Abstract
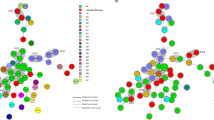
A total of 35 Brazilian isolates of Clostridium difficile from faecal stools and four isolates from hospital environments were analyzed by PCR ribotyping. A whole cell protein profile (as an alternative for serogrouping), in vitro toxin production and susceptibility to vancomycin, metronidazole and clindamycin were also investigated. All strains were typeable by both phenotypic and genotypic methods, and a total of 13 different PCR ribotypes were identified, of which seven (132, 133, 134, 135, 136, 142 and 143) were considered new types and accounted for 78.5% of all samples evaluated (including hospital environments). A non-toxigenic C. difficile PCR ribotype 133 was detected in all children groups examined (inpatients, outpatients and healthy children), whilst toxigenic PCR ribotypes 015, 131, 134 and 135 were associated mostly with symptomatic children. Serogroups G and D were disseminated both in patients from the community and from the pediatric hospital, with group G prevalent among outpatient children. All strains were susceptible to vancomycin and metronidazole but high levels of resistance to clindamycin were found, especially among serogroups G and D. Co-existence of different ribotypes and serogroups in the same individual was observed. The new seven ribotypes found in this investigation may represent strains characteristic of this region of Brazil.
Similar content being viewed by others
Abbreviations
- AAD:
-
Antibiotic-associated diarrhea
- PMC:
-
Pseudomembranous colitis
- PRAS:
-
Pre-reduced Anaerobically Sterilized
References
Al-Barrak A, Embil J, Dick B et al (1999) An outbreak of toxin A negative, toxin B positive Clostridium difficile-associated diarrhea in a Canadian tertiary-care hospital. Canada Communicable Dis Rep 25:1–3
Antunes ENF, Ferreira EO, Vallim DC et al (2002) Pattern III Non-toxigenic Bacteroides fragilis (NTBF) Strains in Brazil. Anaerobe 8:17–22
Al Saif N, Brazier JS (1996) The distribution of Clostridium difficile in the environment of South Wales. J Med Microbiol 45:133–137
Bowman RA, Riley TV (1986) Isolation of Clostridium difficile from stored specimens and comparative susceptibility of various tissues culture cell lines to cytotoxin. FEMS Microbiol Lett 34:31–35
Cerquetti M, Luzzi I, Caprioli A et al (1995) Role of Clostridium difficile in childhood diarrhea. Pediatr Infect Dis J 14:598–603
Delmée M, Laroche Y, Avesani V et al (1986) Comparison of serogrouping and polyacrylamide gel electrophoresis for typing Clostridium difficile. J Clin Microbiol 24:991–994
Depitre CM, Delmée M, Avesani V et al (1993) Serogroup F strains of Clostridium difficile produce toxin B but not toxin A. J Med Microbiol 38:434–441
Farrell RJ, La Mont JT (2000) Pathogenesis and clinical manifestations of Clostridium difficile diarrhea and colitis. Curr Top Microbiol Immunol 250:109–125
Ferroni A, Merckx J, Ancelle T et al (1997) Nosocomial outbreak of Clostridium difficile diarrhea in a pediatric service. Eur J Clin Microbiol Infect Dis 16:928–933
Harmon T, Burkhart G, Applebaum H (1992) Perforated pseudomembranous colitis in the breast-fed infant. J Pediatr Surg 27:744–746
Johnson S, Sambol SP, Brazier JP et al (2003) International typing study of toxin A-negative, toxin B-positive Clostridium difficile variants. J Clin Microbiol 41:1543–1547
Kato H, Kita H, Karasawa T et al (2001) Colonization and transmission of Clostridium difficile in healthy individuals examined by PCR ribotyping and pulsed-field gel electrophoresis. J Med Microbiol 50:720–727
Kim K, Dupont MD, Pickering LK (1983) Outbreaks of diarrhea associated with Clostridium difficile and its toxin in day-care centers: evidence of person-to-person spread. J Pediatrics 102:376–382
Lawson ME, Welch A (1993) In-vitro and in-vivo characterization of resistance to colonization with Clostridium difficile. J Med Microbiol 38:103–108
Loo VG, Poirier L, Miller MA et al (2005) A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality. N Engl J Med 353(23):2442–2449
Lyerly DM, Saum KE, Macdonald DK et al (1985) Effects of Clostiridum difficile toxins gives intragastrically to animals. Infect Immun 47:349–352
Lyerly DM, Barroso LA, Wilkins TD et al (1992) Characterization of a toxin A-negative, toxin B-positive of Clostridium difficile. Infect Immun 60:4633–4639
McDonald IC, Killgore GE, Thompson A et al (2005) An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med 353(23):2433–2441
McFarland LV, Brandmaker SA, Guandalini S (2000) Pediatric Clostridium difficile: A phantom menace or clinical reality? J Ped Gastroent Nut 31:220–231
McGowan KL, Kader HA (1999) Clostridium difficile infection in children. Clin Microbiol Newsletter 21:49–53
National Committee for Clinical Laboratory Standards (2004) Methods for antimicrobial susceptibility testing of anerobic bacteria–6th edition: approved standard M11-A6. NCCLS, Villanova, PA
Perelle S, Gilbert M, Bourlioux P et al (1997) Production of a complete binary toxin (actin-specific ADP- ribosyltransferase) by Clostridium difficile CD196. Infect Immun 65:1402–1407
Pinto LJF, Alcides APP, Ferreira EO et al (2003) Incidence and importance of Clostridium difficile in pediatric diarrhoea in Brazil. J Med Microbiol 52:1095–1099
Qualman SJ, Petric M, Karmali MA et al (1990) Clostridium difficile invasion and toxin circulation in fatal pediatric pseudomembranous colitis. Am J Clin Pathol 94:410–416
Stille CJ, Andrade SE, Huang SS et al (2004) Increased use of second-generation macrolide antibiotics for children in nine health plans in the United States. Pediatrics 114 (5):1206–1211
Stubbs SLJ, Brazier JS, O’Neill GL et al (1999) PCR targeted to the 16S-23S rRNA gene intergenic spacer region of Clostridium difficile and construction of a library consisting of 116 different PCR ribotypes. J Clin Microbiol 37:461–463
Stubbs S, Rupnik M, Gilbert M et al (2000) Production of actin-specific ADP-ribosyltransferase (binary toxin) by strains of Clostridium difficile. FEMS Microbiol Lett 186(2):307–312
Sumannen P, Baron EJ, Citron DM et al (1993) Wadsworth Anaerobic bacteriology Manual 5th edn. Wadsworth Health Science, Belmont
Torres JF (1991) Purification and characterization of toxin B from a strain of Clostridium difficile that does not produce toxin A. J Med Microbiol 35:40–44
Vallim DC, Oliveira ICM, Antunes ENF et al (2002) Evaluation of genetic relatedness of Bacteroides fragilis strains isolated from different Sources by AP-PCR and pulsed-field gel electrophoresis assays. Anaerobe 8:192–199
van den Berg RJ, Ameen HAA, Furusawa T et al (2005) Coexistence of multiple PCR-ribotype strains of Clostridium difficile in faecal samples limits epidemiological studies. J Med Microbiol 54:173–179
Warny M, Pepin J, Fang A et al (2005) Toxin production by an emerging strain of Clostridium difficile associated with outbreaks of severe disease in North America and Europe. Lancet 366:1079–1084
Wilson KH (1993) The microecology of Clostridium difficile. Clin Infect Dis 16:S214–S218
Acknowledgements
The authors are grateful to Joaquim Santos Filho for technical assistance, Dr. Claudia Mendonça, Dr. Rafael Duarte and Prof. Dr. Lucia Teixeira (UFRJ) for SDS-PAGE analysis system assistance; Dr. Michel Delmée (Unité de Microbiologie - Université Catholique de Louvain, Bruxelles, Belgium) for reference strains of serogrouping and to medical staff of Pediatric Institute Prof. Martagão Gesteira from UFRJ. This work was supported by grants from the following Institutions: CNPq, Pronex, FUJB and Faperj.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alcides, A.P.P., Brazier, J.S., Pinto, L.J.F. et al. New PCR ribotypes of Clostridium difficile detected in children in Brazil. Antonie van Leeuwenhoek 92, 53–59 (2007). https://doi.org/10.1007/s10482-006-9134-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10482-006-9134-2