Abstract
Purpose
To study the spatial association of magnetic resonance imaging (MRI) contrast enhancement (CE) areas with visual field defect (VFD) asymmetry in initial cases of optic neuritis (ON) with altitudinal hemianopsia (AH) with reference to nonarteritic anterior ischemic optic neuropathy (NAION) with AH.
Study design
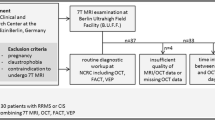
Multicenter, cross-sectional study.
Methods
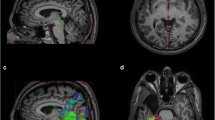
The present study comprised 19 ON patients and 20 NAION patients with AH who underwent orbital contrast fat-suppressed MRI. The signal-to-intensity ratio (SIR) was calculated by dividing the maximum CE of the optic nerve by the mean CE of the cerebral white matter in 11 coronal sections at 3-mm intervals from immediately posterior to the eyeball to the optic chiasm. Sections in ON patients with an SIR exceeding the mean plus 2 standard deviations of the SIR at the corresponding section in the NAION group were considered abnormal. The correlation between upper-to-lower CE asymmetry in the maximum SIR section and VFD counterpart was determined.
Results
The ON group had significantly higher maximum SIR than that of the NAION group (1.77 ± 0.88 vs. 1.25 ± 0.32; P < .01). Seven of the 19 patients had sections with abnormally high CE extending posteriorly beyond the orbital apex. Significant spatial correspondence was observed between CE and VFD asymmetry (rs = 0.563; P = .015) in the ON group but not in the NAION group (rs = − 0. 048; P = .850).
Conclusions
ON patients with AH frequently show CE even in the intracerebral optic nerve, maintaining a moderate structure-function correspondence.








Similar content being viewed by others
References
Toosy AT, Mason DF, Miller DH. Optic neuritis. Lancet Neurol. 2014;13:83–99.
Abel A, McClelland C, Lee MS. Critical review: typical and atypical optic neuritis. Surv Ophthalmol. 2019;64:770–9.
Ishikawa H, Kezuka T, Shikishima K, Yamagami A, Hiraoka M, Chuman H, et al. Epidemiologic and clinical characteristics of optic neuritis in Japan. Ophthalmology. 2019;126:1385–98.
Chen JJ, Tobin WO, Majed M, Jitprapaikulsan J, Fryer JP, Leavitt JA, et al. Prevalence of myelin oligodendrocyte glycoprotein and aquaporin-4-IgG in patients in the Optic Neuritis Treatment Trial. JAMA Ophthalmol. 2018;136:419–22.
Rizzo JF 3rd, Lessell S. Optic neuritis and ischemic optic neuropathy: overlapping clinical profiles. Arch Ophthalmol. 1991;109:1668–72.
Gerling J, Meyer JH, Kommerell G. Visual field defects in optic neuritis and anterior ischemic optic neuropathy: distinctive features. Graefes Arch Clin Exp Ophthalmol. 1998;236:188–92.
Biousse V, Newman NJ. Ischemic optic neuropathies. N Engl J Med. 2015;372:2428–36.
Keltner JL, Johnson CA, Spurr JO, Beck RW. Baseline visual field profile of optic neuritis: the experience of the Optic Neuritis Treatment Trial. Optic Neuritis Study Group. Arch Ophthalmol. 1993;111:231–4.
Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018;17:162–73.
Onodera M, Yama N, Hashimoto M, Shonai T, Aratani K, Takashima H, et al. The signal intensity ratio of the optic nerve to ipsilateral frontal white matter is of value in the diagnosis of acute optic neuritis. Eur Radiol. 2016;26:2640–5.
Youl BD, Turano G, Miller DH, Towell AD, MacManus DG, Moore SG, et al. The pathophysiology of acute optic neuritis: an association of gadolinium leakage with clinical and electrophysiological deficits. Brain. 1991;114:2437–50.
Hood DC, Kardon RH. A framework for comparing structural and functional measures of glaucomatous damage. Prog Retin Eye Res. 2007;26:688–710.
Ueda K, Kanamori A, Akashi A, Kawaka Y, Yamada Y, Nakamura M. Difference in correspondence between visual field defect and inner macular layer thickness measured using three types of spectral-domain OCT instruments. Jpn J Ophthalmol. 2015;59:55–64.
Webb N. The visual system. In: Cocchiarella L, Andersson GBJ, editors. Guides to the evaluation of Permanent Impairment. 5th ed. American Medical Association; 2001. pp. 286–300.
Lee S, Kim SJ, Yu YS, Kim YH, Paek SH, Kim DG, et al. Prognostic factors for visual recovery after transsphenoidal pituitary adenectomy. Br J Neurosurg. 2013;27:425–9.
Horton JC, Greenwood MM, Hubel DH. Non-retinotopic arrangement of fibres in cat optic nerve. Nature. 1979;282:720–2.
Naito J. Retinogeniculate projection fibers in the monkey optic chiasm: a demonstration of the fiber arrangement by means of wheat germ agglutinin conjugated to horseradish peroxidase. J Comp Neurol. 1994;346:559–71.
Horton JC. Wilbrand’s knee: to be or not to be a knee? J Neuroophthalmol. 2020;40(Suppl 1):7–S14.
Hood DC. Does retinal ganglion cell loss precede visual field loss in glaucoma? J Glaucoma. 2019;28:945–51.
Green AJ, Cree BAC. Distinctive retinal nerve fibre layer and vascular changes in neuromyelitis optica following optic neuritis. J Neurol Neurosurg Psychiatry. 2009;80:1002–5.
Nakajima H, Hosokawa T, Sugino M, Kimura F, Sugasawa J, Hanafusa T, et al. Visual field defects of optic neuritis in neuromyelitis optica compared with multiple sclerosis. BMC Neurol. 2010;10:45.
Liu B, Yu Y, Liu W, Deng T, Xiang D. Risk factors for non-arteritic anterior ischemic optic neuropathy: a large scale meta-analysis. Front Med (Lausanne). 2021;8:618353.
Acknowledgements
This study was supported in part by a grant-in-aid (no. 21K09675) from the Japan Society for the Promotion of Science (to M.N.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
H. Ochi, None; T. Kurimoto, None; A. Yamagami, None; K. Goto, None; A. Miki, None; M. Kawai, None; H. Ishikawa, None; M. Matsuzaki, None; M. Kondo, None; Y. Mochizuki, None; A. Kimura, None; T. Maekubo, None; H. Chuman, None; S. Ueki, None; M. Nakamura, None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Makoto Nakamura.
About this article
Cite this article
Ochi, H., Kurimoto, T., Yamagami, A. et al. Structure-function relationship between magnetic resonance imaging lesion areas and visual field defects in initial optic neuritis with altitudinal hemianopsia. Jpn J Ophthalmol 67, 618–627 (2023). https://doi.org/10.1007/s10384-023-01008-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-023-01008-4