Summary
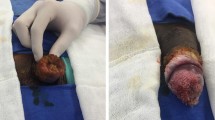
Giant condyloma acuminatum (GCA), alternatively referred to as a Buschke–Löwenstein tumor (BLT), is an uncommon, benign, but locally aggressive form of verrucous carcinoma. The condition usually affects the male population under the age of 50 years; however, there have been rare reports of pediatric cases. Various risk factors such as smoking, diabetes, promiscuous behavior, poor hygiene, immunosuppression, and others are linked to the development of this condition. We present the case of a 26-year-old male patient who came to the dermatology department with primary complaints of 10-year-old verrucous tumor formations located in the perigenital and perianal areas. Serological tests for AIDS, hepatitis B, hepatitis C, Chlamydia trachomatis, and syphilis were negative. The routine blood tests were slightly abnormal. Histological verification of condylomata acuminata of Buschke–Löwenstein was made. Given the sensitive areas, surgery was advised. With several fine undermining scalpel excisions, the lesions in the scrotal and perigenital areas were removed and the dartos muscle was preserved. Electrodissection and shave curettage were not performed. The postoperative period passed without complications and no recurrences in the perigenital area were reported. We believe that our case report represents the first documented surgical approach for scrotal Buschke–Löwenstein tumor using exclusively fine undermining scalpel surgery. A brief literature review of the condition is presented, focusing on the currently available treatment options and highlighting the potential effectiveness of the surgical approach.
Zusammenfassung
Das Condyloma acuminatum giganteum („giant condyloma acuminatum“, GCA), auch Buschke-Löwenstein-Tumor (BLT) genannt, ist eine seltene, gutartige, aber lokal aggressive Form des verrukösen Karzinoms. Die Krankheit betrifft i. d. R. die männliche Bevölkerungsgruppe unter 50 Jahren, es liegen jedoch auch seltene Berichte über Fälle bei Kindern vor. Verschiedene Risikofaktoren wie Rauchen, Diabetes, promiskuitives Verhalten, mangelnde Hygiene, Immunsuppression und andere werden mit der Entstehung dieser Krankheit in Verbindung gebracht. Hier wird der Fall eines 26-jährigen männlichen Patienten vorgestellt, der mit primären Beschwerden über verruköse Tumorbildungen im perigenitalen und perianalen Bereich in die dermatologische Abteilung kam. Serologische Tests für AIDS, Hepatitis B, Hepatitis C, Chlamydia trachomatis und Syphilis waren negativ. Routinemäßige Blutuntersuchungen waren leicht abnormal. Es wurde eine histologische Untersuchung der Buschke-Löwenstein-Condylomata acuminata durchgeführt. Aufgrund der empfindlichen Bereiche wurde eine Operation empfohlen. Mehrere feine unterminierende Skalpellexzisionen wurden durchgeführt, um skrotale und perigenitale Läsionen zu entfernen und die Tunica dartos zu erhalten. Elektrodissektion und Shave-Kürettage wurden nicht durchgeführt. Die postoperative Phase verlief ereignislos, und es wurden keine Rezidive im Perigenitalbereich angegeben. Nach Kenntnis der Autoren handelt es sich bei diesem Fallbericht um den ersten dokumentierten chirurgischen Ansatz zur Behandlung des skrotalen Buschke-Löwenstein-Tumors, bei dem nur eine feine unterminierende Skalpelloperation zum Einsatz kommt. Es wird eine kurze Literaturübersicht über die Erkrankung durchgeführt, wobei der Schwerpunkt auf den derzeit verfügbaren Behandlungsoptionen liegt und die potenzielle Wirksamkeit des chirurgischen Ansatzes hervorgehoben wird.



Similar content being viewed by others
References
Kadouri Y, Nouini Y. La tumeur de Buschke-Löwenstein. Pan Afr Med J. 2020;36:359. https://doi.org/10.11604/pamj.2020.36.359.13292.
Elsayed AG, Sola-Rufai ST, Griswold D, Pacioles T. Verrucous carcinoma arising in a long standing Buschke-Löwenstein tumor. Clin Case Rep. 2019;7(4):836–8. https://doi.org/10.1002/ccr3.2029.
Chao MW, Gibbs P. Squamous cell carcinoma arising in a giant condyloma acuminatum (Buschke-Lowenstein tumour). Asian J Surg. 2005;28(3):238–40. https://doi.org/10.1016/S1015-9584(09)60352-3.
Lévy A, Lebbe C. Prise en charge des tumeurs de Buschke-Löwenstein. Ann Urol. 2006;40(3):175–8. https://doi.org/10.1016/j.anuro.2006.02.002.
Buschke A. Neisser’s Stereokopischer Atlas. New York: Fischer; 1896.
Buschke A, Löwenstein L. Über carcinomähnliche condylomata accuminata des Penis. Klin Wochenschr. 1925;7:1726–8. https://doi.org/10.1007/BF01728480.
Sabuncuoglu MZ, Sabuncuoglu A, Celik G, Sozen I, Cetin R. Moist secret mass; Buschke-Lowenste in tumor: a report of three cases. Case Rep Clin Med. 2014;3:474–8. https://doi.org/10.4236/crcm.2014.38104.
Zidar N, Langner C, Odar K, Hošnjak L, Kamarádová K, Daum O, Pollheimer MJ, Košorok P, Poljak M. Anal verrucous carcinoma is not related to infection with human papillomaviruses and should be distinguished from giant condyloma (Buschke-Löwenstein tumour). Histopathology. 2017;70(6):938–45. https://doi.org/10.1111/his.13158.
Wiedemann A, Diekmann WP, Holtmann G, Kracht H. Report of a case with giant condyloma (Buschke-Löwenstein tumor) localized in the bladder. J Urol. 1995;153(4):1222–4.
Irshad U, Puckett Y. Giant condylomata acuminata of Buschke and Lowenstein. Treasure Island (FL): StatPearls; 2023.
Chu QD, Vezeridis MP, Libbey NP, Wanebo HJ. Giant condyloma acuminatum (Buschke-Lowenstein tumor) of the anorectal and perianal regions. Analysis of 42 cases. Dis Colon Rectum. 1994;37(9):950–7. https://doi.org/10.1007/BF02052606.
Nambudiri VE, Mutyambizi K, Walls AC, Fisher DC, Bleday R, Saavedra AP. Successful treatment of perianal giant condyloma acuminatum in an immunocompromised host with systemic interleukin 2 and topical cidofovir. JAMA Dermatol. 2013;149(9):1068–70. https://doi.org/10.1001/jamadermatol.2013.5160.
Wells M, Robertson S, Lewis F, Dixon MF. Squamous carcinoma arising in a giant peri-anal condyloma associated with human papillomavirus types 6 and 11. Histopathology. 1988;12(3):319–23. https://doi.org/10.1111/j.1365-2559.1988.tb01946.x.
Boda D, Cutoiu A, Bratu D, Bejinariu N, Crutescu R. Buschke-Löwenstein tumors: a series of 7 case reports. Exp Ther Med. 2022;23(6):393. https://doi.org/10.3892/etm.2022.11320.
Bastola S, Halalau A, Kc O, Adhikari A. A gigantic anal mass: Buschke-Löwenstein tumor in a patient with controlled HIV infection with fatal outcome. Case Rep Infect Dis. 2018;2018:7267213. https://doi.org/10.1155/2018/7267213.
Elfatoiki FZ, Hali F, Baghad B, Marnissi F, Chiheb S. Giant perianal condyloma acuminatum in an infant without sexual abuse. Arch Pediatr. 2019;26(8):473–4. https://doi.org/10.1016/j.arcped.2019.09.003.
Leto MD, Santos Júnior GF, Porro AM, Tomimori J. Human papillomavirus infection: etiopathogenesis, molecular biology and clinical manifestations. An Bras Dermatol. 2011;86(2):306–17. https://doi.org/10.1590/s0365-05962011000200014.
Kidd LC, Chaing S, Chipollini J, Giuliano AR, Spiess PE, Sharma P. Relationship between human papillomavirus and penile cancer-implications for prevention and treatment. Transl Androl Urol. 2017;6(5):791–802. https://doi.org/10.21037/tau.2017.06.27.
Zhang D, Gonzalez RS, Feely M, Umrau K, Lee H, Allende DS, Karamchandani DM, Zaleski M, Lin J, Westerhoff M, Zhang X, Alpert L, Liao X, Lai J, Liu X. Clinicopathologic features of Buschke-Löwenstein tumor: a multi-institutional analysis of 38 cases. Virchows Arch. 2020;476(4):543–50. https://doi.org/10.1007/s00428-019-02680-z.
Ingles DJ, Pierre Campbell CM, Messina JA, Stoler MH, Lin HY, Fulp WJ, Abrahamsen M, Sirak BA, O’Keefe MT, Papenfuss M, Gage C, Carvalho da Silva R, Gonzalez Sosa R, Rojas Juarez O, Villa LL, Lazcano Ponce E, Giuliano AR. Human papillomavirus virus (HPV) genotype- and age-specific analyses of external genital lesions among men in the HPV Infection in men (HIM) study. J Infect Dis. 2015;211(7):1060–7. https://doi.org/10.1093/infdis/jiu587.
Cornall AM, Roberts JM, Garland SM, Hillman RJ, Grulich AE, Tabrizi SN. Anal and perianal squamous carcinomas and high-grade intraepithelial lesions exclusively associated with “low-risk” HPV genotypes 6 and 11. Int J Cancer. 2013;133(9):2253–8. https://doi.org/10.1002/ijc.28228.
Antonsson A, Green AC, Mallitt KA, O’Rourke PK, Pandeya N, Pawlita M, Waterboer T, Neale RE. Prevalence and stability of antibodies to 37 human papillomavirus types—a population-based longitudinal study. Virology. 2010;407(1):26–32. https://doi.org/10.1016/j.virol.2010.07.046.
Rahman S, Pierce Campbell CM, Waterboer T, Rollison DE, Ingles DJ, Torres BN, Michel A, Sudenga SL, Pawlita M, Villa LL, Lazcano Ponce E, Borenstein AR, Wang W, Giuliano AR. Seroprevalence of cutaneous human papillomaviruses (HPVs) among men in the multinational HPV Infection in men study. J Gen Virol. 2016;97(12):3291–301. https://doi.org/10.1099/jgv.0.000620.
de Sanjosé S, Bruni L, Alemany L. HPV in genital cancers (at the exception of cervical cancer) and anal cancers. Presse Med. 2014;43(12):e423–8. https://doi.org/10.1016/j.lpm.2014.10.001.
Ahsaini M, Tahiri Y, Tazi MF, Elammari J, Mellas S, Khallouk A, El Fassi MJ, Farih MH, Elfatmi H, Amarti A, Stuurman-Wieringa RE. Verrucous carcinoma arising in an extended giant condyloma acuminatum (Buschke-Löwenstein tumor): a case report and review of the literature. J Med Case Rep. 2013;7:273. https://doi.org/10.1186/1752-1947-7-273.
Jorgaqi E, Jafferany M. Giant condyloma acuminatum (Buschke-Lowenstein tumor): combined treatment with surgery and chemotherapy. Dermatol Ther. 2020;33(1):e13193. https://doi.org/10.1111/dth.13193.
Abbass MA, Valente MA. Premalignant and malignant perianal lesions. Clin Colon Rectal Surg. 2019;32(5):386–93. https://doi.org/10.1055/s-0039-1687835.
Indinnimeo M, Impagnatiello A, D’Ettorre G, Bernardi G, Moschella CM, Gozzo P, Ciardi A, Bangrazi C, De Felice F, Musio D, Tombolini V. Buschke-Löwenstein tumor with squamous cell carcinoma treated with chemo-radiation therapy and local surgical excision: report of three cases. World J Surg Oncol. 2013;11:231. https://doi.org/10.1186/1477-7819-11-231.
Costa Almeida CE, Azevedo J, Botelho I, Vilaça J. Buschke-Löwenstein tumour: a rare and challenging entity. BMJ Case Rep. 2021;14(9):e244192. https://doi.org/10.1136/bcr-2021-244192.
Hicheri J, Jaber K, Dhaoui MR, Youssef S, Bouziani A, Doss N. Giant condyloma (Buschke-Löwenstein tumor). A case report. Acta Dermatovenerol Alp Pannonica Adriat. 2006;15(4):181–3.
Neagu M, Caruntu C, Constantin C, Boda D, Zurac S, Spandidos DA, Tsatsakis AM. Chemically induced skin carcinogenesis: updates in experimental models (review). Oncol Rep. 2016;35(5):2516–28. https://doi.org/10.3892/or.2016.4683.
Tripoli M, Cordova A, Maggì F, Moschella F. Giant condylomata (Buschke-Löwenstein tumours): our case load in surgical treatment and review of the current therapies. Eur Rev Med Pharmacol Sci. 2012;16(6):747–51.
Purzycka-Bohdan D, Szczerkowska-Dobosz A, Swiatecka-Czaj J, Peksa R, Urban M, Szczypior M, Nowicki RJ. Buschke-Löwenstein tumour associated with low-risk human papillomavirus genotypes successfully treated surgically. Postepy Dermatol Alergol. 2019;36(1):112–4. https://doi.org/10.5114/ada.2019.82831.
Papiu HS, Dumnici A, Olariu T, Onita M, Hornung E, Goldis D, Aiordachioae G, Vasca V. Perianal giant condyloma acuminatum (Buschke-Löwenstein tumor). Case report and review of the literature. Chirurgia. 2011;106(4):535–9.
Li AL, Walsh S, McKay DR. Surgical management of a giant condyloma of Buschke-Löwenstein in a patient with Netherton syndrome using the pedicled anterolateral thigh flap—a case report. J Plast Reconstr Aesthet Surg. 2011;64(11):1533–6. https://doi.org/10.1016/j.bjps.2011.03.013.
Spinu D, Rădulescu A, Bratu O, Checheriţă IA, Ranetti AE, Mischianu D. Giant condyloma acuminatum—Buschke-Lowenstein disease—a literature review. Chirurgia. 2014;109(4):445–50.
Afouba AGN, Abessolo HA, Mukam GAM, Noa SAA, Edinga-Melenge BE, Sando Z. Scrotal Buschke-Löwenstein tumor in a teenager: a case study. J Dermatol Res Ther. 2022;5(1):1–5.
Patel AP. Anatomy and physiology of chronic scrotal pain. Transl Androl Urol. 2017;6(1):S51–S6. https://doi.org/10.21037/tau.2017.05.32.
El Khoury A, Jensen JC, Pacioles T. Neoadjuvant chemotherapy and penile conservation in the management of Buschke-Lowenstein tumor, a case report. Urol Case Rep. 2019;29:101111. https://doi.org/10.1016/j.eucr.2019.101111.
Boda D, Negrei C, Arsene AL, Caruntu C, Lupuleasa D, Ion RM. Spectral and photochemical properties of hyperbranched nanostructures based on gardiquimod and TPPS4. Farmacia. 2015;63:218–23.
Iorga L, Marcu R, Diaconu C, Stanescu A, Pantea A, Mischianu D, Surcel M, Bungau S, Constantin T, Boda D, Fekete L, Bratu O. Penile carcinoma and HPV infection (Review). Exp Ther Med. 2020;20(1):91–6. https://doi.org/10.3892/etm.2019.8181.
Kim HG, Kesey JE, Griswold JA. Giant anorectal condyloma acuminatum of Buschke-Löwenstein presents difficult management decisions. J Surg Case Rep. 2018;2018(4):rjy58. https://doi.org/10.1093/jscr/rjy058.
Wu CF, Chen CM, Shen YS, Huang IY, Chen CH, Chen CY, Shieh TY, Sheen MC. Effective eradication of oral verrucous carcinoma with continuous intraarterial infusion chemotherapy. Head Neck. 2008;30(5):611–7. https://doi.org/10.1002/hed.20751.
Fukunaga M, Yokoi K, Miyazawa Y, Harada T, Ushigome S. Penile verrucous carcinoma with anaplastic transformation following radiotherapy. A case report with human papillomavirus typing and flow cytometric DNA studies. Am J Surg Pathol. 1994;18(5):501–5. https://doi.org/10.1097/00000478-199405000-00010.
Combaud V, Verhaeghe C, El Hachem H, Legendre G, Descamps P, Martin L, Bouet PE. Giant condyloma acuminatum of the vulva: successful management with imiquimod. JAAD Case Rep. 2018;4(7):692–4. https://doi.org/10.1016/j.jdcr.2018.04.007.
Heinzerling LM, Kempf W, Kamarashev J, Hafner J, Nestle FO. Treatment of verrucous carcinoma with imiquimod and CO2 laser ablation. Dermatology. 2003;207(1):119–22. https://doi.org/10.1159/000070963.
Dinleyici M, Saracoglu N, Eren M, Kiliç Ö, Ciftci E, Dinleyici EC, Sag C, Kara A. Giant condyloma acuminate due to human papillomavirus type 16 in an infant successfully treated with topical Imiquimod therapy. Dermatol Reports. 2015;7(3):6134. https://doi.org/10.4081/dr.2015.6134.
Masuko T, Fuchigami T, Inadomi T, Inamo Y, Hashimoto K. Effectiveness of imiquimod 5 % cream for treatment of perianal warts in a 28-month-old child. Pediatr Int. 2011;53(5):764–6. https://doi.org/10.1111/j.1442-200X.2010.03277.x.
Lee CN, Hsu CK, Lee JY. Recalcitrant extragenital giant condyloma acuminatum: a need for combination therapy. Dermatol Ther. 2019;32(3):e12867. https://doi.org/10.1111/dth.12867.
Geusau A, Heinz-Peer G, Volc-Platzer B, Stingl G, Kirnbauer R. Regression of deeply infiltrating giant condyloma (Buschke-Löwenstein tumor) following long-term intralesional interferon alfa therapy. Arch Dermatol. 2000;136(6):707–10. https://doi.org/10.1001/archderm.136.6.707.
Bowman IA, Parra A, Arriaga Y. Metastatic giant condyloma acuminata (Buschke-Löwenstein tumor). J Oncol Pract. 2016;12(10):951–3. https://doi.org/10.1200/JOP.2016.013441.
Lukács A, Máté Z, Farkas N, Mikó A, Tenk J, Hegyi P, Németh B, Czumbel LM, Wuttapon S, Kiss I, Gyöngyi Z, Varga G, Rumbus Z, Szabó A. The quadrivalent HPV vaccine is protective against genital warts: a meta-analysis. BMC Public Health. 2020;20(1):691. https://doi.org/10.1186/s12889-020-08753-y.
Deshmukh A, Gulanikar A, Pathrikar S, Pawar SS. Buschke-Lowenstein tumor treated with intralesional measles, mumps, and rubella vaccine. Indian J Sex Transm Dis. 2022;43(1):94–6. https://doi.org/10.4103/ijstd.ijstd_97_20.
Hu Y, Lu Y, Qi X, Chen X, Liu K, Zhou X, Yang Y, Mao Z, Wu Z, Hu Y. Clinical efficacy of paiteling in the treatment of condyloma acuminatum infected with different subtypes of HPV. Dermatol Ther. 2019;32(5):e13065. https://doi.org/10.1111/dth.13065.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
S. Kordeva, I. Pidakev, and G. Tchernev declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kordeva, S., Pidakev, I. & Tchernev, G. Fine scalpel surgery: preserving the dartos muscle in a patient with scrotal and perigenital giant Buschke–Löwenstein tumors. Wien Med Wochenschr (2024). https://doi.org/10.1007/s10354-024-01039-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10354-024-01039-7