Abstract
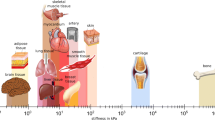
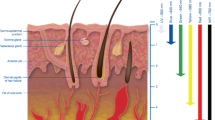
It is quite challenging to describe heat transfer phenomena in living systems because of the involved phenomena complexity. Indeed, thermal conduction and convection in tissues, blood perfusion, heat generation due to metabolism, complex vascular structure, changing of tissue properties depending on various conditions, are some of the features that make hard to obtain an accurate knowledge of heat transfer in living systems for all the clinical situations. This theme has a key role to predict accurately the temperature distribution in tissues, especially during biomedical applications, such as hyperthermia treatment of cancer, in which tumoral cells have to be destroyed and at the same time the surrounding healthy tissue has to be preserved. Moreover, the lack of experimentation in this field, due to ethical reasons, makes bioheat models even more significant. The first simple bioheat model was developed in 1948 by Pennes (J Appl Physiol 1:93–122, 1948) but it has some shortcomings that make the equation not so accurate. For this reason, over the years it has been modified and more complex models have been developed. The purpose of this review is to give a clear overview of how the bioheat models have been modified when applied in various hyperthermia treatments of cancer.



Similar content being viewed by others
Abbreviations
- a :
-
Specific surface area between blood and tissue (m−1)
- a c :
-
Antenna constant (m−1)
- A :
-
Maximum power density (W m−3)
- A tm :
-
Area of the tumor (m2)
- c v :
-
Nanoparticle concentration in the blood flow (kg L−1)
- C :
-
Specific heat (J kg−1 K)
- E :
-
Modulus of the electric field (V m−1)
- f :
-
Frequency (Hz)
- \(f_{\text{T}} \left( {c_{\text{v}} } \right)\) :
-
Source term caused by alternating magnetic field (W m−3)
- G :
-
Incident radiation (W m−2)
- g, F :
-
Functions depending on the radiative heat transfer (W m−3)
- h :
-
Heat transfer coefficient (W m−2 K−1)
- H :
-
Magnetic field (T)
- I :
-
Scattered diffuse intensity (W m−2)
- I ac :
-
Local acoustic intensity (W m−2)
- j 0 :
-
Current density (A m−2)
- k :
-
Thermal conductivity (W m−1 K−1)
- L :
-
Specific thermal effects of chemical conversions (m2 s−2)
- L LFp :
-
Lymphatic permeability (m Pa−1 s−1)
- n :
-
Refractive index (–)
- n inj :
-
Total number of injection points (–)
- n np :
-
Number of nanoparticles (–)
- P :
-
Transmitted antenna power (W)
- q :
-
Heat flux (W m−2)
- Q :
-
Power density (W m−3)
- R mil :
-
Radius of magnetic loop (m)
- r :
-
Radial coordinate (m)
- r 0 :
-
Electrode radius (m)
- r dist :
-
Tissue/outer surface relative distance (m)
- \(\bar{r}\) :
-
Distance covered by the heat generated by nanoparticles (m)
- r inj :
-
Radial distance of the injection (m)
- r np :
-
Mean radius of nanoparticles (m)
- S :
-
Antenna constant (m−1)
- SAR :
-
Specific absorption rate (W kg−1)
- t :
-
Time (s)
- T :
-
Temperature (K)
- u :
-
Velocity (m s−1)
- u, w :
-
Velocity components (m s−1)
- u q(t):
-
Step function (–)
- W :
-
Tissue water density (kg m−3)
- ∞ :
-
Far away from heating focus
- a:
-
Arterial
- b:
-
Blood
- cr:
-
Critical
- ch:
-
Channel conversion
- dis:
-
Dispersion
- e:
-
Effective
- E:
-
Energy to vaporize water
- Ext:
-
External
- Fat:
-
Referred to fat
- Laser:
-
Referred to laser energy
- max:
-
Maximum
- met:
-
Metabolism
- muscle:
-
Referred to muscle
- np:
-
Nanoparticles
- p:
-
Probe
- r:
-
Radiative
- ref:
-
Reference
- t:
-
Tissue
- tm:
-
Tumor
- v:
-
Venous
- α :
-
Absorption coefficient (Np Hz−1 m−1)
- α diff :
-
Effective thermal diffusivity (m2 s−1)
- δ Λ :
-
Parameter that refers to the microvascular network (–)
- γ :
-
Water latent heat constant (J kg−1)
- Φ:
-
Phase function (–)
- Γ:
-
Coordinates index (–)
- Γf :
-
Euler gamma function (–)
- ε :
-
Porosity (–)
- θ :
-
Nanoparticles concentration (–)
- χ ″ :
-
Imaginary part of susceptibility of the magnetic nanoparticles (–)
- ρ :
-
Density (kg m−3)
- P :
-
Arithmetic average of each segment contained into the tumor (m)
- Ψ :
-
Density of nanoparticles on the vascular walls (L m−2)
- σ s :
-
Stefan–Boltzmann constant (W m−2 K−4)
- σ :
-
Electric conductivity (S m−1)
- τ :
-
Relaxation time (s)
- τ q :
-
Phase-lag of the heat flux (s)
- τ T :
-
Phase-lag of temperature gradient (s)
- μ cr :
-
Critical cosine of an angle (–)
- μ 0 :
-
Dielectric vacuum permeability (H m−1)
- ω :
-
Blood perfusion (s−1)
- ω tr :
-
Nanoshell transport albedo (–)
- ω b0 :
-
Constant blood perfusion (s−1)
- Ω :
-
Solid angle (–)
- Ω(t):
-
tissue injury degree (–)
References
Au, J. L., S. H. Jang, J. Zheng, C. T. Chen, S. Song, L. Hu, and M. G. Wientjes. Determinants of drug delivery and transport in solid tumors. J. Control Release 74:31–46, 2001.
Berjano, E. J. Theoretical modeling for radiofrequency ablation: state-of-the-art and challenges for the future. Biomed. Eng. Online 18:5–24, 2006.
Bermeo Varon, L. A., H. R. Barreto Orlande, and G. E. Eliçabe. Estimation of state variables in the hyperthermia therapy of cancer with heating imposed by radiofrequency electromagnetic waves. Int. J. Therm. Sci. 98:228–236, 2015.
Bermeo Varon, L. A., H. R. Barreto Orlande, and G. E. Eliçabe. Combined parameter and state estimation in the radio frequency hyperthermia treatment of cancer. Numer. Heat Transf. A 70:581–594, 2016.
Cavagnaro, M., R. Pinto, and V. Lopresto. Numerical models to evaluate the temperature increase induced by ex vivo microwave thermal ablation. Phys. Med. Biol. 60:3287–3311, 2015.
Chen, M. M., and K. R. Holmes. Microvascular contributions in tissue heat transfer. Ann. N. Y. Acad. Sci. 335:137–142, 1980.
Dombrovsky, L. A., V. Timchenko, and M. Jackson. Indirect heating strategy for laser induced hyperthermia: an advanced thermal model. Int. J. Heat Mass Transf. 55:4688–4700, 2012.
Dombrovsky, L. A., V. Timchenko, M. Jackson, and G. H. Yeoh. A combined transient thermal model for laser hyperthermia of tumors with embedded gold nanoshells. Int. J. Heat Mass Transf. 54:5459–5469, 2011.
Emami, B., and C. W. Song. Physiological mechanisms in hyperthermia: a review. Int. J. Radiat. Oncol. Biol. Phys. 10:289–295, 1984.
Furusawa, H., K. Namba, S. Thomsen, F. Akiyama, A. Bendet, C. Tanaka, Y. Yasuda, and H. Nakahara. Magnetic resonance-guided focused ultrasound surgery of breast cancer: reliability and effectiveness. J. Am. Coll. Surg. 203:54–63, 2006.
Guerrero López, G. D., M. F. J. Cepeda Rubio, J. I. Hernández Jácquez, A. Vera Hernandez, L. Lejia Salas, F. Valdes Perezgasga, and F. FloresGarcia. Computational fem model, phantom and ex vivo swine breast validation of an optimized double-slot microcoaxial antenna designed for minimally invasive breast tumor ablation: theoretical and experimental comparison of temperature, size of lesion, and swr, preliminary data. Comput. Math. Methods Med. 1:1–11, 2017.
Gupta, P. K., J. Singh, and K. N. Rai. A numerical study on heat transfer in tissues during hyperthermia. Math. Comput. Model. 57:1018–1037, 2013.
Gupta, P. K., J. Singh, K. N. Rai, and S. K. Rai. Solution of the heat transfer problem in tissues during hyperthermia by finite difference–decomposition method. Appl. Math. Comput. 219:6882–6892, 2013.
Herman, T. S., and B. A. Teicher. Summary of studies adding systemic chemotherapy to local hyperthermia and radiation. Int. J. Hyperther. 10:443–449, 1994.
Issels, R. D., L. H. Lindner, J. Verweij, P. Wust, P. Reichardt, B. C. Schem, S. Abdel-Rahman, S. Daugaard, C. Salat, C. M. Wendtner, Z. Vujaskovic, R. Wessalowski, K. W. Jauch, H. R. Dürr, F. Ploner, A. Baur-Melnyk, U. Mansmann, W. Hiddemann, J. Y. Blay, P. Hohenberger, and European Organisation for Research and Treatment of Cancer Soft Tissue and Bone Sarcoma Group/EORTC-STBSG) and the European Society for Hyperthermic Oncology (ESHO). Neo-adjuvant chemotherapy alone or with regional hyperthermia for localised high-risk soft tissue sarcoma: a randomised phase 3 multicentre study. Lancet Oncol. 11:561–570, 2010.
Jaunich, M., S. Raje, K. Kim, K. Mitra, and Z. Guo. Bio-heat transfer analysis during short pulse laser irradiation of tissues. Int. J. Heat Mass Transf. 51:5511–5521, 2008.
Jones, E. L., J. R. Oleson, L. R. Prosnitz, T. V. Samulski, Z. Vujaskovic, D. Yu, L. L. Sanders, and M. W. Dewhirst. A randomized trial of hyperthermia and radiation for superficial tumors. J. Clin. Oncol. 23:3079–3085, 2005.
Keangin, P., and P. Rattanadecho. Analysis of heat transport on local thermal non-equilibrium in porous liver during microwave ablation. Int. J. Heat Mass Transf. 67:46–60, 2013.
Keangin, P., and P. Rattanadecho. Numerical study of heat transfer and blood flow in two-layered porous liver tissue during microwave ablation process using single and double slot antenna. Int. J. Heat Mass Transf. 58:457–470, 2013.
Keangin, P., P. Rattanadecho, and T. Wessapan. An analysis of heat transfer in liver tissue during microwave ablation using single and double slot antenna. Int. Commun. Heat Mass Transf. 38:757–766, 2011.
Keangin, P., T. Wessapan, and P. Rattanadecho. Analysis of heat transfer in deformed liver cancer modeling treated using a microwave coaxial antenna. Appl. Therm. Eng. 31:3243–3252, 2011.
Khaled, A. R. A., and K. Vafai. The role of porous media in modeling flow and heat transfer in biological tissues. Int. J. Heat Mass Transf. 46:4989–5003, 2003.
Khanafer, K., J. L. Bull, I. Pop, and R. Berguer. Influence of pulsatile blood flow and heating scheme on the temperature distribution during hyperthermia treatment. Int. J. Heat Mass Transf. 50:4883–4890, 2007.
Khanafer, K., and K. Vafai. The role of porous media in biomedical engineering as related to magnetic resonance imaging and drug delivery. Int. J. Heat Mass Transf. 42:939–953, 2006.
Klinger, H. G. Heat transfer in perfused biological tissue I: general theory. Bull. Math. Biol. 36:403–415, 1974.
Kumar, D. K., and K. N. Rai. Numerical simulation of time fractional dual-phase-lag model of heat transfer within skin tissue during thermal therapy. J. Therm. Biol. 67:49–58, 2017.
Lee, D. Y., and K. Vafai. Analytical characterization and conceptual assessment of solid and fluid temperature differentials in porous media. Int. J. Heat Mass Transf. 42:423–435, 1999.
Leong, K. C., C. Yang, and S. M. S. Murshed. A model for the thermal conductivity of nanofluids—the effect of interfacial layer. J. Nanopart. Res. 8:245–254, 2006.
Liu, K. C., and H. T. Chen. Analysis for the dual-phase-lag bio-heat transfer during magnetic hyperthermia treatment. Int. J. Heat Mass Transf. 52:1185–1192, 2009.
Lopez Molina, J. A., M. J. Rivera, and E. Berjano. Analytical model based on a cylindrical geometry to study RF ablation with needle-like internally cooled electrode. Math. Probl. Eng. 2012. https://doi.org/10.1155/2012/834807.
Lopez Molina, J. A., M. J. Rivera, and E. Berjano. Analytical transient-time solution for temperature in non perfused tissue during radiofrequency ablation. Appl. Math. Model. 42:618–635, 2017.
Mahjoob, S., and K. Vafai. Analytical characterization of heat transport through biological media incorporating hyperthermia treatment. Int. J. Heat Mass Transf. 52:1608–1618, 2009.
Mahjoob, S., and K. Vafai. Analysis of bioheat transport through a dual layer biological media. ASME J Heat Transf. 132:031101–031114, 2010.
Mahjoob, S., and K. Vafai. Analysis of heat transfer in consecutive variable cross-sectional domains: applications in biological media and thermal management. ASME J Heat Transf. 133:011006-1–011006-9, 2011.
Majchrzak, E., G. Dziatkiewicz, and M. Paruch. The modelling of heating a tissue subjected to external electromagnetic field. Acta Bioeng. Biomech. 10:29–37, 2008.
Minchinton, A. I., and I. F. Tannock. Drug penetration in solid tumors. Nat. Rev. Cancer. 6:583–592, 2006.
Moros, E. G., and W. R. Hendee. Physics of Thermal Therapy: Fundamentals and Clinical Applications. Boca Raton: CRC Press, Taylor & Francis Group, 2012.
Nabil, M., P. Decuzzi, and P. Zunino. Modelling mass and heat transfer in nano-based cancer hyperthermia. R. Soc. Open Sci. 2:150447, 2015.
Nabil, M., and P. Zunino. A computational study of cancer hyperthermia based on vascular magnetic nanoconstructs. R. Soc. Open Sci. 3:160287, 2016.
Nakayama, A., and F. Kuwahara. A general bioheat transfer model based on the theory of porous media. Int. J. Heat Mass Transf. 51:3190–3199, 2008.
Ortega Palacios, R., C. J. Trujillo Romero, and M. F. J. Cepeda Rubio. A feasibility of using a novel 2.45 GHz double short distance slot coaxial antenna for minimally invasive cancer breast microwave ablation therapy: computational model, phantom, and in vivo swine experimentation. J. Healthc. Eng. 2018. https://doi.org/10.1155/2018/5806753.
Peek, M. C., M. Ahmed, A. Napoli, S. Usiskin, R. Baker, and M. Douek. Minimally invasive ablative techniques in the treatment ofbreast cancer: a systematic review and meta-analysis. Int. J. Hyperther. 33:1–12, 2016.
Pennes, H. H. Analysis of tissue and arterial blood flow temperatures in the resting forearm. J. Appl. Physiol. 1:93–122, 1948.
Primeau, A. J., A. Rendon, D. Hedley, L. Lilge, and I. F. Tannock. The distribution of the anticancer drug doxorubicin in relation to blood vessels in solid tumors. Clin. Cancer Res. 11:8782–8788, 2005.
Reis, R. F., F. Dos SantosLoureiro, and M. Lobosco. 3D numerical simulations on GPUs of hyperthermia with nanoparticles by a nonlinear bioheat model. J. Comput. Appl. Math. 295:35–47, 2016.
Roetzel, W., and Y. Xuan. Bioheat equation of the human thermal system. Chem. Eng. Technol. 20:268–276, 1997.
Shao, Y. L., B. Arjun, H. L. Leo, and K. J. Chua. Nano-assisted radiofrequency ablation of clinically extracted irregularly-shaped liver tumours. J. Therm. Biol. 66:101–113, 2017.
Sheu, T. W. H., M. A. Solovchuk, A. W. J. Chen, and M. Thiriet. On an acoustics–thermal–fluid coupling model for the prediction of temperature elevation in liver tumor. Int. J. Heat Mass Transf. 54:4117–4126, 2011.
Tzou, D. Y. A unified field approach for heat conduction from macro- to micro-scales. J. Heat Transf. 117:8–16, 1995.
Tzou, D. Y. Experimental support for the lagging behaviour in heat propagation. J. Thermophys. Heat Transf. 9:686–693, 1995.
Vafai, K. Handbook of porous media (3rd ed.). Boca Raton: CRC Press, Taylor & Francis Group, 2015.
Van der Zee, J. Heating the patient: a promising approach? Ann. Oncol. 13:1173–1184, 2002.
Vyas, D. C. M., S. Kumar, and A. Srivastava. Porous media based bio-heat transfer analysis on counter-current artery vein tissue phantoms: applications in photo thermal therapy. Int. J. Heat Mass Transf. 99:122–140, 2016.
Wang, K., F. Tavakkoli, S. Wang, and K. Vafai. Analysis and analytical characterization of bioheat transfer during radiofrequency ablation. J. Biomech. 48:930–940, 2015.
Weinbaum, S., and L. Jiji. A new simplified bioheat equation for the effect of blood flow on local average tissue temperature. J. Biomech. Eng. 107:131–141, 1985.
Weinbaum, S., L. Jiji, and D. E. Lemons. Theory and experiment for the effect of vascular microstructure on surface tissue heat transfer—part I: anatomical foundation and model conceptualization. J. Biomech. Eng. 106:321–330, 1984.
Weinbaum, S., L. Jiji, and D. E. Lemons. Theory and experiment for the effect of vascular microstructure on surface tissue heat transfer—part II: model formulation and solution. J. Biomech. Eng. 106:331–341, 1984.
Wulff, W. The energy conservation equation for living tissue. IEEE Trans. Biomed. Eng. 21:494–497, 1974.
Yang, D., M. Converse, and J. G. Webster. Expanding the bioheat equation to include tissue internal water evaporation during heating. IEEE Transact. Biomed. Eng. 54:1382–1388, 2007.
Yuan, P. Numerical analysis of temperature and thermal dose response of biological tissues to thermal non-equilibrium during hyperthermia therapy. Med. Eng. Phys. 30:35–43, 2008.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Estefanía Peña oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Andreozzi, A., Brunese, L., Iasiello, M. et al. Modeling Heat Transfer in Tumors: A Review of Thermal Therapies. Ann Biomed Eng 47, 676–693 (2019). https://doi.org/10.1007/s10439-018-02177-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10439-018-02177-x