Abstract
Patients with advanced heart failure are implanted with a left ventricular assist device (LVAD) as a bridge-to-transplantation or destination therapy. Despite advances in pump design, the risk of stroke remains high. LVAD implantation significantly alters intraventricular hemodynamics, where regions of stagnation or elevated shear stresses promote thrombus formation. Third generation pumps incorporate a pulsatility mode that modulates rotational speed of the pump to enhance in-pump washout. We investigated how the timing of the pulsatility mode with the cardiac cycle affects intraventricular hemodynamic factors linked to thrombus formation. Computational fluid dynamics simulations with Lagrangian particle tracking to model platelet behavior in a patient-specific left ventricle captured altered intraventricular hemodynamics due to LVAD implantation. HeartMate 3 incorporates a pulsatility mode that modulates the speed of the pump every two seconds. Four different timings of this pulsatility mode with respect to the cardiac cycle were investigated. A strong jet formed between the mitral valve and inflow cannula. Blood stagnated in the left ventricular outflow tract beneath a closed aortic valve, in the near-wall regions off-axis of the jet, and in a large counterrotating vortex near the anterior wall. Computational results showed good agreement with particle image velocimetry results. Synchronization of the pulsatility mode with peak systole decreased stasis, reflected in the intraventricular washout of virtual contrast and Lagrangian particles over time. Temporal synchronization of HeartMate 3 pulsatility with the cardiac cycle reduces intraventricular stasis and could be beneficial for decreasing thrombogenicity.








Similar content being viewed by others
References
Tsao, C. W., A. W. Aday, Z. I. Almarzooq, A. Alonso, A. Z. Beaton, M. S. Bittencourt, A. K. Boehme, A. E. Buxton, A. P. Carson, Y. Commodore-Mensah, M. S. V. Elkind, K. R. Evenson, C. Eze-Nliam, J. F. Ferguson, G. Generoso, J. E. Ho, R. Kalani, S. S. Khan, B. M. Kissela, K. L. Knutson, D. A. Levine, T. T. Lewis, J. Liu, M. S. Loop, J. Ma, M. E. Mussolino, S. D. Navaneethan, A. M. Perak, R. Poudel, M. Rezk-Hanna, G. A. Roth, E. B. Schroeder, S. H. Shah, E. L. Thacker, L. B. VanWagner, S. S. Virani, J. H. Voecks, N.-Y. Wang, K. Yaffe, and S. S. Martin. Heart disease and stroke statistics-2022 update: A report from the American Heart Association. Circulation. 2022. https://doi.org/10.1161/CIR.0000000000001052.
Mancini, D., and P. C. Colombo. Left ventricular assist devices: A rapidly evolving alternative to transplant. J. Am. Coll. Cardiol. 65:2542–2555, 2015. https://doi.org/10.1016/j.jacc.2015.04.039.
McDonagh, T. A., M. Metra, M. Adamo, R. S. Gardner, A. Baumbach, M. Böhm, H. Burri, J. Butler, J. Čelutkienė, O. Chioncel, J. G. F. Cleland, A. J. S. Coats, M. G. Crespo-Leiro, D. Farmakis, M. Gilard, S. Heymans, A. W. Hoes, T. Jaarsma, E. A. Jankowska, M. Lainscak, C. S. P. Lam, A. R. Lyon, J. J. V. McMurray, A. Mebazaa, R. Mindham, C. Muneretto, M. F. Piepoli, S. Price, G. M. C. Rosano, F. Ruschitzka, A. K. Skibelund, R. A. Boer, P. C. Schulze, M. Abdelhamid, V. Aboyans, S. Adamopoulos, S. D. Anker, E. Arbelo, R. Asteggiano, J. Bauersachs, A. Bayes-Genis, M. A. Borger, W. Budts, M. Cikes, K. Damman, V. Delgado, P. Dendale, P. Dilaveris, H. Drexel, J. Ezekowitz, V. Falk, L. Fauchier, G. Filippatos, A. Fraser, N. Frey, C. P. Gale, F. Gustafsson, J. Harris, B. Iung, S. Janssens, M. Jessup, A. Konradi, D. Kotecha, E. Lambrinou, P. Lancellotti, U. Landmesser, C. Leclercq, B. S. Lewis, F. Leyva, A. Linhart, M. L. Løchen, L. H. Lund, D. Mancini, J. Masip, D. Milicic, C. Mueller, H. Nef, J. C. Nielsen, L. Neubeck, M. Noutsias, S. E. Petersen, A. S. Petronio, P. Ponikowski, E. Prescott, A. Rakisheva, D. J. Richter, E. Schlyakhto, P. Seferovic, M. Senni, M. Sitges, M. Sousa-Uva, C. G. Tocchetti, R. M. Touyz, C. Tschoepe, and J. Waltenberger. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur. J. Heart Fail. 24:4–131, 2022. https://doi.org/10.1002/EJHF.2333.
Yancy, C. W., M. Jessup, B. Bozkurt, J. Butler, D. E. Casey, M. H. Drazner, G. C. Fonarow, S. A. Geraci, T. Horwich, J. L. Januzzi, M. R. Johnson, E. K. Kasper, W. C. Levy, F. A. Masoudi, P. E. McBride, J. J. V. McMurray, J. E. Mitchell, P. N. Peterson, B. Riegel, F. Sam, L. W. Stevenson, W. H. W. Tang, E. J. Tsai, and B. L. Wilkoff. 2013 ACCF/AHA guideline for the management of heart failure: Executive summary. Circulation. 128:1810–1852, 2013. https://doi.org/10.1161/CIR.0B013E31829E8807.
Kormos, R. L., J. Cowger, F. Pagani, J. J. Teuteberg, D. J. Goldstein, J. P. Jacobs, R. S. Higgins, L. W. Stevenson, J. Stehlik, P. Atluri, K. L. Grady, and J. K. Kirklin. The Society of Thoracic Surgeons Intermacs database annual report: Evolving indications, outcomes, and scientific partnerships. J. Heart Lung Transplant. 38:114–126, 2019. https://doi.org/10.1016/j.healun.2018.11.013.
Adesiyun, T. A., R. C. McLean, R. J. Tedford, G. J. R. Whitman, C. M. Sciortino, J. V. Conte, A. S. Shah, and S. D. Russell. Long-term follow-up of continuous flow left ventricular assist devices: Complications and predisposing risk factors. Int. J. Artif. Organs. 40:622–628, 2017. https://doi.org/10.5301/IJAO.5000628.
Li, S., J. A. Beckman, R. Cheng, C. Ibeh, C. J. Creutzfeldt, J. Bjelkengren, J. Herrington, A. Stempien-Otero, S. Lin, W. C. Levy, D. Fishbein, K. J. Koomalsingh, D. Zimpfer, M. S. Slaughter, A. Aliseda, D. Tirschwell, and C. Mahr. Comparison of neurologic event rates among HeartMate II, HeartMate 3, and HVAD. ASAIO J. 66:620–624, 2020. https://doi.org/10.1097/MAT.0000000000001084.
Mehra, M. R., G. C. Stewart, and P. A. Uber. The vexing problem of thrombosis in long-term mechanical circulatory support. J. Heart Lung Transplant. 33:1–11, 2014. https://doi.org/10.1016/J.HEALUN.2013.12.002.
Petrucci, R. J., J. G. Rogers, L. Blue, C. Gallagher, S. D. Russell, D. Dordunoo, B. E. Jaski, S. Chillcott, B. Sun, T. L. Yanssens, A. Tatooles, L. Koundakjian, D. J. Farrar, and M. S. Slaughter. Neurocognitive function in destination therapy patients receiving continuous-flow vs pulsatile-flow left ventricular assist device support. J. Heart Lung Transplant. 31:27–36, 2012. https://doi.org/10.1016/J.HEALUN.2011.10.012.
Netuka, I., and M. R. Mehra. Ischemic stroke and subsequent thrombosis within a HeartMate 3 left ventricular assist system: A cautionary tale. J. Heart Lung Transplant. 37:170–172, 2018. https://doi.org/10.1016/j.healun.2017.11.002.
Barac, Y. D., A. Nevo, J. N. Schroder, C. A. Milano, and M. A. Daneshmand. LVAD outflow graft role in pump thrombosis. ASAIO J. 66:128–131, 2020. https://doi.org/10.1097/MAT.0000000000000936.
Estep, J. D., R. F. Stainback, S. H. Little, G. Torre, and W. A. Zoghbi. The role of echocardiography and other imaging modalities in patients with left ventricular assist devices. JACC Cardiovasc. Imaging. 3:1049–1064, 2010. https://doi.org/10.1016/j.jcmg.2010.07.012.
Glass, C. H., A. Christakis, G. A. Fishbein, J. C. Watkins, K. C. Strickland, R. N. Mitchell, and R. F. Padera. Thrombus on the inflow cannula of the HeartWare HVAD: an update. Cardiovasc. Pathol. 38:14–20, 2019. https://doi.org/10.1016/j.carpath.2018.09.002.
Slaughter, M. S., F. D. Pagani, J. G. Rogers, L. W. Miller, B. Sun, S. D. Russell, R. C. Starling, L. Chen, A. J. Boyle, S. Chillcott, R. M. Adamson, M. S. Blood, M. T. Camacho, K. A. Idrissi, M. Petty, M. Sobieski, S. Wright, T. J. Myers, and D. J. Farrar. Clinical management of continuous-flow left ventricular assist devices in advanced heart failure. J. Heart Lung Transplant. 29:1–39, 2010. https://doi.org/10.1016/j.healun.2010.01.011.
May-Newman, K., Y. K. Wong, R. Adamson, P. Hoagland, V. Vu, and W. Dembitsky. Thromboembolism is linked to intraventricular flow stasis in a patient supported with a left ventricle assist device. ASAIO J. 59:452–455, 2013. https://doi.org/10.1097/MAT.0B013E318299FCED.
Fried, J., A. R. Garan, S. Shames, A. Masoumi, M. Yuzefpolskaya, K. Takeda, H. Takayama, N. Uriel, Y. Naka, P. C. Colombo, and V. K. Topkara. Aortic root thrombosis in patients supported with continuous-flow left ventricular assist devices. J. Heart Lung Transplant. 37:1425–1432, 2018. https://doi.org/10.1016/J.HEALUN.2018.07.012.
Carey, M. R., D. Marshall, K. Clerkin, R. Laracuente, J. Sanchez, S. S. Jain, J. K. Raikhelkar, J. S. Leb, Y. Kaku, M. Yuzefpolskaya, Y. Naka, P. C. Colombo, G. T. Sayer, K. Takeda, N. Uriel, V. K. Topkara, and J. A. Fried. Aortic root thrombosis in patients with HeartMate 3 left ventricular assist device support. J. Heart Lung Transplant. 2023. https://doi.org/10.1016/J.HEALUN.2023.08.023.
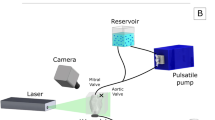
Chassagne, F., M. Miramontes, V. K. Chivukula, S. Li, J. A. Beckman, C. Mahr, and A. Aliseda. In vitro investigation of the effect of left ventricular assist device speed and pulsatility mode on intraventricular hemodynamics. Ann. Biomed. Eng. 49:1318–1332, 2021. https://doi.org/10.1007/S10439-020-02669-9.
Rossini, L., O. O. Braun, M. Brambatti, Y. Benito, A. Mizeracki, M. Miramontes, C. Nguyen, P. Martinez-Legazpi, S. Almeida, M. Kraushaar, V. Vu, K. May-Newman, J. Bermejo, E. D. Adler, A. M. Kahn, and J. C. D. Alamo. Intraventricular flow patterns in patients treated with left ventricular assist devices. ASAIO J. 67:74–83, 2021. https://doi.org/10.1097/MAT.0000000000001158.
Ortiz, S., V. Vu, R. Montes, and K. May-Newman. Left ventricular flow dynamics with the HeartMate 3 left ventricular assist device: Effect of inflow cannula position and speed modulation. ASAIO J. 67:1301–1311, 2021. https://doi.org/10.1097/MAT.0000000000001523.
Wong, K., G. Samaroo, I. Ling, W. Dembitsky, R. Adamson, J. C. Álamo, and K. May-Newman. Intraventricular flow patterns and stasis in the LVAD-assisted heart. J. Biomech. 47:1485–1494, 2014. https://doi.org/10.1016/j.jbiomech.2013.12.031.
Viola, F., E. Jermyn, J. Warnock, G. Querzoli, and R. Verzicco. Left ventricular hemodynamics with an implanted assist device: An in vitro fluid dynamics study. Ann. Biomed. Eng. 47:1799–1814, 2019. https://doi.org/10.1007/S10439-019-02273-6.
Aigner, P., M. Schweiger, K. Fraser, Y. Choi, F. Lemme, N. Cesarovic, U. Kertzscher, H. Schima, M. Hübler, and M. Granegger. Ventricular flow field visualization during mechanical circulatory support in the assisted isolated beating heart. Ann. Biomed. Eng. 48:794–804, 2020. https://doi.org/10.1007/s10439-019-02406-x.
Da Rocha E Silva, J., A. L. Meyer, S. Eifert, J. Garbade, F. W. Mohr, and M. Strueber. Influence of aortic valve opening in patients with aortic insufficiency after left ventricular assist device implantation. Eur. J. Cardiothorac. Surg. 49:784–787, 2016. https://doi.org/10.1093/EJCTS/EZV204.
John, R., K. Mantz, P. Eckman, A. Rose, and K. May-Newman. Aortic valve pathophysiology during left ventricular assist device support. J. Heart Lung Transplant. 29:1321–1329, 2010. https://doi.org/10.1016/J.HEALUN.2010.06.006.
Clifford, R., D. Robson, C. Gross, F. Moscato, H. Schima, P. Jansz, P. S. Macdonald, and C. S. Hayward. Beat-to-beat detection of aortic valve opening in HeartWare left ventricular assist device patients. Artif. Organs. 43:458–466, 2019. https://doi.org/10.1111/AOR.13381.
Lowe, G. D. O. Virchow’s triad revisited: Abnormal flow. Pathophysiol. Haemost. Thromb. 33:455–457, 2003. https://doi.org/10.1159/000083845.
Shear induced aggregation and lysis of platelets. S.P. Hung, R.M.J.J.H.S. T.C.; Hochmith. Transactions - American Society for Artificial Internal Organs. 22:285–290, 1976.
Ramstack, J. M., L. Zuckerman, and L. F. Mockros. Shear-induced activation of platelets. J. Biomech. 12:113–125, 1979. https://doi.org/10.1016/0021-9290(79)90150-7.
Shankaran, H., P. Alexandridis, and S. Neelamegham. Aspects of hydrodynamic shear regulating shear-induced platelet activation and self-association of von Willebrand factor in suspension. Blood. 101:2637–2645, 2003. https://doi.org/10.1182/BLOOD-2002-05-1550.
Chiu, W. C., Y. Alemu, A. J. Mclarty, S. Einav, M. J. Slepian, and D. Bluestein. Ventricular assist device implantation configurations impact overall mechanical circulatory support system thrombogenic potential. ASAIO J. 63:285, 2017. https://doi.org/10.1097/MAT.0000000000000488.
Girdhar, G., M. Xenos, Y. Alemu, W.-C. Chiu, and B. E. Lynch. Device thrombogenicity emulation: A novel method for optimizing mechanical circulatory support device thromboresistance. PLoS ONE. 7:32463, 2012. https://doi.org/10.1371/journal.pone.0032463.
Chivukula, V. K., J. A. Beckman, A. R. Prisco, T. Dardas, S. Lin, J. W. Smith, N. A. Mokadam, A. Aliseda, and C. Mahr. Left ventricular assist device inflow cannula angle and thrombosis risk. Circ. Heart Fail. 2018. https://doi.org/10.1161/CIRCHEARTFAILURE.117.004325.
Chivukula, V. K., J. A. Beckman, S. Li, S. C. Masri, W. C. Levy, S. Lin, R. K. Cheng, S. D. Farris, G. Wood, T. F. Dardas, J. N. Kirkpatrick, K. Koomalsingh, D. Zimpfer, G. B. MacKensen, F. Chassagne, C. Mahr, and A. Aliseda. Left ventricular assist device inflow cannula insertion depth influences thrombosis risk. ASAIO J. 2020. https://doi.org/10.1097/MAT.0000000000001068.
Aliseda, A., V. K. Chivukula, P. McGah, A. R. Prisco, J. A. Beckman, G. J. M. Garcia, N. A. Mokadam, and C. Mahr. LVAD outflow graft angle and thrombosis risk. ASAIO J. 63:14, 2017. https://doi.org/10.1097/MAT.0000000000000443.
Bourque, K., C. Cotter, C. Dague, D. Harjes, O. Dur, J. Duhamel, K. Spink, K. Walsh, and E. Burke. Design rationale and preclinical evaluation of the HeartMate 3 left ventricular assist system for hemocompatibility. ASAIO J. 62:375–383, 2016. https://doi.org/10.1097/MAT.0000000000000388.
Larose, J. A., D. Tamez, M. Ashenuga, and C. Reyes. Design concepts and principle of operation of the HeartWare ventricular assist system. ASAIO J. 56:285–289, 2010. https://doi.org/10.1097/MAT.0B013E3181DFBAB5.
Liao, S., E. L. Wu, M. Neidlin, Z. Li, B. Simpson, and S. D. Gregory. The influence of rotary blood pump speed modulation on the risk of intraventricular thrombosis. Artif. Organs. 42:943–953, 2018. https://doi.org/10.1111/AOR.13330.
Khienwad, T., A. Maurer, M. Ghodrati, T. Schlöglhofer, F. Moscato, M. Stoiber, H. Schima, and P. Aigner. Effect of timings of the Lavare cycle on the ventricular washout in an in vitro flow visualization setup. ASAIO J. 67:517–528, 2021. https://doi.org/10.1097/MAT.0000000000001269.
Chassagne, F., J. A. Beckman, S. Li, C. Mahr, and A. Aliseda. In vitro investigation of the effect of the timing of left ventricular assist device speed modulation on intraventricular flow patterns. ASAIO J. 69:533–543, 2023. https://doi.org/10.1097/MAT.0000000000001893.
Mccormick, M., D. Nordsletten, P. Lamata, and N. P. Smith. Computational analysis of the importance of flow synchrony for cardiac ventricular assist devices. Comput. Biol. Med. 49:83–94, 2014. https://doi.org/10.1016/j.compbiomed.2014.03.013.
Boraschi, A., S. Bozzi, B. Thamsen, M. Granegger, L. Wiegmann, F. Pappalardo, M. J. Slepian, V. Kurtcuoglu, A. Redaelli, D. D. Zélicourt, and F. Consolo. Thrombotic risk of rotor speed modulation regimes of contemporary centrifugal continuous-flow left ventricular assist devices. ASAIO J. 67:737–745, 2021. https://doi.org/10.1097/MAT.0000000000001297.
Fang, P., J. Du, A. Boraschi, S. Bozzi, A. Redaelli, M. S. Daners, V. Kurtcuoglu, F. Consolo, and D. Zélicourt. Insights into the low rate of in-pump thrombosis with the HeartMate 3: Does the artificial pulse improve washout? Frontiers in Cardiovascular Medicine.9:775780, 2022. https://doi.org/10.3389/FCVM.2022.775780.
Wiegmann, L., B. Thamsen, D. Zélicourt, M. Granegger, S. Boës, M. S. Daners, M. Meboldt, and V. Kurtcuoglu. Fluid dynamics in the HeartMate 3: Influence of the artificial pulse feature and residual cardiac pulsation. Artif. Organs. 43:363–376, 2019. https://doi.org/10.1111/aor.13346.
Zimpfer, D., M. Strueber, P. Aigner, J. D. Schmitto, A. E. Fiane, R. Larbalestier, S. Tsui, P. Jansz, A. Simon, S. Schueler, F. Moscato, and H. Schima. Evaluation of the HeartWare ventricular assist device Lavare cycle in a particle image velocimetry model and in clinical practice. Eur. J. Cardiothorac. Surg. 50:839–848, 2016. https://doi.org/10.1093/ejcts/ezw232.
Colombo, P. C., M. R. Mehra, D. J. Goldstein, J. D. Estep, C. Salerno, U. P. Jorde, J. A. Cowger, J. C. Cleveland, N. Uriel, G. Sayer, E. R. Skipper, F. X. Downey, M. Ono, R. Hooker, A. C. Anyanwu, M. M. Givertz, C. Mahr, I. Topuria, S. I. Somo, D. L. Crandall, and D. A. Horstmanshof. Comprehensive analysis of stroke in the long-term cohort of the MOMENTUM 3 study. Circulation. 139:155–168, 2019. https://doi.org/10.1161/CIRCULATIONAHA.118.037231.
Mueller, M., C. Hoermandinger, G. Richter, J. Mulzer, D. Tsyganenko, T. Krabatsch, C. Starck, J. Stein, F. Schoenrath, V. Falk, and E. Potapov. Retrospective 1-year outcome follow-up in 200 patients supported with HeartMate 3 and HeartWare left ventricular assist devices in a single centre. Eur. J. Cardiothorac. Surg. 57:1160–1165, 2020. https://doi.org/10.1093/ejcts/ezaa017.
Sorensen, E. N., L. M. Dees, D. J. Kaczorowski, and E. D. Feller. The HeartWare Lavare cycle: A cautionary tale. ASAIO J. 66:114–116, 2020. https://doi.org/10.1097/MAT.0000000000001161.
Ghodrati, M., T. Khienwad, A. Maurer, F. Moscato, F. Zonta, H. Schima, and P. Aigner. Validation of numerically simulated ventricular flow patterns during left ventricular assist device support. Int. J. Artif. Organs. 44:30–38, 2021. https://doi.org/10.1177/0391398820904056.
Rayz, V. L., L. Boussel, L. Ge, J. R. Leach, A. J. Martin, M. T. Lawton, C. Mcculloch, and D. Saloner. Flow residence time and regions of intraluminal thrombus deposition in intracranial aneurysms. Ann. Biomed. Eng. 38:3058–3069, 2010. https://doi.org/10.1007/s10439-010-0065-8.
Prisco, A.R., Aliseda, A., Beckman, J.A., Mokadam, N.A., Mahr, C. and Garcia, G.J. Impact of LVAD implantation site on ventricular blood stagnation. ASAIO J. 63:392–400, 2017. https://doi.org/10.1097/MAT.0000000000000503.
Hariharan, P., M. Giarra, V. Reddy, S. W. Day, K. B. Manning, S. Deutsch, S. F. C. Stewart, M. R. Myers, M. R. Berman, G. W. Burgreen, E. G. Paterson, and R. A. Malinauskas. Multilaboratory particle image velocimetry analysis of the FDA benchmark nozzle model to support validation of computational fluid dynamics simulations. J. Biomech. Eng. 2011. https://doi.org/10.1115/1.4003440/450920.
Hendabadi, S., J. Bermejo, Y. Benito, R. Yotti, F. Fernández-Avilés, J. C. D. Álamo, and S. C. Shadden. Topology of blood transport in the human left ventricle by novel processing of Doppler echocardiography. Ann. Biomed. Eng. 41:2603–2616, 2013. https://doi.org/10.1007/s10439-013-0853-z.
Dobarro, D., M. Urban, K. Booth, N. Wrightson, J. Castrodeza, J. Jungschleger, N. Robinson-Smith, A. Woods, G. Parry, S. Schueler, and G. A. Macgowan. Impact of aortic valve closure on adverse events and outcomes with the HeartWare ventricular assist device. J. Heart Lung Transplant. 36:42–49, 2016. https://doi.org/10.1016/j.healun.2016.08.006.
Tolpen, S., J. Janmaat, C. Reider, F. Kallel, D. Farrar, and K. May-Newman. Programmed speed reduction enables aortic valve opening and increased pulsatility in the LVAD-assisted heart. ASAIO J. 61:540–547, 2015. https://doi.org/10.1097/MAT.0000000000000241.
Bruckner, B. A., D. J. DiBardino, Q. Ning, A. Adeboygeun, K. Mahmoud, J. Valdes, J. Eze, P. M. Allison, D. A. Cooley, I. D. Gregoric, and O. H. Frazier. High incidence of thromboembolic events in left ventricular assist device patients treated with recombinant activated factor VII. J. Heart Lung Transplant. 28:785–790, 2009. https://doi.org/10.1016/J.HEALUN.2009.04.028.
Liao, S., M. Neidlin, Z. Li, B. Simpson, and S. D. Gregory. Ventricular flow dynamics with varying LVAD inflow cannula lengths: In-silico evaluation in a multiscale model. J. Biomech. 72:106–115, 2018. https://doi.org/10.1016/j.jbiomech.2018.02.038.
Funding
This work was funded by the National Science Foundation Graduate Research Fellowship Program (NSF GRFP) AHRQ (Grant No. 1 R18 HS 026690; Funder ID: 10.13039/100000133). Experimental work has been financially supported by the Locke Trust through a gift to the Division of Cardiology of the University of Washington and the American Heart Association via a Postdoctoral fellowship (19POST34450082). This work was facilitated through the use of advanced computational, storage, and networking infrastructure provided by the Hyak supercomputer system and funded by the Student Technology Fund at the University of Washington.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no conflict of interest.
Additional information
Associate Editor Stefan M. Duma oversaw review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1
Bland-Altman plots of differences in CFD and PIV velocity magnitude for speed modulation synchronized with systole in the posterior–anterior and left–right views a at peak diastole, b at peak systole, c at low RPM and d at high RPM in the pulsatility mode with the median (labeled in bold face) and 95% confidence intervals (labeled with italics) identified with dashed lines
Diversity Statement
Recent work in several fields of science has identified a bias in citation practices such that papers from women and other minority scholars are undercited relative to the number of papers in the field. We recognize this bias and have worked diligently to ensure that we are referencing appropriate papers with fair gender and racial author inclusion.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Straccia, A., Chassagne, F., Barbour, M.C. et al. A Computational Investigation of the Effects of Temporal Synchronization of Left Ventricular Assist Device Speed Modulation with the Cardiac Cycle on Intraventricular Hemodynamics. Ann Biomed Eng (2024). https://doi.org/10.1007/s10439-024-03489-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10439-024-03489-x