Abstract
Background
In recent years, the prevalence of proton pump inhibitor (PPI)-refractory gastroesophageal reflux disease (GERD) has been increasing, posing a clinical obstacle to improving the management of GERD patients. The ability of known predictive factors to explain therapeutic response to PPI remains insufficient. Therefore, we examined whether the addition of early therapeutic response to PPI as an explanatory variable may increase the predictive power for PPI-refractory GERD.
Methods
The severity and therapeutic response of GERD symptoms to PPI were evaluated using the GastroEsophageal Reflux and Dyspepsia Therapeutic Efficacy and Satisfaction Test (GERD-TEST) questionnaire at baseline and at 2 and 4 weeks after treatment. The relevance of the therapeutic effect of PPI at 2 weeks compared to that at 4 weeks was examined in 301 patients with GERD. Independent predictive factors for refractory GERD at 4 weeks of PPI therapy were examined in 182 patients. The effect of various clinical factors, including the early response to PPI, was assessed using multiple regression analysis.
Results
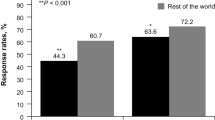
The number of PPI-therapy responders increased significantly with the duration of treatment (p < 0.0001). The response to PPI therapy at 2 weeks was significantly correlated with that at 4 weeks (p < 0.0001). Multiple regression analysis revealed that the therapeutic response to PPI at 2 weeks was by far the strongest predictor of the therapeutic effect at 4 weeks among all clinical factors.
Conclusions
Medication change for PPI-refractory GERD at 2 weeks may be an efficacious therapeutic strategy to improve patients’ quality of life.


Similar content being viewed by others
Change history
08 April 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10388-021-00837-x
References
Emidio S, Daphne A, Ans P, et al. Management of refractory typical GERD symptoms. Nat Rev Gastroentelogy & Hepatology. 2016;13:281–94.
Iwakiri K, Kinoshita Y, Habu Y, et al. Evidence-based clinical practice guidelines for gastroesophageal reflux disease 2015. J Gastroenterol. 2016;51:751–67.
Heading RC, Mönnikes H, Tholen A, et al. Prediction of response to PPI therapy and factors influencing treatment outcome in patients with GORD: a prospective pragmatic trial using pantoprazole. BMC Gastroenterol. 2011;11:52.
Zerbib F, Belhocine K, Simon M, et al. Clinical, but not oesophageal pH-impedance, profiles predict response to proton pump inhibitors in gastro-oesophageal reflux disease. Gut. 2012;61:501–6.
Niu XP, Yu BP, Wang YD, et al. Risk factors for proton pump inhibitor refractoriness in Chinese patients with non-erosive reflux disease. World J Gastroenterol. 2013;19:3124–9.
Hoshihara Y. GERD-gastroesophageal reflux disease endoscopic diagnosis and classification. Rinshou Shoukakinaika. 1996;11:1563–8.
Hongo M. Minimal changes in reflux esophagitis: red ones and white ones. J Gastroenterol. 2006;41(95–9):18.
Nakada K, Matsuhashi N, Iwakiri K, et al. Development and validation of a simple and multifaceted instrument, GERD-TEST, for the clinical evaluation of gastroesophageal reflux and dyspeptic symptoms. World J Gastroenterol. 2017;23:5216–28.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale: Lawrence Erlbaum Associates Publishers; 1988.
Maradey-Romero C, Fass R. New and future drug development for gastroesophageal reflux disease. J Neurogastroenterol Motil. 2014;20:6–16.
Soga T, Matsuura M, Kodama Y, et al. Is a proton pump inhibitor necessary for the treatment of lower-grade reflux esophagitis? J Gastroenterol. 1999;34:435–40.
Iwakiri K, Sakurai Y, Shiino M, et al. A randomized, double-blind study to evaluate the acid-inhibitory effect of vonoprazan (20 mg and 40 mg) in patients with proton-pump inhibitor-resistant erosive esophagitis. Ther Adv Gastroenterol. 2017;10:439–51.
Miwa H, Sasaki M, Furuta T, et al. Efficacy of rabeprazole on heartburn symptom resolution in patients with non-erosive and erosive gastro-oesophageal reflux disease: a multicenter study from Japan. Aliment Pharmacol Ther. 2007;26:69–77.
Chiba N, De Gara CJ, Wilkinson JM, et al. Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a meta-analysis. Gastroenterology. 1997;112:1798–810.
Kinoshita Y, Kobayashi T, Kato M, et al. The pharmacodynamics effect of omeprazole 10 mg and 20 mg once daily in patients with nonerosive reflux disease in Japan. J Gastroenterol. 2006;41:554–61.
Miyazaki H, Igarashi A, Takeuchi T, et al. Vonoprazan versus proton-pump inhibitors for healing gastroesophageal reflux disease: a systematic review. J Gastroenterol Hepatol. 2019;34:1316–28.
Tominaga K, Iwakiri R, Fujimoto K, et al. Rikkunshito improves symptoms in PPI-refractory GERD patients: a prospective, randomized, multicenter trial in Japan. J Gastroenterol. 2012;47:284–92.
Matsuhashi N, Kudo M, Yoshida N, et al. Factors affecting response to proton pump inhibitor therapy in patients with gastroesophageal reflux disease: a multicenter prospective observational study. J Gastroenterol. 2015;50:1173–83.
Talley NJ, Armstrong D, Junghard O, et al. Predictors of treatment response in patients with non-erosive reflux disease. Aliment Pharmacol Ther. 2006;24:371–6.
Bolling-Sternevald E, Lauritsen K, Talley NJ, et al. Is it possible to predict treatment response to a proton pump inhibitor in functional dyspepsia? Aliment Pharmacol Ther. 2003;18:117–24.
Pace F, Annese V, Prada A, et al. Rabeprazole is equivalent to omeprazole in the treatment of erosive gastro-oesophageal reflux disease: a randomised, double-blind, comparative study of rabeprazole and omeprazole 20 mg in acute treatment of reflux oesophagitis, followed by a maintenance open-label, low-dose therapy with rabeprazole. Dig Liver Dis. 2005;37:741–50.
Bytzer P, Morocutti A, Kennerly P, et al. Effect of rabeprazole and omeprazole on the onset of gastro-oesophageal reflux disease symptom relief during the first seven days of treatment. Scand J Gastroenterol. 2006;41:1132–40.
Eggleston A, Katelaris PH, Nandurkar S, et al. Clinical trial: the treatment of gastro-oesophageal reflux disease in primary care–prospective randomized comparison of rabeprazole 20 mg with esomeprazole 20 and 40 mg. Aliment Pharmacol Ther. 2009;29:967–78.
Zheng R-N. Comparative study of omeprazole, lansoprazole, pantoprazole and esomeprazole for symptom relief in patients with reflux esophagitis. World J Gastroenterol. 2009;15:990–5.
Acknowledgements
The authors are grateful to the GERD Society (Osaka, Japan) for their support of this clinical study. We would like to thank the patients and all physicians who participated in this study.
Funding
Financial support for this clinical study was provided by GERD Society (Osaka, Japan).
Author information
Authors and Affiliations
Contributions
The contributors from each institution are listed below: NM: NTT Medical Center Tokyo; MK: Sapporo Hokuyu Hospital; NY and TS: Japanese Red Cross Kyoto Daiichi Hospital; KM and SS: Oita University Faculty of Medicine; MK and KM: Hokkaido University Hospital; TS and JH: Kita Harima Medical Center; NM and KH: Kawasaki Medical School; YN and OH: Kyoto Prefectural University of Medicine; SI: National Hospital Organization Kochi Hospital; HO and YI: Matsushita Memorial Hospital; SM: Tomakomai City Hospital; KF and SO: Shimane University Faculty of Medicine; TO and HM: Hyogo College of Medicine; YF and YK: Osaka City University Graduate School of Medicine; KM and YS: Tenjin Clinic, Medical Corporation Shinai; YI and SO: Shinshu University School of Medicine; TA and YK: Takarazuka Municipal Hospital; HM: Toyama City Hospital; KI, Isshi Gastro-Intestinal Clinic; HS and TC, Kyoto University Hospital; FK and MN, University Hospital, University of the Ryukyus; TS and HF, University of Toyama; KU, Aichi Medical University Medical Clinic; HK and TM, Gunma University Hospital; Noriko Watanabe, National Hospital Organization Mie Chuo Medical Center; FK and KY: Sanuki Municipal Hospital; TI and HF: Shimane Prefectural Central Hospital; TY and YK: Teikyo University School of Medicine; and YN and KK: Tokyo Medical and Dental University.
Corresponding author
Ethics declarations
Ethical Statement
The study was conducted in accordance with the Declaration of Helsinki (sixth revision, 2008), after approval by the ethics committee of each institution or the central ethics committee of Nishi Clinic, Osaka, Japan.
Conflict of interest
Dr. Nobuyuki Matsuhashi received a research grant from Astrazeneca, Takeda Pharm., Eizai. Dr. Katsuhiko Iwakiri received Lecture fees from Takeda Pharmaceutical Co., Ltd., Otsuaka Pharmaceutical Co., Ltd., DAIICHI SANKYO COMPANY, LIMITED, and EA Pharma Co., LTD. Dr. Maiko Ogawa, Dr. Seiji Arihiro, Dr. Takashi Joh, Dr. Kazuhide Higuchi, Dr. Takeshi Kamiya, Dr. Noriaki Manabe, Dr. Kimio Isshi, Dr. Tatsuya Nakada, Dr. Atsushi Hokari, Dr. Masayuki Saruta, Dr. Atsushi Oshio, Dr. Ken Haruma and Dr. Koji Nakada declare that they have no conflict of interest.
Informed consent
Written informed consent was obtained from all enrolled patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ogawa, M., Arihiro, S., Matsuhashi, N. et al. The early therapeutic response at 2 weeks is a crucial predictor of proton pump inhibitor-refractory gastroesophageal reflux disease. Esophagus 18, 398–406 (2021). https://doi.org/10.1007/s10388-020-00792-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10388-020-00792-z