Abstract
Purpose
The blood pressure “error signal” represents the difference between an individual’s mean diastolic blood pressure and the diastolic blood pressure at which 50% of cardiac cycles are associated with a muscle sympathetic nerve activity burst (the “T50”). In this study we evaluated whether T50 and the error signal related to the extent of change in blood pressure during autonomic blockade in young and older women, to study potential differences in sympathetic neural mechanisms regulating blood pressure before and after menopause.
Methods
We measured muscle sympathetic nerve activity and blood pressure in 12 premenopausal (25 ± 1 years) and 12 postmenopausal women (61 ± 2 years) before and during complete autonomic blockade with trimethaphan camsylate.
Results
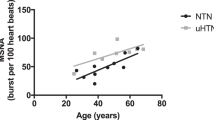
At baseline, young women had a negative error signal (−8 ± 1 versus 2 ± 1 mmHg, p < 0.001; respectively) and lower muscle sympathetic nerve activity (15 ± 1 versus 33 ± 3 bursts/min, p < 0.001; respectively) than older women. The change in diastolic blood pressure after autonomic blockade was associated with baseline T50 in older women (r = −0.725, p = 0.008) but not in young women (r = −0.337, p = 0.29). Women with the most negative error signal had the lowest muscle sympathetic nerve activity in both groups (young: r = 0.886, p < 0.001; older: r = 0.870, p < 0.001).
Conclusions
Our results suggest that there are differences in baroreflex control of muscle sympathetic nerve activity between young and older women, using the T50 and error signal analysis. This approach provides further information on autonomic control of blood pressure in women.





Similar content being viewed by others
References
Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, Horan MJ, Labarthe D (1995) Prevalence of hypertension in the US adult population. Results from the Third National Health and Nutrition Examination Survey, 1988–1991. Hypertension 25(3):305–313
Narkiewicz K, Phillips BG, Kato M, Hering D, Bieniaszewski L, Somers VK (2005) Gender-selective interaction between aging, blood pressure, and sympathetic nerve activity. Hypertension 45(4):522–525
Mercuro G, Podda A, Pitzalis L, Zoncu S, Mascia M, Melis GB, Rosano GM (2000) Evidence of a role of endogenous estrogen in the modulation of autonomic nervous system. Am J Cardiol 85(6):787–789
Hart EC, Charkoudian N, Wallin BG, Curry TB, Eisenach J, Joyner MJ (2011) Sex and ageing differences in resting arterial pressure regulation: the role of the beta-adrenergic receptors. J Physiol 589(Pt 21):5285–5297
Saleh MC, Connell BJ, Saleh TM (2000) Medullary and intrathecal injections of 17 beta-estradiol in male rats. Brain Res 867(1–2):200–209
Saleh TM, Connell BJ (2000) 17 beta-estradiol modulates baroreflex sensitivity and autonomic tone of female rats. J Auton Nerv Syst 80(3):148–161
Minson CT, Halliwill JR, Young TM, Joyner MJ (2000) Influence of the menstrual cycle on sympathetic activity, baroreflex sensitivity, and vascular transduction in young women. Circulation 101(8):862–868
Harvey RE, Barnes JN, Charkoudian N, Curry TB, Eisenach JH, Hart EC, Joyner MJ (2014) Forearm vasodilator responses to a beta-adrenergic receptor agonist in premenopausal and postmenopausal women. Physiol Rep 2(6):1–6
Moreau KL, Donato AJ, Tanaka H, Jones PP, Gates PE, Seals DR (2003) Basal leg blood flow in healthy women is related to age and hormone replacement therapy status. J Physiol 547(Pt 1):309–316
Barnes JN, Hart EC, Curry TB, Nicholson WT, Eisenach JH, Wallin BG, Charkoudian N, Joyner MJ (2014) Aging enhances autonomic support of blood pressure in women. Hypertension 63(2):303–308
Hart EC, Joyner MJ, Wallin BG, Karlsson T, Curry TB, Charkoudian N (2010) Baroreflex control of muscle sympathetic nerve activity: a nonpharmacological measure of baroreflex sensitivity. Am J Physiol Heart Circ Physiol 298(3):H816–H822
Querido JS, Wehrwein EA, Hart EC, Charkoudian N, Henderson WR, Sheel AW (2011) Baroreflex control of muscle sympathetic nerve activity as a mechanism for persistent sympathoexcitation following acute hypoxia in humans. Am J Physiol Regul Integr Comp Physiol 301(6):R1779–R1785
Wehrwein EA, Joyner MJ, Hart EC, Wallin BG, Karlsson T, Charkoudian N (2010) Blood pressure regulation in humans: calculation of an “error signal” in control of sympathetic nerve activity. Hypertension 55(2):264–269
Charkoudian N, Joyner MJ, Johnson CP, Eisenach JH, Dietz NM, Wallin BG (2005) Balance between cardiac output and sympathetic nerve activity in resting humans: role in arterial pressure regulation. J Physiol 568(Pt 1):315–321
Osborn JW, Jacob F, Guzman P (2005) A neural set point for the long-term control of arterial pressure: beyond the arterial baroreceptor reflex. Am J Physiol Regul Integr Comp Physiol 288(4):R846–R855
Osborn JW (2005) Hypothesis: set-points and long-term control of arterial pressure. A theoretical argument for a long-term arterial pressure control system in the brain rather than the kidney. Clin Exp Pharmacol Physiol 32(5–6):384–393
Gracia CR, Sammel MD, Freeman EW, Lin H, Langan E, Kapoor S, Nelson DB (2005) Defining menopause status: creation of a new definition to identify the early changes of the menopausal transition. Menopause 12(2):128–135
Sundlof G, Wallin BG (1977) The variability of muscle nerve sympathetic activity in resting recumbent man. J Physiol 272(2):383–397
Wilkins BW, Hesse C, Sviggum HP, Nicholson WT, Moyer TP, Joyner MJ, Eisenach JH (2007) Alternative to ganglionic blockade with anticholinergic and alpha-2 receptor agents. Clin Auton Res 17(2):77–84
Kienbaum P, Karlssonn T, Sverrisdottir YB, Elam M, Wallin BG (2001) Two sites for modulation of human sympathetic activity by arterial baroreceptors? J Physiol 531(Pt 3):861–869
Wesseling KH, Jansen JR, Settels JJ, Schreuder JJ (1993) Computation of aortic flow from pressure in humans using a nonlinear, three-element model. J Appl Physiol 74(5):2566–2573
Wallin BG, Delius W, Sundlof G (1974) Human muscle nerve sympathetic activity in cardiac arrhythmias. Scand J Clin Lab Invest 34(4):293–300
Saleh TM, Connell BJ (2007) Role of oestrogen in the central regulation of autonomic function. Clin Exp Pharmacol Physiol 34(9):827–832
Christou DD, Jones PP, Jordan J, Diedrich A, Robertson D, Seals DR (2005) Women have lower tonic autonomic support of arterial blood pressure and less effective baroreflex buffering than men. Circulation 111(4):494–498
Barnes JN, Matzek LJ, Charkoudian N, Joyner MJ, Curry TB, Hart EC (2012) Association of cardiac baroreflex sensitivity with blood pressure transients: influence of sex and menopausal status. Front Physiol 3:1–6
Convertino VA (1998) Gender differences in autonomic functions associated with blood pressure regulation. Am J Physiol 275(6 Pt 2):R1909–R1920
Shoemaker JK, Hogeman CS, Khan M, Kimmerly DS, Sinoway LI (2001) Gender affects sympathetic and hemodynamic response to postural stress. Am J Physiol Heart Circ Physiol 281(5):H2028–H2035
Hart EC, Joyner MJ, Wallin BG, Charkoudian N (2012) Sex, ageing and resting blood pressure: gaining insights from the integrated balance of neural and haemodynamic factors. J Physiol 590(Pt 9):2069–2079
Sundlof G, Wallin BG (1978) Human muscle nerve sympathetic activity at rest. Relationship to blood pressure and age. J Physiol 274:621–637
Vaccaro A, Despas F, Delmas C, Lairez O, Lambert E, Lambert G, Labrunee M, Guiraud T, Esler M, Galinier M, Senard JM, Pathak A (2014) Direct evidences for sympathetic hyperactivity and baroreflex impairment in Tako Tsubo cardiopathy. PLoS One 9(3):e93278
Acknowledgements
We thank Shelly Roberts, Sarah Wolhart, Luke Matzek, Alexander Allen, Casey Hines, Pamela Engrav, Nancy Meyer, and Christopher Johnson for their continued assistance throughout the project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Grants
This work was supported by National Institutes of Health grants RR024150 (Center for Translational Science Activities), AG038067 (Jill N. Barnes), HL083947 (B. Gunnar Wallin, Nisha Charkoudian, Michael J. Joyner), American Heart Association grant 2170087 (Emma C. Hart) and Mobility Grant Abroad “José Castillejo” for Young PhD CAS14/00239 (Ana B. Peinado).
Conflict of interest
No conflicts of interest, financial or otherwise, are declared by the authors.
Appendix
Appendix
In the original description of baroreflex threshold diagrams, Wallin et al. [22] found that in subjects with cardiac arrhythmias the wide ranges of blood pressure variations resulted in an S-shaped relationship between occurrence of sympathetic bursts and DBP. To define the relationship statistically probit transformation was used, and then the data points fitted a straight line which was characterized in terms of the T50 point and the slope of the probit line. In contrast, when variations of blood pressure are small (as in sinus rhythm) and data points fall within the linear part of the threshold diagram, linear regression has generally been assumed to provide valid measures of T50 and slope. This approach has been used in several studies. If, however, subjects have high or low resting burst incidence the data points may belong to the curved parts of the S curve. In such cases linear regressions may lead to values for T50 and/or slope that differ from those obtained with the probit method (Fig. 6). Linear and probit analyses of baroreflex threshold curves have not been compared previously in a systematic way. Therefore, to clarify at which burst incidence levels discrepancies between the two methods may occur, we made such comparisons in a group of healthy subjects with burst incidences ranging from low to very high values.
Data points indicating percentage heart beats associated with a sympathetic burst at different diastolic blood pressures (DBP) in subjects with resting burst incidences of 96 (a) and 22 (b). Baroreflex threshold curves based on linear (solid line) and probit (dashed line) analysis. Corresponding T50 values indicated by arrows
The material consists of 51 healthy normotensive subjects (33 men, 18 women), aged 21–71 years, MSNA burst incidence ranged between 16 and 97 bursts/100 heartbeats and burst frequency between 11 and 60 bursts/min. The differences between the results obtained with the two methods are summarized in Fig. 7. For T50 the results are more or less identical at burst incidence between 30 and 70 (Fig. 7a). At lower or higher burst incidences, however, differences start to occur, and for burst incidences above 80 or below 20 the differences are sometimes large. Also for the regression lines (Fig. 7b) differences between slopes are mostly small when burst incidences are between 30 and 70 but occasional exceptions do occur. Outside this range the differences increase and at high or low burst incidences they may be quite large.
Difference between T50 values calculated with linear and probit methodology in subjects with different levels of resting muscle sympathetic nerve activity (MSNA) (a). For three subjects with burst incidences >80 the difference was >25 and therefore data points are not shown. Difference between slopes of threshold diagrams calculated with linear and probit methodology in subjects with different levels of resting MSNA (b)
The results confirm the supposition that for subjects with burst incidences in the medium range, linear and probit analyses of baroreflex threshold curves give similar results. If the subjects have a burst incidence range outside 30 to 70 bursts/100 heartbeats, however, linear analysis may result in erroneous values of T50 and slope (i.e., baroreflex sensitivity); only probit analysis provides reliable measures. Since MSNA burst incidence is known to increase with age [29], probit analysis should be the preferred method in most studies of age-related baroreflex control (like the present one). Special care is important when investigating patient groups with pathological increases of MSNA. A recent example is a study of patients with Takotsubo cardiomyopathy [30] in which linear regression analysis was used at burst incidences above 90; obviously in that case probit analysis would have been an adequate method. In addition, at burst incidences above 90 all data points may fall on the flat part of the S curve and, if so, baroreflex analysis of threshold curves becomes highly unreliable even with probit methodology.
Rights and permissions
About this article
Cite this article
Peinado, A.B., Harvey, R.E., Hart, E.C. et al. Neural control of blood pressure in women: differences according to age. Clin Auton Res 27, 157–165 (2017). https://doi.org/10.1007/s10286-017-0403-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-017-0403-0