Abstract
Background
Understanding the effects of the COVID-19 pandemic on cause-specific mortality should be a priority, as this metric allows for a detailed analysis of the true burden of the pandemic. The aim of this systematic literature review is to estimate the impact of the pandemic on different causes of death, providing a quantitative and qualitative analysis of the phenomenon.
Methods
We searched MEDLINE, Scopus, and ProQuest for studies that reported cause-specific mortality during the COVID-19 pandemic, extracting relevant data.
Results
A total of 2413 articles were retrieved, and after screening 22 were selected for data extraction. Cause-specific mortality results were reported using different units of measurement. The most frequently analyzed cause of death was cardiovascular diseases (n = 16), followed by cancer (n = 14) and diabetes (n = 11). We reported heterogeneous patterns of cause-specific mortality, except for suicide and road accident.
Conclusions
Evidence on non-COVID-19 cause-specific deaths is not exhaustive. Reliable scientific evidence is needed by policymakers to make the best decisions in an unprecedented and extremely uncertain historical period. We advocate for the urgent need to find an international consensus to define reliable methodological approaches to establish the true burden of the COVID-19 pandemic on non-COVID-19 mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the SARS-CoV-2 pandemic, a surge in overall deaths has been recorded in many countries, most of them probably attributable to COVID-19 (Wang et al. 2022). Numerous researchers investigated the patterns of COVID-19-related excess mortality at the international, national, and subnational levels (Kontis et al. 2020; Ahmad and Anderson 2021), with most of the studies focusing on all-cause mortality. Excess mortality analysis investigates the difference between the reported number of deaths within a given time in a location, and the number of expected deaths in “normal conditions” (often estimated using the same period in the preceding year or averaged over several preceding years) (Beaney et al. 2020). All-cause mortality is considered a strong and comprehensive indicator that reflects the full burden of the pandemic as it considers the pandemic’s direct and indirect effects on individuals, healthcare systems, and society as a whole (Beaney et al. 2020) and allows to nullify the differences in COVID-19 reporting and testing strategies and in the misclassification of the cause of death on certificates (Sanmarchi et al. 2021).
Although this information is relevant, understanding the effects of the pandemic on cause-specific mortality is crucial and should be deeply assessed, as this metric allows for a more detailed analysis of the true impact of the pandemic on people's health. Specifically, through cause-specific mortality, researchers analyze the pandemic indirect effects on other communicable and non-communicable diseases. Thus, investigating cause-specific mortality would lead to overcoming all-cause excess mortality limitations and better understanding the true impact of the pandemic on society (Beaney et al. 2020).
On the one hand, the spreading of the SARS-CoV-2 infection has directly caused a huge number of deaths, especially in the older population (Banerjee et al. 2020; Gibertoni et al. 2021), becoming the third leading cause of death in 2020 (Ahmad and Anderson 2021); on the other hand, it may have indirectly changed the burden of mortality from other causes. For instance, the adoption of non-pharmaceutical interventions (e.g., physical-distancing, mask mandates, school closings) to control the COVID-19 pandemic determined a decreased risk of death from certain other causes (e.g., car accidents or work-related accidents) (Yasin et al. 2021). Conversely, overwhelmed healthcare systems and changes to clinical pathways may have affected standard care, thus increasing the number of deaths for many acute and chronic diseases (Santi et al. 2021; Golinelli et al. 2021) and possibly leading to an increase in mortality from underdiagnosed diseases (Arolas et al. 2021; Aron and Muellbauer 2022).
To the best of our knowledge, there are no systematic literature reviews that have analyzed trends of cause-specific mortality during the SARS-CoV-2 pandemic. Such evidence should guide policymakers and the healthcare systems and help them dealing with the pandemic and its aftermath. Therefore, we undertook a systematic literature review to summarize current knowledge on cause-specific mortality during the pandemic and we aimed at estimating the impact of this global health crisis on different causes of death, providing a quantitative and qualitative analysis of the phenomenon. Specifically, we evaluated the number of papers published for each cause of death, evaluated whether the effects of the pandemic are consistent among different countries, provided insights into the models used to estimate the expected mortality, and discussed the cause-specific mortality estimates.
Methods
We developed a search strategy, following the Preferred Reporting Items for Systematic Reviews (PRISMA) approach (Page et al. 2020), to identify studies that reported cause-specific mortality during the COVID-19 pandemic.
We searched the electronic databases MEDLINE , Scopus, and ProQuest (from January 1, 2020, to July 31, 2022).
We used the following search string for MEDLINE:
2020/01/01:2022/07/31[Date - Publication] AND (("excess"[All Fields] OR "excesses"[All Fields] OR "excessive"[All Fields] OR "excessively"[All Fields]) AND (("mortality"[MeSH Terms] OR "mortality"[All Fields] OR "mortalities"[All Fields] OR "mortality"[MeSH Subheading]) AND ("sars cov 2"[MeSH Terms] OR "sars cov 2"[All Fields] OR "covid"[All Fields] OR "covid 19"[MeSH Terms] OR "covid 19"[All Fields]) AND ("causative"[All Fields] OR "causatively"[All Fields] OR "causatives"[All Fields] OR "cause"[All Fields] OR "caused"[All Fields] OR "causing"[All Fields] OR "etiology"[MeSH Subheading] OR "etiology"[All Fields] OR "causes"[All Fields] OR "causality"[MeSH Terms] OR "causality"[All Fields] OR "disease-specific"[All Fields]))).
We used the following search string for Scopus:
( excess* ) AND ( ( mortality ) OR ( deaths ) ) AND ( covid-19 ) AND ( cause AND specific )
We used the following search terms for ProQuest:
“(excess mortality) AND (COVID-19) AND (cause-specific mortality)” , limiting the search to peer-reviewed articles in academic journals.
Inclusion and exclusion criteria
We adopted the following inclusion criteria: (i) original article, (ii) assessment of at least one cause-specific mortality during the pandemic period, (iii) assessed causes of deaths using the 10th revision of the International Classification of Diseases (ICD-10), (iv) reporting of at least one of the following outcomes: cause-specific mortality estimates or cause-specific excess mortality, and (v) full-length articles. We excluded articles based on the following criteria: (i) preprints of articles, (ii) reviews, and (iii) non-English-language articles.
Data extraction and analysis
Two independent investigators (EA, FE) evaluated each record to determine eligibility. All disagreements were discussed with an independent arbiter (FS) to reach consensus. The investigators (EA, FE) independently extracted the data. Disagreements were discussed with FS. Relevant data extracted from each article were: publication year, data stratification, territory, country income level (World Bank Index (Fantom and Serajuddin 2016)), results standardization, results’ level of aggregation, all-cause excess mortality, and cause-specific mortality (values and unit of measure).
When extracting cause-specific mortality data, we reported confidence intervals if available, if not, we reported the percentage variation and the respective p-value and if the p-value was not included, we reported the estimates. For the sake of completeness, we reported all the results (Tables 1, 2, 3, and 4 and supplemental material), but we limited the discussion only to those studies that reported statistical significance.
Quality assessment
The evaluation of the included studies was performed using the Newcastle–Ottawa Quality Assessment Scale (NOS) developed by Wells and colleagues (Wells et al. 2022). NOS contains eight items within three domains and the total maximum score is 9. A study with a score from 7–9 has fair to good quality, 4–6 high risk, and 0–3 very high risk of bias.
Results
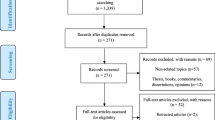
A total of 705 were retrieved from MEDLINE, 2380 from Scopus and 379 articles were retrieved from ProQuest. After merging and duplicates removal, 2413 articles were screened. Out of those articles, 1896 were ruled out after title screening. Of the remaining 517 articles, 439 were removed after abstract screening.
A total of 78 articles were included in the full-text review process (Fig. 1). Of these, 56 were excluded after the full-text screening. We extracted relevant data from the final set of 22 articles (Brant et al. 2020; Fernandes et al. 2021; Décarie and Michaud 2021; Liu et al. 2021; Li et al. 2021; Shoaib et al. 2021; Wu et al. 2021a, b; Al Wahaibi et al. 2021; Wang et al. 2021; Wu et al. 2021a, b; Kontopantelis et al. 2021; Sharma et al. 2021; Faust et al. 2021; Grande et al. 2022; Palacio-Mejía et al. 2022; Gobiņa et al. 2022; Perotti et al. 2022; Jardim et al. 2022; Glei 2022; Orellana and de Souza 2022; Odd et al. 2022; Chen et al. 2022).
Among the 22 articles selected for data extraction, one was published in 2020 (Brant et al. 2020), 12 were published in 2021 (Fernandes et al. 2021; Décarie and Michaud 2021; Liu et al. 2021; Li et al. 2021; Shoaib et al. 2021; Wu et al. 2021a, b; Al Wahaibi et al. 2021; Wang et al. 2021; Wu et al. 2021a, b; Kontopantelis et al. 2021; Sharma et al. 2021; Faust et al. 2021) and nine were published in 2022 (Grande et al. 2022; Palacio-Mejía et al. 2022; Gobiņa et al. 2022; Perotti et al. 2022; Jardim et al. 2022; Glei 2022; Orellana and de Souza 2022; Odd et al. 2022; Chen et al. 2022). All the included studies used data from official governmental sources to perform their analysis. Studies’ characteristics are reported in Table S1.
Out of the nine countries investigated by the included studies, two of them (Brazil and Mexico) are classified as upper-middle-income by the World Bank classification system, while the others are classified as high-income (Canada, China, Italy, Latvia, Oman, United Kingdom, and United States of America). The studies included in our review have study settings with heterogeneous granularity. For instance, studies investigate mortality at a city level (Brant et al. 2020; Fernandes et al. 2021; Liu et al. 2021; Li et al. 2021; Perotti et al. 2022), subnational region/state level (Décarie and Michaud 2021; Liu et al. 2021; Shoaib et al. 2021; Kontopantelis et al. 2021; Sharma et al. 2021; Chen et al. 2022) and country levels (Shoaib et al. 2021; Wu et al. 2021a, b; Al Wahaibi et al. 2021; Wang et al. 2021; Wu et al. 2021a, b; Kontopantelis et al. 2021; Faust et al. 2021; Grande et al. 2022; Palacio-Mejía et al. 2022; Gobiņa et al. 2022; Jardim et al. 2022; Glei 2022; Orellana and de Souza 2022; Odd et al. 2022).
All but three studies analyzed timeframes within the year 2020. All the included studies reported the extensions of the historical data used to estimate the expected deaths. The mean length of the study period was 226.3 ± 149.5 days. The mean length of the historical data used to obtain the expected number of deaths was 5 ± 2 years.
All studies reported the methods used to estimate the expected mortality for the respective study period. The Poisson regression model (n = 7) (Brant et al. 2020; Décarie and Michaud 2021; Li et al. 2021; Shoaib et al. 2021; Sharma et al. 2021; Jardim et al. 2022; Palacio-Mejía et al. 2022) was the most widely employed method, followed by the mean number of deaths of the previous years (n = 4) (Shoaib et al. 2021; Wang et al. 2021; Grande et al. 2022; Perotti et al. 2022), the Farrington surveillance algorithm (n = 3) (Liu et al. 2021; Al Wahaibi et al. 2021: Wu et al. 2021a, b), and the negative binomial regression model (n = 3) (Kontopantelis et al. 2021; Glei 2022; Odd et al. 2022). Other methods included the autoregressive integrated moving average (ARIMA) model (n = 2) (Faust et al. 2021; Chen et al. 2022) and generalized additive modeling (GAM) (n = 2; Gobina et al. 2022; Orellana and de Souza 2022). One study (Fernandes et al. 2021) reported using the 2019 number of deaths as the expected number of deaths of 2020.
Of all included studies, 13 (Fernandes et al. 2021; Li et al. 2021; Shoaib et al. 2021; Wu et al. 2021a, b; Al Wahaibi et al. 2021; Wang et al. 2021; Wu et al. 2021a, b; Kontopantelis et al. 2021; Grande et al. 2022; Perotti et al. 2022; Jardim et al. 2022; Glei 2022; Orellana and de Souza 2022) studies reported stratified results by socio-demographic variables. Specifically, ten studies stratified by sex (Fernandes et al. 2021; Wu et al. 2021a, b; Al Wahaibi et al. 2021; Wang et al. 2021; Wu et al. 2021a, b; Kontopantelis et al. 2021; Grande et al. 2022; Perotti et al. 2022; Glei 2022; Orellana and de Souza 2022), ten by age (Fernandes et al. 2021; Wu et al. 2021a, b; Al Wahaibi et al. 2021; Wang et al. 2021; Wu et al. 2021a, b; Kontopantelis et al. 2021; Grande et al. 2022; Perotti et al. 2022; Glei 2022; Orellana and de Souza 2022), two by month (Wang et al. 2021; Faust et al. 2021), two by healthcare setting (Shoaib et al. 2021; Al Wahaibi et al. 2021), one by type of occupation(Li et al. 2021) and one by quintile of deprivation (Kontopantelis et al. 2021). Only six studies (Fernandes et al. 2021; Wang et al. 2021; Grande et al. 2022; Perotti et al. 2022; Glei 2022; Jardim et al. 2022) reported standardized mortality rates.
Cause-specific mortality results were reported using different units of measurement. Specifically, three studies (Brant et al. 2020; Li et al. 2021; Grande et al. 2022) analyzed the percentage change in mortality with respect to the comparison period, seven studies (Décarie and Michaud 2021; Kontopantelis et al. 2021; Sharma et al. 2021; Palacio-Mejía et al. 2022; Gobiņa et al. 2022; Glei 2022; Chen et al. 2022) analyzed the absolute number of excess deaths, two studies (Fernandes et al. 2021; Al Wahaibi et al. 2021) reported the standardized mortality ratio, two studies (Wu et al. 2021a, b) reported both the total number of excess deaths and percentage variation, six studies (Liu et al. 2021; Al Wahaibi et al. 2021; Faust et al. 2021; Perotti et al. 2022; Jardim et al. 2022; Odd et al. 2022) reported the observed-to-expected ratio, and one study (Shoaib et al. 2021) reported the incidence rate ratio.
Of the 22 included studies, 15 report significance and/or confidence intervals (Brant et al. 2020; Fernandes et al. 2021; Liu et al. 2021; Li et al. 2021; Shoaib et al. 2021; Al Wahaibi et al. 2021; Wang et al. 2021; Kontopantelis et al. 2021; Faust et al. 2021; Palacio-Mejía et al. 2022; Gobiņa et al. 2022; Perotti et al. 2022; Jardim et al. 2022; Orellana and de Souza 2022; Odd et al. 2022). Moreover, there was no consensus among the included studies on the ICD-10 codes used to group causes of death.
Cause-specific mortality
Table 1 reports the number of studies which analyzed a specific cause of death, and for each specific cause shows the number of studies which included the statistical significance levels with their results (e.g., 11 out of 16 studies on cardiovascular-specific mortality reported 95% confidence intervals in their estimates).
The most frequently analyzed causes of deaths were cardiovascular diseases (n = 16, Table 2) (Brant et al. 2020; Fernandes et al. 2021; Décarie and Michaud 2021; Liu et al. 2021; Li et al. 2021; Shoaib et al. 2021; Wu et al. 2021a, b; Al Wahaibi et al. 2021; Wang et al. 2021; Wu et al. 2021a, b; Sharma et al. 2021; Gobiņa et al. 2022; Perotti et al. 2022; Jardim et al. 2022; Glei 2022; Chen et al. 2022), followed by cancer (n = 14, Table 3) (Fernandes et al. 2021; Décarie and Michaud 2021; Liu et al. 2021; Li et al. 2021; Wu et al. 2021a, b; Kontopantelis et al. 2021; Grande et al. 2022; Palacio-Mejía et al. 2022; Gobiņa et al. 2022; Perotti et al. 2022; Jardim et al. 2022; Glei 2022; Odd et al. 2022; Chen et al. 2022), diabetes (n = 11, Table 4) (Fernandes et al. 2021; Décarie and Michaud 2021; Liu et al. 2021; Li et al. 2021; Wu et al. 2021a, b; Grande et al. 2022; Palacio-Mejía et al. 2022; Gobiņa et al. 2022; Perotti et al. 2022; Glei 2022; Chen et al. 2022), and suicide (n = 9) (Décarie and Michaud 2021; Liu et al. 2021; Shoaib et al. 2021; Faust et al. 2021; Grande et al. 2022; Palacio-Mejía et al. 2022; Perotti et al. 2022; Glei 2022; Odd et al. 2022). Cerebrovascular and road accident deaths were also frequently investigated (Table 1).
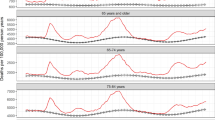
As for cardiovascular mortality (Table 2), the included studies reported heterogeneous patterns of cause-specific mortality in terms of data stratification and trends. For instance, the study by Brant et al. (2020) investigated cardiovascular mortality in six major Brazilian cities and reported changes in mortality ranging from +46.1% (29.5–64.9, 95% CI) in Manaus to −7.1% (−11.9 to−1.9, 95% CI) in Rio de Janeiro. The study by Li et al. (2021) investigated patterns of cardiovascular mortality for different age groups and working/occupation class, and reported changes in mortality ranging from +12.9% (4.6–20.5, 95% CI) in the age class 25–44 years, to −24.4% (−46.5 to 5.3, 95% CI) in the age class < 25 years.
As for cancer mortality (Table 3), the included studies reported heterogenous patterns of cause-specific mortality. Décarie and Michaud (2021) reported a decrease in excess deaths both in British Columbia and in Quebec regions (−45.0 and −570.5 excess deaths respectively), while Liu et al. (2021) reported no significant changes in cancer mortality in Wuhan city, Hubei Region without Wuhan, and China without Hubei region (1.02, 1.08 and 0.99 mortality rate ratios respectively).
Considering deaths for diabetes (Table 4), Décarie and Michaud (2021) reported an increase in excess deaths in British Columbia (29.1), and a decrease in Quebec (−48.1), while Wu et al. (2021a, b) found more homogenous patterns of increased mortality for diabetes in several healthcare settings in England and Wales.
Complete data for other causes of deaths can be found in the supplemental material (Tables S2–S26).
Quality assessment
According to the Newcastle–Ottawa Quality Assessment Scale (Wells et al. 2022) (Table S18), most of the included articles showed a fair quality (n = 15; 68%, score = 7), and seven (32%) of the included articles showed a good quality (score = 8). None of the included studies showed high risk of bias.
Discussion
Main finding of this study
Investigating the true impact of the pandemic on causes of death other than COVID-19 is crucial for public health decision-making and defining priorities. In this study we systematically reviewed the body of literature on the patterns of cause-specific mortality during the COVID-19 pandemic.
The majority of the included studies analyzed study periods within the year 2020, while three of them also investigated 2021. This does not allow us to speculate about the long-term effects of the pandemic, nor on the impact of the vaccination campaign among the included countries. Conceivably, the effects on certain diseases could be delayed. Globally, the World Health Organization reported that 49% of countries experienced disruptions to diabetes services, 31% for cardiovascular disease services and 42% for cancer services due to the COVID-19 crisis (WHO 2020).
Considering that the types of studies were relatively similar (i.e., mainly cohort studies on excess mortality) and above all that the data used originated from national or supranational mortality registries characterized by controls and sufficient data security, the studies’ quality was high (between fair and good). The only substantial difference in the quality of the studies is related to the use of standardized mortality and the choice of controls for the implementation of the statistical models. This highlights how, despite the heterogeneity of the data sources and of the coding of the causes of death, the level of scientific evidence is high.
It should be noted that we could neither perform meta-analyses nor direct comparisons between studies due to the heterogeneity of methodologies and approaches. Specifically, authors investigated different time periods, adopted different methodologies for estimating excess mortality, different coding, and classification of causes of death, and, most importantly, they did not always standardize their results and adopted different approaches in the stratification of the results. Furthermore, despite the large body of literature on all-cause mortality, we found a relatively small number of studies focusing on specific causes of death.
Most of the studies included in this review reported excess all-cause mortality in the respective study periods, apart from Li et al. (2021) Kontopantelis et al. (2021), Glei (2022) and Chen et al. (2022). The scientific evidence accumulated so far confirms what has been reported by most of the studies included in our review, namely that the SARS-CoV-2 pandemic caused a global excess of deaths much greater than what is indicated by reported deaths due to COVID-19 alone (Wang et al. 2022; Glei 2022). The registered reduction of mortality in certain geographical areas and in certain care settings can be mainly explained by the measures adopted to counter the spread of the virus (i.e., social distancing, non-pharmaceutical interventions, mobility reduction, etc.). Notably, a reduction in hospice-related mortality also appears to be a common trend in recent pandemics (Bone et al. 2020; Chen et al. 2006).
Overall, there is still an important knowledge gap on cause-specific mortality patterns during the COVID-19 pandemic. In fact, most of the included studies investigated the causes of deaths that determine the greatest burden of disease in high-income countries (e.g., cardiovascular diseases, cancers, and diabetes). For instance, in the six Brazilian capitals analyzed by Brant et al. (2020), the impact of the pandemic on cardiovascular deaths was noticeable, especially in regions where the health system collapsed, which corresponds to the most socioeconomically deprived. This was also confirmed by Jardim et al. (2022). Li et al. (2021) also found excesses in deaths from cardiovascular diseases in China, particularly during the first wave of COVID-19, with an increase in observed deaths immediately after the start of the pandemic. Despite non-homogeneous results, an important share of the scientific literature reports an increase in cardiovascular diseases mortality during the first phases of the pandemic. Conceivably, the impaired access to healthcare services contributed to the increased cardiovascular mortality (Pines et al. 2021; De Luca et al. 2022; Perotti et al. 2022; Jardim et al. 2022; Glei 2022). Moreover, many cardiovascular diseases are time-dependent. An overwhelmed and fully committed health care system in the fight against respiratory disease caused by the SARS-CoV-2 pandemic partially neglected time-dependent conditions (Fox et al. 2022; Velek et al. 2022).
Although mortality patterns for cardiovascular diseases were very heterogeneous, for chronic diseases — such as oncological diseases — this aspect was even more marked. All the articles included in the review reported different results and addressed different aspects. For instance, opposite results were reported by Kontopantelis et al. (2021) on the one hand, who reported excess deaths for cancer during the first 30 weeks of the pandemic in England and Wales, and by Grande et al. (2022) on the other hand, who instead reported a fair percentage reduction in cancer mortality both overall and by gender during the first wave of the pandemic in Italy. This discrepancy can be explained by the different settings considered and by the different analytical approaches used in the articles. Nonetheless, the impact of the pandemic on the burden of cancer is still unknown and will probably be fully understood only in the next decades (Malagón et al. 2022; Englum et al. 2022). Moreover, the suspension of screening programs in many areas, combined with the reduction of surgical interventions and non-urgent visits, will affect cancer mortality, and increase its burden on societies, in a way which is still difficult to quantify.
When investigating mortality from road accidents, we discovered more homogeneous evidence. Most of the included studies (Liu et al. 2021; Li et al. 2021; Grande et al. 2022; Odd et al. 2022; Perotti et al. 2022) report a significant reduction in the number of road-accident deaths. By confining people at home, interrupting work activities, and reducing road traffic, the frequency of travel- and work-related conditions dropped. This is especially true for the first pandemic wave, when stricter confinement measures were adopted almost worldwide.
What this study adds
Overall, the impact of the pandemic on non-COVID-19 cause-specific deaths has been very heterogeneous, and the analyses conducted so far are not exhaustive. Moreover, the current body of literature is limited in terms of number of studies and geographical location coverage. Specifically, the current evidence is limited to high-income and upper-middle-income countries only. This finding is a direct consequence of the lack of robust data management infrastructures and information systems and lack of reliable and up-to-date data in low-income countries (Lloyd-Sherlock et al. 2021). This lack of data provided by these countries is alarming because those countries are the ones with fewer resources to face the consequences of the pandemic (Bong et al. 2020), having also low supplies of SARS-CoV-2 vaccines (Mathieu et al. 2021). It is of utmost importance to invest in the improvement of infrastructures and information networks in low-income countries, to ensure updated and reliable data that would allow the rapid development of knowledge on which policymakers could base their decisions.
Limitations of the study
This study faced some limitations that must be acknowledged. We were not able to compare the results of the studies, due to the differences in terms of study periods, adopted classification codes, stratification, and lack of standardization. The limited number of studies and the lack of representation of low- and middle-income countries did not make it possible to generalize the results. Moreover, the reduced number of studies that reported statistical significance and/or confidence intervals has further limited our ability to analyze the data. Another limitation is represented by misreporting and misclassification (Sanmarchi et al. 2021), especially for COVID-19 deaths in the early phases of the pandemic. This may have caused, especially in the most affected countries, an altered attribution of causes of death. Also, in this study we considered several subsequent pandemic waves with different variants of the SARS-CoV-2 lineage. Therefore, the impact of the virus on mortality could have been different, mainly due to differences in terms of intrinsic viral characteristics (i.e., pathogenicity and contagiousness). This may have at least partially influenced our findings. However, what we aimed to verify with this systematic review was not only the excess deaths that may have been caused directly by the virus and its pathogenicity, but also the indirect effects caused by the disruption of health services caused by the virus. Finally, when assessing the impact of the COVID-19 pandemic to develop and inform future public health strategies, it is important to analyze other consequences other than excess mortality only. COVID-19 can have long-term effects (Mathieu et al. 2021; Lopez-Leon et al. 2021) that can affect the quality of life of people who have contracted the disease. The emergency period affected people’s mental health (Adams-Prassl et al. 2022; Xie et al. 2022), and these effects will be quantifiable in the future, particularly for the younger generations. Future studies are needed to address these shortcomings.
Conclusions
In this study, we reviewed the available literature to estimate the impact of the COVID-19 pandemic on different causes of death, and to provide a quantitative and qualitative analysis of the phenomenon. We found a high degree of heterogeneity of results and methodologies, which did not allow us to identify unique patterns of cause-specific mortality.
The SARS-CoV-2 pandemic wreaked havoc on society, economy, education, and health. At present, the extent of these effects is not completely known, and it will take time to fully understand them. We believe that it is of fundamental importance to produce novel and up-to-date evidence-based on robust and shared methods. Specifically, given the heterogeneity of the applied methodologies and the cause-specific mortality patterns detected, it would be appropriate to report standardized results (at least by age and sex) for specific macro-categories of death causes.
Reliable scientific evidence is needed by policymakers to make the best decisions in an unprecedented and extremely uncertain historical period, and this is true for the income level of all countries. We advocate for the urgent need to find an international consensus to define uniform conceptual and methodological approaches to establish the true burden of the COVID-19 pandemic on non-COVID-19 mortality.
Data availability
Data extracted from the included articles is available in the supplemental.
References
Adams-Prassl A, Boneva T, Golin M et al (2022) The impact of the coronavirus lockdown on mental health: evidence from the United States. Econ Policy 37(109):139–155. https://doi.org/10.1093/epolic/eiac002
Ahmad FB, Anderson RN (2021) The leading causes of death in the US for 2020. JAMA 325:1829–1830. https://doi.org/10.1001/JAMA.2021.5469
Al Wahaibi A, Al-Maani A, Alyaquobi F et al (2021) Effects of COVID-19 on mortality: a 5-year population-based study in Oman. Int J Infect Dis 104:102–107. https://doi.org/10.1016/j.ijid.2020.12.054
Arolas HPI, Vidal-Alaball J, Gil J et al (2021) Missing diagnoses during the COVID-19 pandemic: a year in review. Int J Environ Res Public Health 18:5335. https://doi.org/10.3390/IJERPH18105335
Aron J, Muellbauer J (2022) Excess mortality versus COVID-19 death rates: a spatial analysis of socioeconomic disparities and political allegiance across U.S. states. Rev Income Wealth 68(2):348–392. https://doi.org/10.1111/ROIW.12570
Banerjee A, Pasea L, Harris S et al (2020) Estimating excess 1-year mortality associated with the COVID-19 pandemic according to underlying conditions and age: a population-based cohort study. Lancet 395:1715–1725. https://doi.org/10.1016/S0140-6736(20)30854-0
Beaney T, Clarke JM, Jain V et al (2020) Excess mortality: the gold standard in measuring the impact of COVID-19 worldwide? J R Soc Med 113:329–334. https://doi.org/10.1177/0141076820956802
Bone AE, Finucane AM, Leniz J et al (2020) Changing patterns of mortality during the COVID-19 pandemic: population-based modelling to understand palliative care implications. Palliat Med 34:1193–1201. https://doi.org/10.1177/0269216320944810
Bong C-L, Brasher C, Chikumba E et al (2020) The COVID-19 pandemic: effects on low- and middle-income countries. Anesth Analg 131:86–92. https://doi.org/10.1213/ANE.0000000000004846
Brant LCC, Nascimento BR, Teixeira RA et al (2020) Excess of cardiovascular deaths during the COVID-19 pandemic in Brazilian capital cities. Heart Br Card Soc 106:1898–1905. https://doi.org/10.1136/HEARTJNL-2020-317663
Chen TJ, Lin MH, Chou LF et al (2006) Hospice utilization during the SARS outbreak in Taiwan. BMC Health Serv Res 6:1–9. https://doi.org/10.1186/1472-6963-6-94/TABLES/5
Chen YH, Stokes AC, Aschmann HE et al (2022) Excess natural-cause deaths in California by cause and setting: March 2020 through February 2021. PNAS Nexus 1(3):pgac079. https://doi.org/10.1093/pnasnexus/pgac079
De Luca G, Algowhary M, Uguz B et al (2022) COVID-19 pandemic, mechanical reperfusion and 30-day mortality in ST elevation myocardial infarction. Heart Br Card Soc 108:458–466. https://doi.org/10.1136/heartjnl-2021-319750
Décarie Y, Michaud PC (2021) Counting the dead: COVID-19 and mortality in Quebec and British Columbia during the first wave. Can Stud Popul 48:139–164. https://doi.org/10.1007/S42650-021-00053-Z
Englum BR, Prasad NK, Lake RE et al (2022) Impact of the COVID-19 pandemic on diagnosis of new cancers: a national multicenter study of the Veterans Affairs Healthcare System. Cancer 128(5):1048–056. https://doi.org/10.1002/cncr.34011
Fantom N, Serajuddin U (2016) The World Bank’s classification of countries by income. World Bank, Washington DC. https://doi.org/10.1596/1813-9450-7528
Faust JS, Du C, Mayes KD et al (2021) Mortality from drug overdoses, homicides, unintentional injuries, motor vehicle crashes, and suicides during the pandemic, March–August 2020. JAMA 326:84–86. https://doi.org/10.1001/JAMA.2021.8012
Fernandes GA, Junior APN, Silva GAE et al (2021) Excess mortality by specific causes of deaths in the city of São Paulo, Brazil, during the COVID-19 pandemic. PLoS One 16:0252238. https://doi.org/10.1371/JOURNAL.PONE.0252238
Fox DK, Waken RJ, Johnson DY et al (2022) Impact of the COVID-19 pandemic on patients without COVID-19 with acute myocardial infarction and heart failure. J Am Heart Assoc 11:22625. https://doi.org/10.1161/JAHA.121.022625
Gibertoni D, Adja KYC, Golinelli D et al (2021) Patterns of COVID-19 related excess mortality in the municipalities of Northern Italy during the first wave of the pandemic. Health Place 67:102508. https://doi.org/10.1016/J.HEALTHPLACE.2021.102508
Glei DA (2022) The US midlife mortality crisis continues: excess cause–specific mortality during 2020. Am J Epidemiol 2022:kwac055. https://doi.org/10.1093/aje/kwac055
Gobiņa I, Avotiņš A, Kojalo U et al (2022) Excess mortality associated with the COVID-19 pandemic in Latvia: a population-level analysis of all-cause and noncommunicable disease deaths in 2020. BMC Public Health 22(1):1109. https://doi.org/10.1186/s12889-022-13491-4
Golinelli D, Campinoti F, Sanmarchi F et al (2021) Patterns of emergency department visits for acute and chronic diseases during the two pandemic waves in Italy. Am J Emerg Med 50:22–26. https://doi.org/10.1016/J.AJEM.2021.07.010
Grande E, Fedeli U, Pappagallo M et al (2022) Variation in cause-specific mortality rates in Italy during the first wave of the COVID-19 pandemic: a study based on nationwide data. Int J Environ Res Public Health 19(2):805. https://doi.org/10.3390/IJERPH19020805
Jardim BC, Migowski A, Corrêa FM, Silva GAE (2022) Covid-19 in Brazil in 2020: impact on deaths from cancer and cardiovascular diseases. Rev Saude Publica 56:22. https://doi.org/10.11606/s1518-8787.2022056004040
Kontis V, Bennett JE, Rashid T et al (2020 2612) Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries. Nat Med 26:1919–1928. https://doi.org/10.1038/s41591-020-1112-0
Kontopantelis E, Mamas MA, Webb RT et al (2021) Excess deaths from COVID-19 and other causes by region, neighbourhood deprivation level and place of death during the first 30 weeks of the pandemic in England and Wales: a retrospective registry study. Lancet Reg Health Eur 7:100144. https://doi.org/10.1016/J.LANEPE.2021.100144
Li L, Hang D, Dong H et al (2021) Temporal dynamic in the impact of COVID- 19 outbreak on cause-specific mortality in Guangzhou, China. BMC Public Health 21. https://doi.org/10.1186/S12889-021-10771-3
Liu J, Zhang L, Yan Y et al (2021) Excess mortality in Wuhan city and other parts of China during the three months of the Covid-19 outbreak: findings from nationwide mortality registries. BMJ 372:n415. https://doi.org/10.1136/BMJ.N415
Lloyd-Sherlock P, Sempe L, McKee M et al (2021) Problems of data availability and quality for COVID-19 and older people in low- and middle-income countries. The Gerontologist 61:141–144. https://doi.org/10.1093/GERONT/GNAA153
Lopez-Leon S, Wegman-Ostrosky T, Perelman C et al (2021) More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep 11:16144. https://doi.org/10.1038/s41598-021-95565-8
Malagón T, Yong JHE, Tope P et al (2022) Predicted long-term impact of COVID-19 pandemic-related care delays on cancer mortality in Canada. Int J Cancer 150:1244–1254. https://doi.org/10.1002/IJC.33884
Mathieu E, Ritchie H, Ortiz-Ospina E et al (2021) A global database of COVID-19 vaccinations. Nat Hum Behav 5:947–953. https://doi.org/10.1038/s41562-021-01122-8
Odd D, Stoianova S, Williams T, Fleming P, Luyt K (2022) Child mortality in England during the first year of the COVID-19 pandemic. Arch Dis Child 107(3):e22. https://doi.org/10.1136/archdischild-2021-323370
Orellana JDY, de Souza MLP (2022) Excess suicides in Brazil: Inequalities according to age groups and regions during the COVID-19 pandemic. Int J Soc Psychiatry 68(5):997–1009. https://doi.org/10.1177/00207640221097826
Page MJ, McKenzie JE, Bossuyt PM, The PRISMA et al (2020) statement: an updated guideline for reporting systematic reviews. BMJ 372:n160. https://doi.org/10.1136/BMJ.N71
Palacio-Mejía LS, Hernández-Ávila JE, Hernández-Ávila M et al (2022) Leading causes of excess mortality in Mexico during the COVID-19 pandemic 2020-2021: a death certificates study in a middle-income country. Lancet Reg Health Am 13:100303. https://doi.org/10.1016/j.lana.2022.100303
Perotti P, Bertuccio P, Cacitti S et al (2022) Impact of the COVID-19 pandemic on total and cause-specific mortality in Pavia, Northern Italy. Int J Environ Res Public Health 19(11):6498. https://doi.org/10.3390/ijerph19116498
Pines JM, Zocchi MS, Black BS et al (2021) The effect of the COVID-19 pandemic on emergency department visits for serious cardiovascular conditions. Am J Emerg Med 47:42–51. https://doi.org/10.1016/J.AJEM.2021.03.004
Sanmarchi F, Golinelli D, Lenzi J et al (2021) Exploring the gap between excess mortality and COVID-19 deaths in 67 countries. JAMA Netw Open 4(7):e2117359. https://doi.org/10.1001/JAMANETWORKOPEN.2021.17359
Santi L, Golinelli D, Tampieri A et al (2021) Non-COVID-19 patients in times of pandemic: emergency department visits, hospitalizations and cause-specific mortality in Northern Italy. PLoS One 16:e0248995. https://doi.org/10.1371/JOURNAL.PONE.0248995
Sharma R, Kuohn LR, Weinberger DM et al (2021) Excess cerebrovascular mortality in the United States during the COVID-19 pandemic. Stroke 52:563–572. https://doi.org/10.1161/STROKEAHA.120.031975
Shoaib A, Spall HGCV, Wu J et al (2021) Substantial decline in hospital admissions for heart failure accompanied by increased community mortality during COVID-19 pandemic. Eur Heart J Qual Care Clin Outcomes 7:378–387. https://doi.org/10.1093/EHJQCCO/QCAB040
Velek P, Splinter MJ, Ikram MK et al (2022) Changes in the diagnosis of stroke and cardiovascular conditions in primary care during the first 2 COVID-19 waves in the Netherlands. Neurology 98:e564–e572. https://doi.org/10.1212/WNL.0000000000013145
Wang J, Zhu J, Yang H et al (2021) Cardiovascular-related deaths at the beginning of the COVID-19 outbreak: a prospective analysis based on the UK Biobank. BMJ Open 11:e046931. https://doi.org/10.1136/BMJOPEN-2020-046931
Wang H, Paulson KR, Pease SA et al (2022) Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. Lancet 11:e046931. https://doi.org/10.1016/S0140-6736(21)02796-3
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. (2022) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses [cited 2022 Aug 30]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm
WHO (2020) COVID-19 significantly impacts health services for noncommunicable diseases. WHO, Geneva. https://www.who.int/news/item/01-06-2020-covid-19-significantly-impacts-health-services-for-noncommunicable-diseases (accessed 29 Mar 2022).
Wu J, Mafham M, Mamas MA et al (2021a) Place and underlying cause of death during the COVID-19 pandemic: retrospective cohort study of 3.5 million deaths in England and Wales, 2014 to 2020. Mayo Clin Proc 96:952–963. https://doi.org/10.1016/J.MAYOCP.2021.02.007
Wu J, Mamas MA, Mohamed MO et al (2021b) Place and causes of acute cardiovascular mortality during the COVID-19 pandemic. Heart Br Card Soc 107:113–119. https://doi.org/10.1136/HEARTJNL-2020-317912
Xie Y, Xu E, Al-Aly Z (2022) Risks of mental health outcomes in people with covid-19: cohort study. BMJ 376:e068993. https://doi.org/10.1136/bmj-2021-068993
Yasin YJ, Grivna M, Abu-Zidan FM (2021) Global impact of COVID-19 pandemic on road traffic collisions. World J Emerg Surg 16(1):51. https://doi.org/10.1186/s13017-021-00395-8
Funding
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors made full and substantial contributions. Emanuele Adorno, Davide Golinelli, and Francesco Sanmarchi contributed to conceptualization, data processing, writing, reviewing, and editing; Francesco Esposito and Francesco De Dominicis contributed to data processing, writing, reviewing and editing; Maria Pia Fantini contributed to reviewing and editing. All authors have given final approval of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not needed
Consent to participate
Not needed
Consent for publication
Not needed
Competing interests
The authors report no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 186 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sanmarchi, F., Esposito, F., Adorno, E. et al. The impact of the SARS-CoV-2 pandemic on cause-specific mortality patterns: a systematic literature review. J Public Health (Berl.) 31, 1847–1865 (2023). https://doi.org/10.1007/s10389-022-01755-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-022-01755-7