Summary
Background
Gastric cancer is one of the most common diseases in Japan, and surgery for gastric cancer is conducted in many general hospitals. However, there has been little investigation of the differences between institutions in terms of postoperative results in gastric cancer patients. This study aimed to compare the quality of treatment for gastric cancer between university hospital and general hospital.
Methods
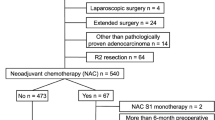
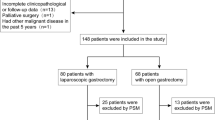
We previously performed a multicenter trial in patients with stage II or III gastric cancer who underwent curative surgery followed by adjuvant S-1 chemotherapy. We selected 39 patients with similar backgrounds from this cohort: 16 from the Tottori University Hospital and 23 from a general hospital (Tottori Prefectural Central Hospital). Quality of surgery, postoperative patient nutrition and immunity, relapse-free survival, and overall survival were compared between the two groups.
Results
Operation time was significantly longer, but postoperative hospital stay was significantly shorter in the university group. Postoperative neutrophil/lymphocyte ratio and prognostic nutritional index improved significantly in the university group but remained unchanged in the general-hospital group. Relapse-free survival and overall survival both were better in the university group compared with the general-hospital group, although the difference in relapse-free survival was not significant.
Conclusions
Surgery and follow-up for advanced gastric cancer should be conducted by trained surgeons and gastric cancer specialists.


Similar content being viewed by others
References
Sierzega M, Kolodziejczyk P, Kulig J, Polish Gastric Cancer Study Group. Impact of anastomotic leakage on long-term survival after total gastrectomy for carcinoma of the stomach. Br J Surg. 2010;97(7):1035–42.
Kubota T, Hiki N, Sano T, et al. Prognostic significance of complications after curative surgery for gastric cancer. Ann Surg Oncol. 2014;21(3):891–8.
Relles DM, Burkhart RA, Pucci MJ, et al. Does resident experience affect outcomes in complex abdominal surgery? Pancreaticoduodenectomy as an example. J Gastrointest Surg. 2014;18(2):279–85.
Lau K, Salami A, Barden G, et al. The effect of a regional hepatopancreaticobiliary surgical program on clinical volume, quality of cancer care, and outcomes in the veterans affairs system. JAMA Surg. 2014;149(11):1153–61. doi:10.1001/jamasurg.2014.1711.
Sakuramoto S, Sasako M, Yamaguchi T, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007;357:1810–20.
Tatebe S, Tsujitani S, Nakamura S, et al. Feasibility study of alternate-day S-1 as adjuvant chemotherapy for gastric cancer: a randomized controlled trial. Gastric Cancer. 2014;17:508–13.
Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M. The baseline ratio of neutrophils to lymphocytes is associated with patient prognosis in advanced gastric cancer. Oncology. 2007;73:215–20.
Ubkata H, Motohashi G, Tabuchi T, Nagata H, Konishi S, Tabuchi T. Evaluation of interferon-γ/interleukin-4 ratio and neutrophil/lymphocyte ratio as prognostic indicators in gastric cancer patients. J Surg Oncol. 2010;102:742–7.
Nozoe T, Kohno M, Iguchi T, et al. The prognostic nutritional index can be a prognostic indicator in colorectal carcinoma. Surg Today. 2012;42:532–5.
Maeda K, Shibutani M, Otani H, et al. Low nutritional prognostic index correlates with poor survival in patients with stage IV colorectal cancer following palliative resection of the primary tumor. World J Surg. 2014;38:1217–22.
Yamada T, Hayashi T, Aoyama T, et al. Feasibility of enhanced recovery after surgery in gastric surgery: a retrospective study. BMC Surg. 2014;14:41. doi:10.1186/1471-2482-14–41.
Low DE. Evolution in surgical management of esophageal cancer. Dig Dis. 2013;31(1):21–9.
Hsu PK, Chen HS, Wu SC, et al. Impact of hospital volume on long-term survival after resection for oesophageal cancer: a population-based study in Taiwan. Eur J Cardiothorac Surg. 2014;46(6):e127–35.
Ravaioli M, Pinna AD, Francioni G, et al. A partnership model between high- and low-volume hospitals to improve results in hepatobiliary pancreatic surgery. Ann Surg. 2014;260(5):871–7.
Liu C, Lu Y, Jun Z, et al. Impact of total retrieved lymph nodes on staging and survival of patients with gastric cancer invading the subserosa. Surg Oncol. 2009;18(4):379–84.
Sasako M, Saka M, Fukagawa T, Katai H, Sano T. Surgical treatment of advanced gastric cancer: Japanese perspective. Dig Surg. 2007;24:101–7.
Ligthart-Melis GC, Weijs PJ, te Boveldt ND, et al. Dietician-delivered intensive nutritional support is associated with a decrease in severe postoperative complications after surgery in patients with esophageal cancer. Dis Esophagus. 2013;26(6):587–93.
Poulsen GM, Pedersen LL, Østerlind K, Bæksgaard L, Andersen JR. Randomized trial of the effects of individual nutritional counseling in cancer patients. Clin Nutr. 2014;33(5):749–53.
Conflict of interest
Masahide Ikeguchi, Masataka Amisaki, Yuki Murakami, Tomohiro Osaki, and Hiroaki Saito declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ikeguchi, M., Amisaki, M., Murakami, Y. et al. Differences in quality of surgery for advanced gastric cancer between institutions. Eur Surg 47, 20–24 (2015). https://doi.org/10.1007/s10353-015-0295-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10353-015-0295-y