Abstract
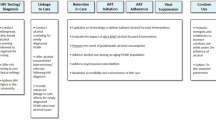
HIV/AIDS remains a significant health threat and alcohol is a robust contributing factor. After 25 years of alcohol challenge studies investigating alcohol-related behavioral risk (ARBR), much has been learned delineating how drinking influences sexual transmission. We examine this research and consider its relevance for interventions in the era of antiretrovirals. We consider prototypic alcohol challenge methods, illustrative findings, and prevention/intervention implications, noting three perspectives: (a) scale up/extend existing interventions, including identifying under-targeted risk groups and intersecting with PrEP/PEP interventions; (b) modify existing interventions by cultivating psychoeducational content related to alcohol expectancies, alcohol myopia, sexual arousal, risk perception, sexual abdication, and condom use resistance; and (c) innovate new interventions through Science of Behavior Change approaches and repurposing ARBR paradigms. Finally, we suggest research directions concluding that until HIV incidence diminishes significantly, psychosocial interventions addressing the nexus of alcohol use, sexual transmission, and adherence to biomedical protocols will be an important priority.
Similar content being viewed by others
References
Albarracín D, Gillette JC, Earl AN, Glasman LR, Durantini MR, Ho MH. A test of major assumptions about behavior change: a comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull. 2005;131(6):856–97.
Centers for Disease Control and Prevention. High-Impact HIV Prevention CDC’s Approach to Reducing HIV Infections in the United States. CDC. 2019. https://www.cdc.gov/hiv/policies/hip/works.html. Accessed 3 Aug 2020
UNAIDS. Global HIV & AIDS statistics—2020 fact sheet. 2020. https://www.unaids.org/en. Accessed 3 Aug 2020.
Stall R, McKusick L, Wiley J, Coates TJ, Ostrow DG. Alcohol and drug use during sexual activity and compliance with safe sex guidelines for AIDS: The AIDS behavioral research project. Health Educ Q. 1986;13(4):359–71.
Hendershot CS, George WH. Alcohol and sexuality research in the AIDS era: Trends in publication activity, target populations and research design. AIDS Behav. 2007;11(2):217–26.
Sullivan MC, Cruess DG, Huedo-Medina TB, Kalichman SC. Substance use, HIV serostatus disclosure, and sexual risk behavior in people living with HIV: an event-level analysis. Arch Sex Behav. 2019;20:1–4.
Simons JS, Simons RM, Maisto SA, Hahn AM, Walters KJ. Daily associations between alcohol and sexual behavior in young adults. Exp Clin Psychopharmacol. 2018;26(1):36–48.
Wray TB, Monti PM, Kahler CW, Guigayoma JP. Using ecological momentary assessment (EMA) to explore mechanisms of alcohol-involved HIV risk behavior among men who have sex with men (MSM). Addict. 2020;115(12):2293–302.
Berry MS, Johnson MW. Does being drunk or high cause HIV sexual risk behavior? A systematic review of drug administration studies. Pharmacol Biochem Behav. 2018;164:125–38.
George WH. Alcohol and sexual health behavior: “What we know and how we know it.” J Sex Res. 2019;56(4–5):409–24.
Rehm J, Shield KD, Joharchi N, Shuper PA. Alcohol consumption and the intention to engage in unprotected sex: Systematic review and meta-analysis of experimental studies. Addict. 2012;107(1):51–9.
Scott-Sheldon LA, Carey KB, Cunningham K, Johnson BT, Carey MP, MASH Research Team. Alcohol use predicts sexual decision-making: a systematic review and meta-analysis of the experimental literature. AIDS Behav. 2016;20(1):19–39.
George WH, Davis KC, Norris J, Heiman JR, Schacht RL, Stoner SA, Kajumulo KF. Alcohol and erectile response: the effects of high dosage in the context of demands to maximize sexual arousal. Exp Clin Psychopharmacol. 2006;14(4):461–70.
George WH, Davis KC, Heiman JR, et al. Women’s sexual arousal: Effects of high alcohol dosages and self-control instructions. Horm Behav. 2011;59(5):730–8.
MacDonald TK, Fong GT, Zanna MP, Martineau AM. Alcohol myopia and condom use: can alcohol intoxication be associated with more prudent behavior? J Pers Soc Psychol. 2000;78(4):605–19.
Cho YH, Span SA. The effect of alcohol on sexual risk-taking among young men and women. Addict Behav. 2010;35(8):779–85.
George WH, Davis KC, Masters NT, et al. Sexual victimization, alcohol intoxication, sexual-emotional responding, and sexual risk in heavy episodic drinking women. Arch Sex Behav. 2014;43(4):645–58.
Woolf-King SE, Maisto S, Carey M, Vanable P. Selection of film clips and development of a video for the investigation of sexual decision making among men who have sex with men. J Sex Res. 2010;47(6):589–97.
Gordon CM, Carey MP, Carey KB. Effects of a drinking event on behavioral skills and condom attitudes in men: implications for HIV risk from a controlled experiment. Health Psychol. 1997;16(5):490–5.
Maisto SA, Carey MP, Carey KB, Gordon CM, Schum JL. Effects of alcohol and expectancies on HIV-related risk perception and behavioral skills in heterosexual women. Exp Clin Psychopharmacol. 2004;12(4):288–97.
Davis KC, Jacques-Tiura AJ, Stappenbeck CA, et al. Men’s condom use resistance: alcohol effects on theory of planned behavior constructs. Health Psychol. 2016;35(2):178–86.
George WH, Davis KC, Masters NT, et al. Partner pressure, victimization history, and alcohol: women’s condom-decision abdication mediated by mood and anticipated negative partner reaction. AIDS Behav. 2016;20(1):134–46.
Masters NT, George WH, Davis KC, et al. Women’s unprotected sex intentions: roles of sexual victimization, intoxication, and partner perception. J Sex Res. 2014;51(5):586–98.
Fromme K, D’Amico EJ, Katz EC. Intoxicated sexual risk taking: an expectancy or cognitive impairment explanation? J Stud Alcohol. 1999;60(1):54–63.
Abbey A, Saenz C, Buck PO. The cumulative effects of acute alcohol consumption, individual differences and situational perceptions on sexual decision making. J Stud Alcohol. 2005;66(1):82–90.
Maisto SA, Carey MP, Carey KB, Gordon CM. The effects of alcohol and expectancies on risk perception and behavioral skills relevant to safer sex among heterosexual young adult women. J Stud Alcohol. 2002;63(4):476–85.
MacDonald TK, Zanna MP, Fong GT. Why common sense goes out the window: effects of alcohol on intentions to use condoms. Pers Soc Psychol Bull. 1996;22(8):763–75.
Murphy ST, Monahan JL, Miller LC. Inference under the influence: the impact of alcohol and inhibition conflict on women’s sexual decision making. Pers Soc Psychol Bull. 1998;24(5):517–28.
Ariely D, Loewenstein G. The heat of the moment: the effect of sexual arousal on sexual decision making. J Behav Decis Mak. 2006;19(2):87–98.
Imhoff R, Schmidt AF. Sexual disinhibition under sexual arousal: evidence for domain specificity in men and women. Arch Sex Behav. 2014;43(6):1123–36.
Davis KC, Hendershot CS, George WH, Norris J, Heiman JR. Alcohol’s effects on sexual decision making: an integration of alcohol myopia and individual differences. J Stud Alcohol Drugs. 2007;68(6):843–51.
George WH, Davis KC, Norris J, et al. Indirect effects of acute alcohol intoxication on sexual risk-taking: the roles of subjective and physiological sexual arousal. Arch Sex Behav. 2009;38(4):498–513.
Stoner SA, George WH, Peters LM, Norris J. Liquid courage: alcohol fosters risky sexual decision-making in individuals with sexual fears. AIDS Behav. 2007;11(2):227–37.
Stoner SA, Norris J, George WH, et al. Women’s condom use assertiveness and sexual risk-taking: effects of alcohol intoxication and adult victimization. Addict Behav. 2008;33(9):1167–76.
Schacht RL, Stoner SA, George WH, Norris J. Idiographically determined versus standard absorption periods in alcohol administration studies. Alcohol Clin Exp Res. 2010;34(5):925–7.
National Institute on Alcohol Abuse and Alcoholism. (NIAAA). Administering alcohol in human studies. http://www.niaaa.nih.gov/research/guidelines-and-resources/administering-alcohol-human-studies (2005). Accessed 3 Aug 2020.
Kajumulo KF, Davis KC, George WH. Experimental vignettes in assessing alcohol-involved risky sexual decision-making: evidence for external validity. Presentation presented at: annual meeting of the Society for the Scientific Study of Sexuality. Mexico: Puerto Vallarta; 2009.
Norris J, Kiekel PA, Purdie MP, Abdallah DA. Using experimental simulations to assess self-reported sexual behavior: further evidence of external validity. Presentation at a symposium on Alternative Conceptualizations of Assessing Sexual Behavior presented at: annual meeting of the Society for the Scientific Study of Sexuality. Nevada: Las Vegas; 2010.
Anderson CA, Lindsay JJ, Bushman BJ. Research in the psychological laboratory: truth or triviality? Curr Dir Psychol Sci. 1999;8(1):3–9.
Maisto SA, Carey MP, Carey KB, Gordon CM, Schum JL, Lynch KG. The relationship between alcohol and individual differences variables on attitudes and behavioral skills relevant to sexual health among heterosexual young adult men. Arch Sex Behav. 2004;33(6):571–84.
Zawacki T, Norris J, Hessler DM, et al. Effects of relationship motivation, partner familiarity, and alcohol on women’s risky sexual decision making. Pers Soc Psychol Bull. 2009;35(6):723–36.
Zawacki T. Effects of alcohol on women’s risky sexual decision making during social interactions in the laboratory. Psychol Women Q. 2011;35(1):107–18.
Steele CM, Josephs RA. Alcohol myopia: its prized and dangerous effects. Am Psychol. 1990;45(8):921–33.
Gilmore AK, George WH, Jacques-Tiura AJ, et al. Men’s intentions to have sex with a new partner: sexual and emotional responding, alcohol, and condoms. J Sex Marital Ther. 2016;42(2):165–77.
Davis KC, George WH, Norris J, et al. Effects of alcohol and blood alcohol concentration limb on sexual risk-taking intentions. J Stud Alcohol Drugs. 2009;70(4):499–507.
Norris J, Stoner SA, Hessler DM, et al. Influences of sexual sensation seeking, alcohol consumption, and sexual arousal on women’s behavioral intentions related to having unprotected sex. Psychol Addict Behav. 2009;23(1):14–22.
Prause N, Staley C, Finn P. The effects of acute ethanol consumption on sexual response and sexual risk-taking intent. Arch Sex Behav. 2011;40(2):373–84.
Wray TB, Simons JS, Maisto SA. Effects of alcohol intoxication and autonomic arousal on delay discounting and risky sex in young adult heterosexual men. Addict Behav. 2015;42:9–13.
Norris J, Stoner SA, Hessler DM, et al. Cognitive mediation of alcohol’s effects on women’s in-the-moment sexual decision making. Health Psychol. 2009;28(1):20–8.
Purdie MP, Norris J, Davis KC, et al. The effects of acute alcohol intoxication, partner risk level, and general intention to have unprotected sex on women’s sexual decision making with a new partner. Exp Clin Psychopharmacol. 2011;19(5):378–88.
Simons JS, Maisto SA, Wray TB, Emery NN. Acute effects of intoxication and arousal on approach/avoidance biases toward sexual risk stimuli in heterosexual men. Arch Sex Behav. 2016;45(1):43–51.
Stappenbeck CA, George WH, Staples JM, et al. In-the-moment dissociation, emotional numbing, and sexual risk: the influence of sexual trauma history, trauma symptoms, and alcohol intoxication. Psychol Violence. 2016;6(4):586–95.
Centers for Disease Control and Prevention (CDC). Complete Listing of Risk Reduction Evidence-based Behavioral Interventions. CDC. 2020a. https://www.cdc.gov/hiv/research/interventionresearch/compendium/rr/complete.html. Accessed 3 Aug 2020.
Freeman RC. Toward development of enhanced preventive interventions for HIV sexual risk among alcohol-using populations: confronting the ‘mere pause from thinking.’ AIDS Behav. 2016;20(1):1–8.
Walsh JL, Weinhardt LS, Kalichman SC, Carey MP. Using integrative data analysis to examine changes in alcohol use and changes in sexual risk behavior across four samples of STI clinic patients. Ann Behav Med. 2017;51(1):39–56.
Lewis MA, Rhew IC, Fairlie AM, Swanson A, Anderson J, Kaysen D. Evaluating personalized feedback intervention framing with a randomized controlled trial to reduce young adult alcohol-related sexual risk taking. Prev Sci. 2019;20(3):310–20.
Centers for Disease Control and Prevention. Pre-Exposure Prophylaxis. CDC. 2020b. https://www.cdc.gov/hiv/clinicians/prevention/prep.html. Accessed 3 Aug 2020.
Centers for Disease Control and Prevention. Preexposure prophylaxis for the prevention of HIV infection in the United States—2017 Update: a clinical practice guideline. CDC. 2018. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2017.pdf. Accessed 3 Aug 2020.
Auerbach JD, Kinsky S, Brown G, Charles V. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDS. 2015;29(2):102–10.
Biello KB, Bazzi AR, Mimiaga MJ, et al. Perspectives on HIV pre-exposure prophylaxis (PrEP) utilization and related intervention needs among people who inject drugs. Harm Reduct J. 2018;15(1):1–2.
Brooks RA, Landovitz RJ, Regan R, Lee SJ, Allen VC Jr. Perceptions of and intentions to adopt HIV pre-exposure prophylaxis among black men who have sex with men in Los Angeles. Int J STD AIDS. 2015;26(14):1040–8.
Pérez-Figueroa RE, Kapadia F, Barton SC, Eddy JA, Halkitis PN. Acceptability of PrEP uptake among racially/ethnically diverse young men who have sex with men: The P18 study. AIDS Educ Prev. 2015;27(2):112–25.
Wood BR, McMahan VM, Naismith K, Stockton JB, Delaney LA, Stekler JD. Knowledge, practices, and barriers to HIV preexposure prophylaxis prescribing among Washington State medical providers. Sex Transm Dis. 2018;45(7):452–8.
Gilmore HJ, Liu A, Koester KA, et al. Participant experiences and facilitators and barriers to pill use among men who have sex with men in the iPrEx pre-exposure prophylaxis trial in San Francisco. AIDS Patient Care STDS. 2013;27(10):560–6.
Haberer JE, Baeten JM, Campbell J, et al. Adherence to antiretroviral prophylaxis for HIV prevention: a substudy cohort within a clinical trial of serodiscordant couples in East Africa. PLoS Med. 2013;10(9):e1001511.
Psaros C, Haberer JE, Katabira E, et al. An intervention to support HIV pre-exposure prophylaxis (PrEP) adherence in HIV serodiscordant couples in Uganda. J Acquir Immune Defic Syndr (1999). 2014;66(5):522–9.
Tangmunkongvorakul A, Chariyalertsak S, Amico KR, et al. Facilitators and barriers to medication adherence in an HIV prevention study among men who have sex with men in the iPrEx study in Chiang Mai, Thailand. AIDS Care. 2013;25(8):961–7.
Centers for Disease Control and Prevention. Updated guidelines for antiretroviral postexposure prophylaxis after sexual, injection drug use, or other nonoccupational exposure to HIV—United States, 2016. Ann Emerg Med. 2016;68(3):335–8.
Chacko L, Ford N, Sbaiti M, Siddiqui R. Adherence to HIV post-exposure prophylaxis in victims of sexual assault: a systematic review and meta-analysis. Sex Transm Infect. 2012;88(5):335–41.
Ford N, Irvine C, Shubber Z, et al. Adherence to HIV postexposure prophylaxis: a systematic review and meta-analysis. AIDS. 2014;28(18):2721–7.
Desrosiers A, Levy M, Dright A, et al. A randomized controlled pilot study of a culturally-tailored counseling intervention to increase uptake of HIV pre-exposure prophylaxis among young Black men who have sex with men in Washington. DC AIDS Behav. 2019;23(1):105–15.
Mayer KH, Safren SA, Elsesser SA, et al. Optimizing pre-exposure antiretroviral prophylaxis adherence in men who have sex with men: results of a pilot randomized controlled trial of “Life-Steps for PrEP.” AIDS Behav. 2017;21(5):1350–60.
Moitra E, van den Berg JJ, Sowemimo-Coker G, Chau S, Nunn A, Chan PA. Open pilot trial of a brief motivational interviewing-based HIV pre-exposure prophylaxis intervention for men who have sex with men: preliminary effects, and evidence of feasibility and acceptability. AIDS Care. 2019;32(3):406–10.
Getty CA, Subramaniam S, Holtyn AF, Jarvis BP, Rodewald A, Silverman K. Evaluation of a computer-based training program to teach adults at risk for HIV about pre-exposure prophylaxis. AIDS Educ Prev. 2018;30(4):287–300.
Shrestha R, Altice FL, Karki P, Copenhaver MM. Integrated bio-behavioral approach to improve adherence to pre-exposure prophylaxis and reduce HIV risk in people who use drugs: a pilot feasibility study. AIDS Behav. 2018;22(8):2640–9.
Centers for Disease Control and Prevention. Approach to public health – High-impact Prevention. CDC. 2019b. https://www.cdc.gov/nchhstp/highimpactprevention/index.html. Accessed 3 Aug 2020.
Young I, McDaid L. How acceptable are antiretrovirals for the prevention of sexually transmitted HIV? A review of research on the acceptability of oral pre-exposure prophylaxis and treatment as prevention. AIDS Behav. 2014;18(2):195–216.
Collier KL, Colarossi LG, Sanders K. Raising awareness of pre-exposure prophylaxis (PrEP) among women in New York City: community and provider perspectives. J Health Commun. 2017;22(3):183–9.
Centers for Disease Control and Prevention. HIV by group: Gender – women. CDC. 2020c. https://www.cdc.gov/hiv/group/gender/women/index.html. Accessed 3 Aug 2020.
Lyon AR, Koerner K. User-centered design for psychosocial intervention development and implementation. Clin Psychol. 2016;23(2):180–200.
Centers for Disease Control and Prevention. Prevent—Pre-Exposure Prophylaxis (PrEP). CDC. 2020d. https://www.cdc.gov/hiv/effective-interventions/prevent/prep/index.html. Accessed 3 Aug 2020
Kalichman SC, Eaton L. Alcohol-antiretroviral interactive toxicity beliefs as a potential barrier to HIV pre-exposure prophylaxis among men who have sex with men. J Int AIDS Soc. 2017;20(1):21534.
Noar SM, Pierce LB, Black HG. Can computer-mediated interventions change theoretical mediators of safer sex? A meta-analysis. Hum Commun Res. 2010;36(3):261–97.
Noar SM. Computer technology-based interventions in HIV prevention: state of the evidence and future directions for research. AIDS Care. 2011;23(5):525–33.
Ingersoll KS, Dillingham RA, Hettema JE, et al. Pilot RCT of bidirectional text messaging for ART adherence among nonurban substance users with HIV. Health Psychol. 2015;34(S):1305–15.
Pop-Eleches C, Thirumurthy H, Habyarimana JP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS (London, England). 2011;25(6):825–34.
Rana AI, van den Berg JJ, Lamy E, Beckwith CG. Using a mobile health intervention to support HIV treatment adherence and retention among patients at risk for disengaging with care. AIDS Patient Care STDS. 2016;30(4):178–84.
Fuchs JD, Stojanovski K, Vittinghoff E, et al. A mobile health strategy to support adherence to antiretroviral preexposure prophylaxis. AIDS Patient Care STDS. 2018;32(3):104–11.
Hendershot CS, Stoner SA, George WH, Norris J. Alcohol use, expectancies, and sexual sensation seeking as correlates of HIV risk behavior in heterosexual young adults. Psychol Addict Behav. 2007;21(3):365–72.
Fromme K, Stroot EA, Kaplan D. Comprehensive effects of alcohol: development and psychometric assessment of a new expectancy questionnaire. Psychol Assess. 1993;5(1):19–26.
George WH, Dermen KH, Nochajski TH. Expectancy set, self-reported expectancies and predispositional traits: predicting interest in violence and erotica. J Stud Alcohol. 1989;50(6):541–51.
George WH, Frone MR, Cooper ML, Russell M, Skinner JB, Windle M. A revised Alcohol Expectancy Questionnaire: factor structure confirmation, and invariance in a general population sample. J Stud Alcohol. 1995;56(2):177–85.
Leigh BC, Stacy AW. Alcohol outcome expectancies: scale construction and predictive utility in higher order confirmatory models. Psychol Assess. 1993;5(2):216–29.
Abbey A, McAuslan P, Ross LT, Zawacki T. Alcohol expectancies regarding sex, aggression, and sexual vulnerability: reliability and validity assessment. Psychol Addict Behav. 1999;13(3):174–82.
Dermen KH, Cooper ML. Sex-related alcohol expectancies among adolescents: I. Scale development. Psychol Addict Behav. 1994;8(3):152–60.
Leigh BC. “Venus gets in my thinking”: Drinking and female sexuality in the age of AIDS. J Subst Abuse. 1990;2(2):129–45.
Darkes J, Goldman MS. Expectancy challenge and drinking reduction: experimental evidence for a mediational process. J Consult Clin Psychol. 1993;61(2):344–53.
Labbe AK, Maisto SA. Alcohol expectancy challenges for college students: a narrative review. Clin Psychol Rev. 2011;31(4):673–83.
Scott-Sheldon LA, Terry DL, Carey KB, Garey L, Carey MP. Efficacy of expectancy challenge interventions to reduce college student drinking: a meta-analytic review. Psychol Addict Behav. 2012;26(3):393–405.
Steele CM, Southwick L. Alcohol and social behavior: I. The psychology of drunken excess. J Pers Soc Psychol. 1985;48(1):18–34.
MacDonald TK, MacDonald G, Zanna MP, Fong G. Alcohol, sexual arousal, and intentions to use condoms in young men: applying alcohol myopia theory to risky sexual behavior. Health Psychol. 2000;19(3):290–8.
Morrison DM, Gillmore MR, Hoppe MJ, Gaylord J, Leigh BC, Rainey D. Adolescent drinking and sex: findings from a daily diary study. Perspect Sex Reprod Health. 2003;35(4):162–8.
Dal Cin S, MacDonald TK, Fong GT, Zanna MP, Elton-Marshall TE. Remembering the message: the use of a reminder cue to increase condom use following a safer sex intervention. Health Psychol. 2006;25(3):438–43.
Norris J, Masters NT, Zawacki T. Cognitive mediation of women’s sexual decision making: the influence of alcohol, contextual factors, and background variables. Annu Rev Sex Res. 2004;15(1):258–96.
Davis KC, Norris J, Hessler DM, Zawacki T, Morrison DM, George WH. College women’s sexual decision making: cognitive mediation of alcohol expectancy effects. J Am Coll Health. 2010;58(5):481–9.
Danube CL, Norris J, Stappenbeck CA, et al. Partner type, sexual double standard endorsement, and ambivalence predict abdication and unprotected sex intentions in a community sample of young women. J Sex Res. 2016;53(4–5):601–13.
Bryan AE, Norris J, Abdallah DA, et al. Condom-insistence conflict in Women’s alcohol-involved sexual encounters with a new male partner. Psychol Women Q. 2017;41(1):100–13.
Scott-Sheldon LA, Johnson BT. Eroticizing creates safer sex: a research synthesis. J Prim Prev. 2006;27(6):619–40.
Staras SA, Cook RL, Clark DB. Sexual partner characteristics and sexually transmitted diseases among adolescents and young adults. Sex Transm Dis. 2009;36(4):232–8.
Seth P, Raiji PT, DiClemente RJ, Wingood GM, Rose E. Psychological distress as a correlate of a biologically confirmed STI, risky sexual practices, self-efficacy and communication with male sex partners in African-American female adolescents. Psychol Health Med. 2009;14(3):291–300.
Harvey SM, Bird ST. What makes women feel powerful? An exploratory study of relationship power and sexual decision-making with African Americans at risk for HIV/STDs. Women Health. 2004;39(3):1–8.
Adimora AA, Schoenbach VJ, Taylor EM, Khan MR, Schwartz RJ. Concurrent partnerships, nonmonogamous partners, and substance use among women in the United States. Am J Public Health Res. 2011;101(1):128–36.
Davis KC, Stappenbeck CA, Norris J, et al. Young men’s condom use resistance tactics: a latent profile analysis. J Sex Res. 2014;51(4):454–65.
Wegner R, Lewis MA, Davis KC, Neilson EC, Norris J. Tactics young women use to resist condom use when a partner wants to use a condom. J Sex Res. 2018;55(7):817–23.
Davis KC, Stappenbeck CA, Masters NT, George WH. Young women’s experiences with coercive and noncoercive condom use resistance: examination of an understudied sexual risk behavior. Womens Health Issues. 2019;29(3):231–7.
Neilson EC, Eakins DR, Cue Davis K, Norris J, George WH. Depressive symptoms, acute alcohol intoxication, and risk rationale effects on men’s condom use resistance. J Sex Res. 2017;54(6):764–75.
Wegner R, Davis KC, Stappenbeck CA, Kajumulo KF, Norris J, George WH. The effects of men’s hostility toward women, acute alcohol intoxication, and women’s condom request style on men’s condom use resistance tactics. Psychol Violence. 2017;7(4):593–601.
Davis KC, Schraufnagel TJ, Jacques-Tiura AJ, Norris J, George WH, Kiekel PA. Childhood sexual abuse and acute alcohol effects on men’s sexual aggression intentions. Psychol Violence. 2012;2(2):179–93.
Davis KC, Danube CL, et al. Distal and proximal influences on men’s intentions to resist condoms: alcohol, sexual aggression history, impulsivity, and social-cognitive factors. AIDS Behav. 2016;20(1):147–57.
Davis KC. The influence of alcohol expectancies and intoxication on men’s aggressive unprotected sexual intentions. Exp Clin Psychopharmacol. 2010;18(5):418–28.
Davis KC, Kirwan M, Wegner R, Neilson EC, Stappenbeck CA. Effects of alcohol, condom request style, and state anger on men’s condom use resistance. J Stud Alcohol Drugs. 2020;81(4):454–61.
Brooks RA, Landrian A, Nieto O, Fehrenbacher A. Experiences of anticipated and enacted pre-exposure prophylaxis (PrEP) stigma among Latino MSM in Los Angeles. AIDS Behav. 2019;23(7):1964–73.
Mustanski B, Ryan DT, Hayford C, Phillips G, Newcomb ME, Smith JD. Geographic and individual associations with PrEP stigma: results from the RADAR cohort of diverse young men who have sex with men and transgender women. AIDS Behav. 2018;22(9):3044–56.
Dubov A, Galbo P Jr, Altice FL, Fraenkel L. Stigma and shame experiences by MSM who take PrEP for HIV prevention: a qualitative study. Am J Mens Health. 2018;12(6):1843–54.
Lelutiu-Weinberger C, Golub SA. Enhancing PrEP access for Black and Latino men who have sex with men. J Acquir Immune Defic Syndr (1999). 2016;73(5):547–55.
Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull. 2009;135(5):707–30.
Nielsen L, Riddle M, King JW, et al. The NIH Science of Behavior Change Program: transforming the science through a focus on mechanisms of change. Behav Res Ther. 2018;101:3–11.
Edmondson D, Falzon L, Sundquist KJ, et al. A systematic review of the inclusion of mechanisms of action in NIH-funded intervention trials to improve medication adherence. Behav Res Ther. 2018;101:12–9.
Babcock JC, Graham K, Canady B, Ross JM. A proximal change experiment testing two communication exercises with intimate partner violent men. Behav Ther. 2011;42(2):336–47.
Gottman J, Ryan K, Swanson C, Swanson K. Proximal change experiments with couples: a methodology for empirically building a science of effective interventions for changing couples’ interaction. J Fam Comm. 2005;5(3):163–90.
Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. J Child Psychol Psychiatry. 2003;44(8):1116–29.
Davis KC, Neilson EC, Kirwan ME, Eldridge N, George WH, Stappenbeck CA. Alcohol-involved sexual aggression: emotion regulation as a mechanism of behavior change. Health Psychol. 2020. https://doi.org/10.1037/hea0001048.
Andrasik MP, Otto JM, Nguyen HV, et al. The potential of alcohol “heat-of-the-moment” scenarios in HIV prevention: a qualitative study exploring intervention implications. Arch Sex Behav. 2013;42(8):1487–99.
Lindgren KP, Neighbors C, Blayney JA, Mullins PM, Kaysen D. Do drinking motives mediate the association between sexual assault and problem drinking? Addict Behav. 2012;37(3):323–6.
Davis KC, Neilson EC, Wegner R, Danube CL. The intersection of men’s sexual violence perpetration and sexual risk behavior: a literature review. Aggress Violent Behav. 2018;40:83–90.
Gordon CM, Carey MP. Alcohol’s effects on requisites for sexual risk reduction in men: an initial experimental investigation. Health Psychol. 1996;15(1):56–60.
Funding
Manuscript preparation was partially supported by the National Institute of Alcohol Abuse and Alcoholism: K99AA028777 (PI: Blayney); 2R37AA025212 (PI: Davis); R01AA016281 (PIs: George, Davis); K08AA021745 (PI: Stappenbeck).
Author information
Authors and Affiliations
Contributions
All authors contributed to all aspects of manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
George, W.H., Blayney, J.A., Stappenbeck, C.A. et al. The Role of Alcohol-Related Behavioral Risk in the Design of HIV Prevention Interventions in the Era of Antiretrovirals: Alcohol Challenge Studies and Research Agenda. AIDS Behav 25 (Suppl 3), 347–364 (2021). https://doi.org/10.1007/s10461-021-03351-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03351-4