Abstract
Advanced age is widely recognized as a key risk factor for incident cardiovascular disease. The age-associated changes in cardiac properties alter the substrate on which cardiovascular disease is superimposed in various ways, and thus affect the development and manifestations of cardiovascular disease (CVD) in the elderly. However, it is still unclear whether age-related cardiac alteration is attributed to aging itself or whether it is secondary to other acquired cardiovascular risk factors. Understanding the association between aging and cardiac functional remodeling might provide insight into the pathogenesis of cardiovascular aging and may help inform possible preventive strategies for CVD in older individuals. Speckle-tracking echocardiography enables the objective and quantitative assessment of subtle myocardial alterations that are undetectable with conventional echocardiography, and has excellent feasibility and reproducibility. Left ventricular (LV) global longitudinal strain, a sensitive measure of LV systolic dysfunction, was found to be an independent risk factor for cardiovascular morbidity and mortality. More recently, deformation imaging has been employed to assess right ventricular (RV) and atrial performance, and impaired RV and atrial strain predict unfavorable outcomes in various clinical settings. This article reviews the association between aging and changes in myocardial strain values and describes future perspectives.



Similar content being viewed by others
References
Shapiro MD, Maron DJ, Morris PB, et al. Preventive cardiology as a subspecialty of cardiovascular medicine: JACC council perspectives. J Am Coll Cardiol. 2019;74:1926–42.
Wong TC, Piehler KM, Kang IA, et al. Myocardial extracellular volume fraction quantified by cardiovascular magnetic resonance is increased in diabetes and associated with mortality and incident heart failure admission. Eur Heart J. 2014;35:657–64.
Bianco CM, Farjo PD, Ghaffar YA, et al. Myocardial mechanics in patients with normal LVEF and diastolic dysfunction. JACC Cardiovasc Imaging. 2020;13:258–71.
Marwick TH, Leano RL, Brown J, et al. Myocardial strain measurement with 2-dimensional speckle-tracking echocardiography: definition of normal range. JACC Cardiovasc Imaging. 2009;2:80–4.
Nakanishi K, Daimon M, Yoshida Y, et al. Serum uric acid level and subclinical left ventricular dysfunction: a community-based cohort study. ESC Heart Fail. 2020;7:1031–8.
Hirose K, Nakanishi K, Daimon M, et al. Impact of insulin resistance on subclinical left ventricular dysfunction in normal weight and overweight/obese Japanese subjects in a general community. Cardiovasc Diabetol. 2021;20:22.
Voigt JU, Pedrizzetti G, Lysyansky P, et al. Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. J Am Soc Echocardiogr. 2015;28:183–93.
Badano LP, Kolias TJ, Muraru D, et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging. 2018;19:591–600.
Charisopoulou D, Banner NR, Demetrescu C, et al. Right atrial and ventricular echocardiographic strain analysis predicts requirement for right ventricular support after left ventricular assist device implantation. Eur Heart J Cardiovasc Imaging. 2019;20:199–208.
Nakanishi K, Daimon M, Yoshida Y, et al. Carotid intima-media thickness and subclinical left heart dysfunction in the general population. Atherosclerosis. 2020;305:42–9.
Sawada N, Nakanishi K, Daimon M, et al. Influence of visceral adiposity accumulation on adverse left and right ventricular mechanics in the community. Eur J Prev Cardiol. 2020;27:2006–15.
Yoshida Y, Nakanishi K, Daimon M, et al. Association of arterial stiffness with left atrial structure and phasic function: a community-based cohort study. J Hypertens. 2020;38:1140–8.
Nakanishi K, Daimon M, Yoshida Y, et al. Relation of Body Mass Index to adverse right ventricular mechanics. Am J Cardiol. 2021;144:137–42.
Otterstad JE, Froeland G, St John Sutton M, et al. Accuracy and reproducibility of biplane two-dimensional echocardiographic measurements of left ventricular dimensions and function. Eur Heart J. 1997;18:507–13.
Ho SY. Anatomy and myoarchitecture of the left ventricular wall in normal and in disease. Eur J Echocardiogr. 2009;10:iii3–7.
Hoit BD. Strain and strain rate echocardiography and coronary artery disease. Circ Cardiovasc Imaging. 2011;4:179–90.
Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–200.
Morris DA, Otani K, Bekfani T, et al. Multidirectional global left ventricular systolic function in normal subjects and patients with hypertension: multicenter evaluation. J Am Soc Echocardiogr. 2014;27:493–500.
Alcidi GM, Esposito R, Evola V, et al. Normal reference values of multilayer longitudinal strain according to age decades in a healthy population: a single-centre experience. Eur Heart J Cardiovasc Imaging. 2018;19:1390–6.
Sugimoto T, Dulgheru R, Bernard A, et al. Echocardiographic reference ranges for normal left ventricular 2D strain: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging. 2017;18:833–40.
Takigiku K, Takeuchi M, Izumi C, et al. Normal range of left ventricular 2-dimensional strain: Japanese Ultrasound Speckle Tracking of the Left Ventricle (JUSTICE) study. Circ J. 2012;76:2623–32.
Cheng S, Larson MG, McCabe EL, et al. Age- and sex-based reference limits and clinical correlates of myocardial strain and synchrony: the Framingham Heart Study. Circ Cardiovasc Imaging. 2013;6:692–9.
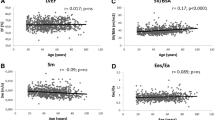
Yoshida Y, Nakanishi K, Daimon M, et al. Alteration of cardiac performance and Serum B-Type Natriuretic peptide level in healthy aging. J Am Coll Cardiol. 2019;74:1789–800.
Yingchoncharoen T, Agarwal S, Popovic ZB, et al. Normal ranges of left ventricular strain: a meta-analysis. J Am Soc Echocardiogr. 2013;26:185–91.
D’Elia N, Caselli S, Kosmala W, et al. Normal global longitudinal strain: an individual patient meta-analysis. JACC Cardiovasc Imaging. 2020;13:167–9.
Obokata M, Nagata Y, Wu VC, et al. Direct comparison of cardiac magnetic resonance feature tracking and 2D/3D echocardiography speckle tracking for evaluation of global left ventricular strain. Eur Heart J Cardiovasc Imaging. 2016;17:525–32.
Sakurai D, Asanuma T, Masuda K, et al. New parameter derived from three-dimensional speckle-tracking echocardiography for the estimation of left ventricular filling pressure in nondilated hearts. J Am Soc Echocardiogr. 2017;30:522–31.
Kaku K, Takeuchi M, Tsang W, et al. Age-related normal range of left ventricular strain and torsion using three-dimensional speckle-tracking echocardiography. J Am Soc Echocardiogr. 2014;27:55–64.
Kleijn SA, Pandian NG, Thomas JD, et al. Normal reference values of left ventricular strain using three-dimensional speckle tracking echocardiography: results from a multicentre study. Eur Heart J Cardiovasc Imaging. 2015;16:410–6.
Bernard A, Addetia K, Dulgheru R, et al. 3D echocardiographic reference ranges for normal left ventricular volumes and strain: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging. 2017;18:475–83.
Truong VT, Phan HT, Pham KNP, et al. Normal ranges of left ventricular strain by three-dimensional speckle-tracking echocardiography in adults: a systematic review and meta-analysis. J Am Soc Echocardiogr. 2019;32:1586–97.
Marcus KA, Janousek J, Barends ME, et al. Synchronicity of systolic deformation in healthy pediatric and young adult subjects: a two-dimensional strain echocardiography study. Am J Physiol Heart Circ Physiol. 2012;302:H196-205.
Sun JP, Lam YY, Wu CQ, et al. Effect of age and gender on left ventricular rotation and twist in a large group of normal adults—a multicenter study. Int J Cardiol. 2013;167:2215–21.
Menting ME, McGhie JS, Koopman LP, et al. Normal myocardial strain values using 2D speckle tracking echocardiography in healthy adults aged 20 to 72 years. Echocardiography. 2016;33:1665–75.
Melenovsky V, Hwang SJ, Lin G, et al. Right heart dysfunction in heart failure with preserved ejection fraction. Eur Heart J. 2014;35:3452–62.
Mohammed SF, Hussain I, AbouEzzeddine OF, et al. Right ventricular function in heart failure with preserved ejection fraction: a community-based study. Circulation. 2014;130:2310–20.
Hamada-Harimura Y, Seo Y, Ishizu T, et al. Incremental prognostic value of right ventricular strain in patients with acute decompensated heart failure. Circ Cardiovasc Imaging. 2018;11:e007249.
Di Salvo TG, Mathier M, Semigran MJ, et al. Preserved right ventricular ejection fraction predicts exercise capacity and survival in advanced heart failure. J Am Coll Cardiol. 1995;25:1143–53.
Borlaug BA, Kane GC, Melenovsky V, et al. Abnormal right ventricular-pulmonary artery coupling with exercise in heart failure with preserved ejection fraction. Eur Heart J. 2016;37:3293–302.
Guazzi M, Dixon D, Labate V, et al. RV contractile function and its coupling to pulmonary circulation in heart failure with preserved ejection fraction: stratification of clinical phenotypes and outcomes. JACC Cardiovasc Imaging. 2017;10:1211–21.
Kusunose K, Seno H, Yamada H, et al. Right ventricular function and beneficial effects of cardiac rehabilitation in patients with systolic chronic heart failure. Can J Cardiol. 2018;34:1307–15.
Nochioka K, Querejeta Roca G, Claggett B, et al. Right ventricular function, right ventricular-pulmonary artery coupling, and heart failure risk in 4 US communities: the atherosclerosis risk in communities (ARIC) study. JAMA Cardiol. 2018;3:939–48.
Focardi M, Cameli M, Carbone SF, et al. Traditional and innovative echocardiographic parameters for the analysis of right ventricular performance in comparison with cardiac magnetic resonance. Eur Heart J Cardiovasc Imaging. 2015;16:47–52.
Morris DA, Krisper M, Nakatani S, et al. Normal range and usefulness of right ventricular systolic strain to detect subtle right ventricular systolic abnormalities in patients with heart failure: a multicentre study. Eur Heart J Cardiovasc Imaging. 2017;18:212–23.
Muraru D, Onciul S, Peluso D, et al. Sex- and method-specific reference values for right ventricular strain by 2-dimensional speckle-tracking echocardiography. Circ Cardiovasc Imaging. 2016;9:e003866.
Addetia K, Takeuchi M, Maffessanti F, et al. Simultaneous longitudinal strain in all 4 cardiac chambers: a novel method for comprehensive functional assessment of the heart. Circ Cardiovasc Imaging. 2016;9:e003895.
Olivetti G, Melissari M, Capasso JM, et al. Cardiomyopathy of the aging human heart. Myocyte loss and reactive cellular hypertrophy. Circ Res. 1991;68:1560–8.
Li Y, Zhang L, Gao Y, et al. Comprehensive assessment of right ventricular function by three-dimensional speckle-tracking echocardiography: comparisons with cardiac magnetic resonance imaging. J Am Soc Echocardiogr. 2021;34:472–82.
Brecht A, Oertelt-Prigione S, Seeland U, et al. Left atrial function in preclinical diastolic dysfunction: two-dimensional speckle-tracking echocardiography-derived results from the BEFRI Trial. J Am Soc Echocardiogr. 2016;29:750–8.
Singh A, Addetia K, Maffessanti F, et al. LA strain for categorization of LV diastolic dysfunction. JACC Cardiovasc Imaging. 2017;10:735–43.
Morris DA, Belyavskiy E, Aravind-Kumar R, et al. Potential usefulness and clinical relevance of adding left atrial strain to left atrial volume index in the detection of left ventricular diastolic dysfunction. JACC Cardiovasc Imaging. 2018;11:1405–15.
Nakanishi K, Daimon M, Yoshida Y, et al. Subclinical hypothyroidism as an independent determinant of left atrial dysfunction in the general population. J Clin Endocrinol Metab. 2021;106:e1859–67.
Potter EL, Ramkumar S, Kawakami H, et al. Association of asymptomatic diastolic dysfunction assessed by left atrial strain with incident heart failure. JACC Cardiovasc Imaging. 2020;13:2316–26.
Morris DA, Parwani A, Huemer M, et al. Clinical significance of the assessment of the systolic and diastolic myocardial function of the left atrium in patients with paroxysmal atrial fibrillation and low CHADS(2) index treated with catheter ablation therapy. Am J Cardiol. 2013;111:1002–11.
Patel RB, Delaney JA, Hu M, et al. Characterization of cardiac mechanics and incident atrial fibrillation in participants of the Cardiovascular Health Study. JCI Insight. 2020;5:e141656.
Sun JP, Yang Y, Guo R, et al. Left atrial regional phasic strain, strain rate and velocity by speckle-tracking echocardiography: normal values and effects of aging in a large group of normal subjects. Int J Cardiol. 2013;168:3473–9.
Morris DA, Takeuchi M, Krisper M, et al. Normal values and clinical relevance of left atrial myocardial function analysed by speckle-tracking echocardiography: multicentre study. Eur Heart J Cardiovasc Imaging. 2015;16:364–72.
Liao JN, Chao TF, Kuo JY, et al. Age, sex, and blood pressure-related influences on reference values of left atrial deformation and mechanics from a large-scale Asian Population. Circ Cardiovasc Imaging. 2017;10:e006077.
Thum T, Gross C, Fiedler J, et al. MicroRNA-21 contributes to myocardial disease by stimulating MAP kinase signalling in fibroblasts. Nature. 2008;456:980–4.
Burstein B, Libby E, Calderone A, Nattel S. Differential behaviors of atrial versus ventricular fibroblasts: a potential role for platelet-derived growth factor in atrial-ventricular remodeling differences. Circulation. 2008;117:1630–41.
Hanna N, Cardin S, Leung TK, Nattel S. Differences in atrial versus ventricular remodeling in dogs with ventricular tachypacing-induced congestive heart failure. Cardiovasc Res. 2004;63:236–44.
Pathan F, D’Elia N, Nolan MT, et al. Normal ranges of left atrial strain by speckle-tracking echocardiography: a systematic review and meta-analysis. J Am Soc Echocardiogr. 2017;30:59–70.
Sallach JA, Tang WH, Borowski AG, et al. Right atrial volume index in chronic systolic heart failure and prognosis. JACC Cardiovasc Imaging. 2009;2:527–34.
Cioffi G, de Simone G, Mureddu G, et al. Right atrial size and function in patients with pulmonary hypertension associated with disorders of respiratory system or hypoxemia. Eur J Echocardiogr. 2007;8:322–31.
Peluso D, Badano LP, Muraru D, et al. Right atrial size and function assessed with three-dimensional and speckle-tracking echocardiography in 200 healthy volunteers. Eur Heart J Cardiovasc Imaging. 2013;14:1106–14.
Soulat-Dufour L, Addetia K, Miyoshi T, et al. Normal values of right atrial size and function according to age, sex, and ethnicity: results of the world alliance societies of echocardiography study. J Am Soc Echocardiogr. 2021;34:286–300.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no disclosures pertinent to the content of the manuscript. The authors declare that there are no conflicts of interest.
Ethical statements
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nakanishi, K., Daimon, M. Aging and myocardial strain. J Med Ultrasonics 49, 53–60 (2022). https://doi.org/10.1007/s10396-021-01115-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10396-021-01115-0