10.3390/ijerph110908962.
Duncan, D. T., Kapadia, F., Regan, S. D., Goedel, W. C., Levy, M. D., Barton, S. C., et al. (2016). Feasibility and acceptability of global positioning system (GPS) methods to study the spatial contexts of substance use and sexual risk behaviors among young men who have sex with men in New York City: A P18 cohort sub-study. PLoS ONE,11(2), e0147520. https://doi.org/10.1371/journal.pone.0147520.
Duncan, D. T., & Kawachi, I. (2018). Neighborhoods and health (2nd ed.). Oxford, England: Oxford University Press.
Duncan, D. T., Kawachi, I., Subramanian, S. V., Aldstadt, J., Melly, S. J., & Williams, D. R. (2014b). Examination of how neighborhood definition influences measurements of youths’ access to tobacco retailers: A methodological note on spatial misclassification. American Journal of Epidemiology,179(3), 373–381. https://doi.org/10.1093/aje/kwt251.
Duncan, D. T., Kim, B., Al-Ajlouni, Y. A., & Callander, D. (2019). Neighborhood structural-level factors, HIV and communities of color. In B. Bisola & K. Stone (Eds.), HIV/AIDS in U.S. communities of color (2nd ed.). New York: Springer.
Duncan, D. T., Regan, S. D., & Chaix, B. (2018b). Operational neighborhood definitions in health research: Spatial misclassification and other issues. In D. T. Duncan & I. Kawachi (Eds.), Neighborhoods and health (2nd ed., pp. 19–56). Oxford, England: Oxford University Press.
Echeverria, S., Diez-Roux, A. V., Shea, S., Borrell, L. N., & Jackson, S. (2008). Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: The multi-ethnic study of atherosclerosis. Health & Place,14(4), 853–865. https://doi.org/10.1016/j.healthplace.2008.01.004.
Elo, I. T., Mykyta, L., Margolis, R., & Culhane, J. F. (2009). Perceptions of neighborhood disorder: The role of individual and neighborhood characteristics. Social Science Quarterly,90(5), 1298–1320.
Fallon, S. A., Park, J. N., Ogbue, C. P., Flynn, C., & German, D. (2017). Awareness and acceptability of pre-exposure HIV prophylaxis among men who have sex with men in Baltimore. AIDS and Behavior,21(5), 1268–1277.
Frye, V., Koblin, B., Chin, J., Beard, J., Blaney, S., Halkitis, P., et al. (2010). Neighborhood-level correlates of consistent condom use among men who have sex with men: A multi-level analysis. AIDS and Behavior,14(4), 974–985. https://doi.org/10.1007/s10461-008-9438-5.
Frye, V., Latka, M. H., Koblin, B., Halkitis, P. N., Putnam, S., Galea, S., et al. (2006). The urban environment and sexual risk behavior among men who have sex with men. Journal of Urban Health,83(2), 308–324. https://doi.org/10.1007/s11524-006-9033-x.
Frye, V., Nandi, V., Egan, J. E., Cerda, M., Rundle, A., Quinn, J. W., et al. (2017). Associations among neighborhood characteristics and sexual risk behavior among black and white MSM living in a major urban area. AIDS and Behavior,21(3), 870–890.
Fujimoto, K., Flash, C. A., Kuhns, L. M., Kim, J. Y., & Schneider, J. A. (2018). Social networks as drivers of syphilis and HIV infection among young men who have sex with men. Sexually Transmitted Infections,94(5), 365–371. https://doi.org/10.1136/sextrans-2017-053288.
Gallo, L. C., Bogart, L. M., Vranceanu, A. M., & Matthews, K. A. (2005). Socioeconomic status, resources, psychological experiences, and emotional responses: A test of the reserve capacity model. Journal of Personality and Social Psychology,88(2), 386–399. https://doi.org/10.1037/0022-3514.88.2.386.
Gebreab, S. Y., Riestra, P., Gaye, A., Khan, R. J., Xu, R. H., Davis, A. R., et al. (2016). Perceived neighborhood problems are associated with shorter telomere length in African American women. Psychoneuroendocrinology,69, 90–97. https://doi.org/10.1016/j.psyneuen.2016.03.018.
Hermanstyne, K. A., Green, H. D., Cook, R., Tieu, H. V., Dyer, T. V., Hucks-Ortiz, C., et al. (2018). Social network support and decreased risk of seroconversion in black MSM: Results of the BROTHERS (HPTN 061) Study. Journal of Acquired Immune Deficiency Syndromes,78(2), 163–168. https://doi.org/10.1097/Qai.0000000000001645.
Hermanstyne, K. A., Green, H. D., Tieu, H.-V., Hucks-Ortiz, C., Wilton, L., & Shoptaw, S. (2019). The association between condomless anal sex and social support among black men who have sex with men (MSM) in six US cities: A study using data from the HIV prevention trials network BROTHERS study (HPTN 061). AIDS and Behavior,23(6), 1387–1395. https://doi.org/10.1007/s10461-018-2315-y.
Hess, K. L., Hu, X., Lansky, A., Mermin, J., & Hall, H. I. (2017). Lifetime risk of a diagnosis of HIV infection in the United States. Annals of Epidemiology,27(4), 238–243.
Hickson, D. A., Mena, L. A., Wilton, L., Tieu, H. V., Koblin, B. A., Cummings, V., & Mayer, K. H. (2017). Sexual networks, dyadic characteristics, and HIV acquisition and transmission behaviors among black men who have sex with men in 6 US cities. American Journal of Epidemiology,185(9), 786–800. https://doi.org/10.1093/aje/kww144.
Hickson, D. A., Truong, N. L., Smith-Bankhead, N., Sturdevant, N., Duncan, D. T., Schnorr, J., & Mena, L. A. (2015). Rationale, design and methods of the ecological study of sexual behaviors and HIV/STI among African American men who have sex with men in the southeastern United States (The MARI Study). PLoS ONE,10(12), e0143823. https://doi.org/10.1371/journal.pone.0143823.
Hoots, B. E., Finlayson, T., Nerlander, L., Paz-Bailey, G., Group, N. H. B. S. S., Wortley, P., et al. (2016). Willingness to take, use of, and indications for pre-exposure prophylaxis among men who have sex with men—20 US cities, 2014. Clinical Infectious Diseases,63(5), 672–677.
Kelly, B. C., Carpiano, R. M., Easterbrook, A., & Parsons, J. T. (2012). Sex and the community: the implications of neighbourhoods and social networks for sexual risk behaviours among urban gay men. Sociology of Health & Illness,34(7), 1085–1102. https://doi.org/10.1111/j.1467-9566.2011.01446.x.
Kleinhans, R., & Bolt, G. (2014). More than just fear: On the intricate interplay between perceived neighborhood disorder, collective efficacy, and action. Journal of Urban Affairs,36(3), 420–446. https://doi.org/10.1111/juaf.12032.
Kramer, M. R. (2018). Residential segregation and health. In D. T. Duncan & I. Kawachi (Eds.), Neighborhoods and health (2nd ed., pp. 321–356). Oxford, England: Oxford University Press.
Latkin, C. A., Tieu, H. V., Fields, S., Hanscom, B. S., Connor, M., Hanscom, B., et al. (2017). Social network factors as correlates and predictors of high depressive symptoms among black men who have sex with men in HPTN 061. AIDS and Behavior,21(4), 1163–1170. https://doi.org/10.1007/s10461-016-1493-8.
Lieb, S., Prejean, J., Thompson, D. R., Fallon, S. J., Cooper, H., Gates, G. J., et al. (2011). HIV prevalence rates among men who have sex with men in the southern United States: Population-based estimates by race/ethnicity. AIDS and Behavior,15(3), 596–606. https://doi.org/10.1007/s10461-010-9820-y.
Mauck, D. E., Sheehan, D. M., Fennie, K. P., Maddox, L. M., & Trepka, M. J. (2018). Role of gay neighborhood status and other neighborhood factors in racial/ethnic disparities in retention in care and viral load suppression among men who have sex with men, Florida, 2015. AIDS and Behavior,22(9), 2978–2993. https://doi.org/10.1007/s10461-018-2032-6.
McNair, O. S., Gipson, J. A., Denson, D., Thompson, D. V., Sutton, M. Y., & Hickson, D. A. (2018). The associations of resilience and HIV risk behaviors among black gay, bisexual, other men who have sex with men (MSM) in the Deep South: The MARI study. AIDS and Behavior,22(5), 1679–1687. https://doi.org/10.1007/s10461-017-1881-8.
McNutt, L. A., Wu, C., Xue, X., & Hafner, J. P. (2003). Estimating the relative risk in cohort studies and clinical trials of common outcomes. American Journal of Epidemiology,157(10), 940–943.
Millett, G. A., Flores, S. A., Peterson, J. L., & Bakeman, R. (2007). Explaining disparities in HIV infection among black and white men who have sex with men: A meta-analysis of HIV risk behaviors. AIDS,21(15), 2083–2091.
Mills, T. C., Stall, R., Pollack, L., Paul, J. P., Binson, D., Canchola, J., et al. (2001). Health-related characteristics of men who have sex with men: A comparison of those living in “gay ghettos” with those living elsewhere. American Journal of Public Health,91(6), 980–983.
Oster, A. M., Dorell, C. G., Mena, L. A., Thomas, P. E., Toledo, C. A., & Heffelfinger, J. D. (2011). HIV risk among young African American men who have sex with men: A case-control study in Mississippi. American Journal of Public Health,101(1), 137–143. https://doi.org/10.2105/ajph.2009.185850.
Phillips, G., 2nd, Birkett, M., Kuhns, L., Hatchel, T., Garofalo, R., & Mustanski, B. (2015). Neighborhood-level associations with HIV infection among young men who have sex with men in Chicago. Archives of Sexual Behavior,44(7), 1773–1786. https://doi.org/10.1007/s10508-014-0459-z.
Pierce, S. J., Miller, R. L., Morales, M. M., & Forney, J. (2007). Identifying HIV prevention service needs of African American men who have sex with men: An application of spatial analysis techniques to service planning. Journal of Public Health Management and Practice,13, S72–S79.
Quinn, K., Voisin, D. R., Bouris, A., & Schneider, J. (2016). Psychological distress, drug use, sexual risks and medication adherence among young HIV-positive Black men who have sex with men: Exposure to community violence matters. AIDS Care,28(7), 866–872. https://doi.org/10.1080/09540121.2016.1153596.
Raymond, H. F., Chen, Y. H., Syme, S. L., Catalano, R., Hutson, M. A., & McFarland, W. (2014). The role of individual and neighborhood factors: HIV acquisition risk among high-risk populations in San Francisco. AIDS and Behavior,18(2), 346–356. https://doi.org/10.1007/s10461-013-0508-y.
Reif, S., Pence, B. W., Hall, I., Hu, X., Whetten, K., & Wilson, E. (2015). HIV diagnoses, prevalence and outcomes in nine southern states. Journal of Community Health,40(4), 642–651. https://doi.org/10.1007/s10900-014-9979-7.
Reif, S. S., Whetten, K., Wilson, E. R., McAllaster, C., Pence, B. W., Legrand, S., et al. (2014). HIV/AIDS in the Southern USA: A disproportionate epidemic. AIDS Care,26(3), 351–359. https://doi.org/10.1080/09540121.2013.824535.
Ross, C. E., & Mirowsky, J. (1999). Disorder and decay—The concept and measurement of perceived neighborhood disorder. Urban Affairs Review,34(3), 412–432. https://doi.org/10.1177/10780879922184004.
Sampson, R. J., & Raudenbush, S. W. (1999). Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. American Journal of Sociology,105(3), 603–651. https://doi.org/10.1086/210356.
Sampson, R. J., & Raudenbush, S. W. (2004). Seeing disorder: Neighborhood stigma and the social construction of “Broken windows”. Social Psychology Quarterly,67(4), 319–342. https://doi.org/10.1177/019027250406700401.
Schmidt, N. M., Nguyen, Q. C., & Osypuk, T. L. (2018). Experimental and quasi-experimental designs in neighborhood health effects research: Strengthening causal inference and promoting translation. In D. T. Duncan & I. Kawachi (Eds.), Neighborhoods and health (pp. 155–191). Oxford, England: Oxford University Press.
Schneider, J., Michaels, S., & Bouris, A. (2012). Family network proportion and HIV risk among black men who have sex with men. Journal of Acquired Immune Deficiency Syndromes,61(5), 627–635. https://doi.org/10.1097/QAI.0b013e318270d3cb.
Singh, S., Song, R. G., Johnson, A. S., McCray, E., & Hall, H. I. (2018). HIV incidence, prevalence, and undiagnosed infections in US men who have sex with men. Annals of Internal Medicine,168(10), 685–694. https://doi.org/10.7326/m17-2082.
South, E. C., Kondo, M. C., Cheney, R. A., & Branas, C. C. (2015). Neighborhood blight, stress, and health: A walking trial of urban greening and ambulatory heart rate. American Journal of Public Health,105(5), 909–913.
Steptoe, A., & Feldman, P. J. (2001). Neighborhood problems as sources of chronic stress: Development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of Behavioral Medicine,23(3), 177–185.
Stevens, R., Icard, L., Jemmott, J. B., O’Leary, A., Rutledge, S., Hsu, J., et al. (2017). Risky trade: Individual and neighborhood-level socio-demographics associated with transactional sex among urban African American MSM. Journal of Urban Health,94(5), 676–682.
Thompson, M. L., Myers, J. E., & Kriebel, D. (1998). Prevalence odds ratio or prevalence ratio in the analysis of cross sectional data: what is to be done? Occupational and Environmental Medicine,55(4), 272–277.
Tieu, H. V., Liu, T. Y., Hussen, S., Connor, M., Wang, L., Buchbinder, S., et al. (2015). Sexual networks and HIV risk among black men who have sex with men in 6 US cities. PLoS ONE,10(8), e0134085. https://doi.org/10.1371/journal.pone.0134085.
Tobin, K. E., Latkin, C. A., & Curriero, F. C. (2014). An examination of places where African American men who have sex with men (MSM) use drugs/drink alcohol: A focus on social and spatial characteristics. International Journal of Drug Policy,25(3), 591–597. https://doi.org/10.1016/j.drugpo.2013.12.006.
Acknowledgements
Dr. Hickson received support from R25MH083620, Dr. Timothy Flanigan, Principal Investigator). This project was supported by a Grant from the Centers for Disease Control and Prevention (Grant #U01PS003315, Dr. DeMarc Hickson, Principal Investigator). We thank William Goedel for conducting the initial background research, we thank Yazan Al-Ajlouni for formatting the references, and we thank the participants for engaging in this study.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individuals included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Duncan, D.T., Sutton, M.Y., Park, S.H. et al. Associations Between Neighborhood Problems and Sexual Behaviors Among Black Men Who Have Sex with Men in the Deep South: The MARI Study. Arch Sex Behav 49, 185–193 (2020). https://doi.org/10.1007/s10508-019-01619-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10508-019-01619-4