Abstract
Purpose
To compare the differences between cycloplegic and noncycloplegic refraction as well as associated factors in grade one students of primary schools, and explore the effectiveness of noncycloplegic refraction for refractive error screening.
Study design
Cross-sectional study.
Methods
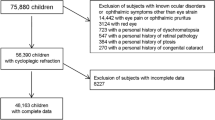
A school-based study of 1856 students was conducted in Lhasa, Tibetan Plateau, China. Cycloplegia was achieved with two drops of 1% cyclopentolate and 1 drop of Mydrin P at a 5-min interval. Autorefraction was performed under both cycloplegic and noncycloplegic conditions. Bland–Altman analysis, receiver operating characteristic curve analysis, univariate and multiple linear regression models were used for analysis.
Results
Of the 1856 children enrolled, 1830 (98.60%) completed all procedures. The average age was 6.83 ± 0.46 years. 965 (52.73%) children were boys and 1737 (94.92%) were Tibetan. Overall, there was a significant difference between cycloplegic and noncycloplegic SE of 0.90 ± 0.76D (P < 0.001). However, the intra-class coefficient correlation (ICC) for cylinder between these two methods was high (ICC = 0.941, 95% CI, 0.935–0.946). Larger differences between cycloplegic and noncycloplegic SE were associated with hyperopic RE and higher cylindrical value (P < 0.001). The prevalence of myopia, emmetropia and hyperopia with and without cycloplegia was (3.93% vs 14.59%), (9.95% vs 45.8%) and (86.21% vs 39.56%), respectively. Myopia, emmetropia and hyperopia based on noncycloplegic refraction was defined as SE ≤ − 0.625D, − 0.625 < SE ≤ 0D, and SE > 0D, respectively.
Conclusions
Lack of cycloplegia leads to underestimation of hyperopia, with overestimation of myopia and emmetropia. Larger hyperopic refraction exhibited greater difference between cycloplegic and noncycloplegic refraction.





Similar content being viewed by others
References
Sun YY, Shi-Fei W, Shi-Ming L, Jian-Ping H, Xiao-Hui Y, Kai C, et al. Cycloplegic refraction by 1% cyclopentolate in young adults: is it the gold standard? The Anyang University Students Eye Study (AUSES)? Br J Ophthalmol. 2018;2018:312199.
Kulp MT, Ying G-S, Huang J, Maguire M, Quinn G, Ciner EB, et al. Accuracy of noncycloplegic retinoscopy, retinomax autorefractor, and suresight vision screener for detecting significant refractive errors. Invest Ophthalmol Vis Sci. 2014;55:1378–85.
Ip JM, Robaei D, Kifley A, Jie JW, Mitchell P. Prevalence of hyperopia and associations with eye findings in 6- and 12-year-olds. Ophthalmology. 2008;115:678–85.
Giordano L, Friedman DS, Repka MX, Katz J, Tielsch JM. Prevalence of refractive error among preschool children in an urban population: the baltimore pediatric eye disease study. Ophthalmology. 2009;116:739–46.
Naidoo KS, Leasher J, Bourne RR, Flaxman SR, Resnikoff S. Global vision impairment and blindness due to uncorrected refractive error, 1990–2010. Optom Vis Sci. 2016;93:227–34.
Kaur G, Koshy J, Thomas S, Kapoor H, Bedi S. Vision screening of school children by teachers as a community based strategy to address the challenges of childhood blindness. J Clin Diagn Res. 2016;10:NC09-NC14.
Kalikivayi V, Naduvilath TJ, Bansal AK, Dandona L. Visual impairment in school children in Southern India. Indian J Ophthalmol. 1997;45:129–34.
Jorge J, Queiros A, Gonzálezméijome J, Fernandes P, Almeida JB, Parafita MA. The influence of cycloplegia in objective refraction. Ophthalmic Physiol Opt. 2010;25:340–5.
Zhao J, Mao J, Luo R, Li F, Pokharel GP, Ellwein LB. Accuracy of noncycloplegic autorefraction in school-age children in China. Optom Vis Sci. 2003;81:49–55.
Choong YF, Chen A-H, Goh P-P. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am J Ophthalmol. 2006;142:68–74.
Morgan IG, Rose KA, Ellwein LB, Group TRESiCS. Is emmetropia the natural endpoint for human refractive development? An analysis of population-based data from the refractive error study in children (RESC). Acta Ophthalmol. 2010;88:877–84.
Morgan IG, Iribarren R, Fotouhi A, Grzybowski A. Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol. 2015;93:581–5. https://doi.org/10.1111/aos.12642.
Chua W-H, Balakrishnan V, Chan Y-H, Tong L, Ling Y, Quah B-L, et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113:2285–91.
Gong Q, Janowski M, Luo M, Wei H, Liu L. Efficacy and adverse effects of atropine in childhood myopia: a meta-analysis. Jama Ophthalmol. 2017;135:624–30.
Wakayama A, Nishina S, Miki A, Utsumi T, Sugasawa J, Hayashi T, et al. Incidence of side effects of topical atropine sulfate and cyclopentolate hydrochloride for cycloplegia in Japanese children: a multicenter study. Jpn J Ophthalmol. 2018;62:531–6.
Hu YY, Feng WJ, Liang LT, Hui W, Wei S, Rong WX, et al. Effect of cycloplegia on the refractive status of children: The Shandong children eye study. PLoS ONE. 2015;2015:10. https://doi.org/10.1371/journal.pone.0117482.
Prabhakar SK, Prathiba KS, Angadhi AP, Kumar SA, Reddy AR, Shamsiya NA. Cycloplegic influence on the accuracy of autorefractometer in myopic and hyperopic children. Nepal J Ophthalmol. 2015;7:148–58.
Loewen N, Barry JC. The use of cycloplegic agents. Results of a 1999 survey of German-speaking centers for pediatric ophthalmology and strabology. Strabismus. 1999;2000(8):91–9.
Fotouhi A, Morgan IG, Iribarren R, Khabazkhoob M, Hashemi H. Validity of noncycloplegic refraction in the assessment of refractive errors: the Tehran Eye Study. Acta Ophthalmol. 2012;90:380–6.
Hashemi H, Khabazkhoob M, Asharlous A, Soroush S, Yekta A, Dadbin N, et al. Cycloplegic autorefraction versus subjective refraction: the Tehran Eye Study. Br J Ophthalmol. 2016;100:1122–7.
Chen W, Fu J, Meng Z, Li L, Su H, Dai W, et al. Lhasa childhood eye study: the rationale, methodology, and baseline data of a 5 year follow-up of school-based cohort study in the Tibetan plateau region of Southwest China. BMC Ophthalmol. 2020;2020:20.
Li S-M, Liu L-R, Li S-Y, Ji Y-Z, Fu J, Wang Y, et al. Design, methodology and baseline data of a school-based cohort study in Central China: the Anyang Childhood Eye Study. Ophthalmic Epidemiol. 2013;20:348–59.
Zhou WJ, Zhang YY, Li H, Wu YF, Xu J, Lv S, et al. Five-year progression of refractive errors and incidence of myopia in school-aged children in Western China. J epidemiol. 2016;26:386–95.
Huynh SC, Kifley A, Rose KA, Morgan I, Heller GZ, Mitchell P. Astigmatism and its components in 6-year-old children. Invest Ophthalmol Vis Sci. 2006;47:55–64.
Hopkins S, Sampson GP, Hendicott P, Lacherez P, Wood JM. Refraction in children: a comparison of two methods of accommodation control. Optom Vis Sci. 2012;89:1734–9.
Funarunart P, Tengtrisorn S, Sangsupawanich P, Siangyai P. Accuracy of non-cycloplegic refraction in primary school children in Southern Thailand. J Med Assoc Thai. 2009;92:806–11.
Lin Z, Vasudevan B, Ciuffreda KJ, Zhou HJ, Mao GY, Wang NL, et al. The difference between cycloplegic and non-cycloplegic autorefraction and its association with progression of refractive error in Beijing urban children. Ophthalmic Physiol Opt. 2017;37:489–97.
Sankaridurg P, He X, Naduvilath T, Lv M, Ho A, Smith E 3rd, et al. Comparison of noncycloplegic and cycloplegic autorefraction in categorizing refractive error data in children. Acta Ophthalmol. 2017;95:e633–40.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J chiropr med. 2016;15:155–63.
Fotedar R, Rochtchina E, Morgan I, Wang JJ, Mitchell P, Rose KA. Necessity of cycloplegia for assessing refractive error in 12-year-old children: a population-based study. Am J Ophthalmol. 2007;144:307–9.
Zhu D, Wang Y, Yang X, Yang D, Pan CW. Pre- and postcycloplegic refractions in children and adolescents. PLoS ONE. 2016;2016:11. https://doi.org/10.1371/journal.
Yingyan MXH, Haidong Z, Lina L, Xiaomei Q, Jianfeng Z. Myopia screening: combining visual acuity and noncycloplegic autorefraction. Optom Vis Sci. 2013;90:1479–85.
Wu JF, Bi HS, Wang SM, Hu YY, Wu H, Sun W, et al. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong Children Eye Study. PLoS ONE. 2013;8:e82763. https://doi.org/10.1371/journal.pone.0082763.
Lian-Hong PLC, Qin L, Ning K, Jing F, Shu Z, Jun X, Wei-Jiang Y, Yan X, Hui SZ-QY. Refractive status and prevalence of refractive errors in suburban school-age children. Int J Med Sci. 2010;7:342–53.
Tideman JWL, Polling JR, Hofman A, Jaddoe VW, Mackenbach JP, Klaver CC. Environmental factors explain socioeconomic prevalence differences in myopia in 6-year-old children. Br J Ophthalmol. 2018;102:243–7.
O’Donoghue L, McClelland JF, Logan NS, Rudnicka AR, Owen CG, Saunders KJ. Refractive error and visual impairment in school children in Northern Ireland. Br J Ophthalmol. 2010;94:1155–9.
Yingyan MXQ, Xiaofeng Z. Age-specific prevalence of visual impairment and refractive error in children aged 3–10 years in Shanghai. China Invest Ophthalmol Vis Sci. 2016;57:6188–96.
He JMZ, Yizhi L. Refractive error and visual impairment in urban children in Southern China. Invest Ophthalmol Vis Sci. 2004;45:793–9.
You QS, Wu LJ, Duan JL, Luo YX, Liu LJ, Li X, et al. Prevalence of myopia in school children in greater Beijing: the Beijing Childhood Eye Study. Acta Ophthalmol. 2014;92:e398–406.
Acknowledgements
The authors are grateful for the support from the Lhasa city government and the Beijing Hoson Foundation for helping organize the survey. The study is supported by Special Topic of Clinical Application Research with Capital Characteristics (Z171100001017066); High-level health technicians in Beijing health system- Backbone of discipline (2015-3-023). I thank Professor Morgan IG, who gave advice on paper writing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
L. Li, None; J. Fu, None; W. Chen, None; Z. Meng, None; Y. Sun, None; H. Su, None; Y. Yao, None; W. Dai, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Jing Fu
About this article
Cite this article
Li, L., Fu, J., Chen, W. et al. Difference of refractive status before and after cycloplegic refraction: the Lhasa Childhood Eye Study. Jpn J Ophthalmol 65, 526–536 (2021). https://doi.org/10.1007/s10384-021-00828-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-021-00828-6