Abstract
Improving the quality of digital health care through information and communication technology can mainly contribute to the clinical, social, financial, and economic systems’ success, especially during the COVID-19 pandemic period. The co-design approach, which unleashes the end-user power, can contribute actively in improving the healthcare systems. It deals with understanding the user behaviors, requirements, and motivations through observation, inspection, task analysis, and feedback techniques. Consequently, both the co-design and digital technologies might empower the management of patients’ health and that of their families. The research strategy is based on a systematic literature review and meta-analysis to summarize how the co-design methodologies handled the existing technology-based health systems for their improvement. Based on the findings, we establish the following hypotheses: (i) A user-centered methodology for service implementation might offer a promising tool to enhance the healthcare services quality before they be launched; (ii) Several limitations can affect the co-design approach in digital health, such as a bias for a patients’ group. Efforts have been made to reduce this risk by identifying bias at an early stage, or different groups should be included in the test phase for example; (iii) Use decision-making devices that handle technologies for patient and clinical healthcare solution
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
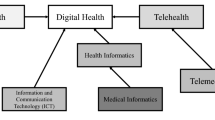
The concept of digital health is defined by different researchers as the improvement of provision and delivery of health services by using information and communication methods in monitoring the patients’ health and well-being ([1,2,3,4]). Obviously, digital health is the adoption of digital communication and information technologies in collecting, sharing and analyzing health data to enhance healthcare services and the patient’s health. A report issued by the World Health Organization (WHO) states that over 130 million individuals require humanitarian aid due to conflicts, disease pandemics, and natural disasters [5]. In most low to middle income earning states around the world, a disease outbreak (i.e., such as in the COVID-19 period) can lead to the crippling of their healthcare structures, which are vital in attaining sustainable development goals in relation to health. Making decisions in such scenario should be informed and rapid, hence the need for new technologies, especially those using Artificial Intelligence (AI), Internet of Things (IoT), computer vision, etc. [6]. Recently, the Food and Drug Administration (FDA) has accepted some of the Digital Health Technologies (DHTs) used in chronic diseases, especially in remote patient monitoring [7]. These technologies are now being integrated with wearables and telemedicine to assist in tracking symptoms, educating patients on health issues, supporting fitness, and helping in the collaborative care coordination, social distancing and disease management [8]. The healthcare landscape is changing tremendously, and there is a greater push for care based on value. On the one hand, the acceptance of DHT by healthcare workers is growing at a high rate, especially in the context of the COVID-19 pandemic. In the other hand, co-design is an approach of “collective creativity” with potential varied stakeholders, who are actively involved throughout the entire development process [9], which is aiding to ensure that this will meet the end-user’s needs and predilections. Whereas, the providers of healthcare services, lack the ability to adapt to changes occurring at run-time.
Currently, research on digital health design methods gained attention from the knowledge that emerged from iterative adaptation and implementation to the responses of the clinicians and patients feedback [10,11,12]. Therefore, in this work, we contribute to the literature, by offering, for the first time, a systematic review of applied co-design techniques in Digital Health Services (DHS). In fact, our contribution aims at referring to the review in order to elicit the practical considerations for healthcare innovation and the actual outcomes of existing innovations when deployed in practice. So, the healthcare innovators, applied health science researchers, clinicians, and quality improvement specialists may refer to this manuscript detailing the DHS design and development in cooperation with healthcare staff and patients together by utilizing AI, IoT, 5G technologies, and smart apps aid patients in the facilitation process of timely and remote access to an appropriate DHS. Furthermore, this paper aims at outlining the guidelines designated to get patients engaged and involved in DHS supporting COVID-19 pandemic combat.
The rest of the paper is organized as follows: Section 2 presents the motivation for our research study. Moreover, it presents some technology solutions as well as the co-design methodologies handling the digital health sector. Section 3 describes the research methodology that we are based on during our systematic review. In Sect. 4, we classify the state-of-the-art of co-design of DHT into information system and automation service solutions. Section 5 presents our findings relating to the literature review. Finally, in Sect. 6, we conclude the manuscript and we present some research directions to support the battle in front of the COVID-19 pandemic.
2 Research study motivation
This section highlights, the technology solutions handling the digital health sector, while addressing the growing need for patient health care, such as interactive voice systems, tracking information systems, robots, and chatbots for e-transmission. Then, it deals with a set of co-designing methodologies handling the user engagement into the digital health sector.
2.1 Combating the COVID-19 pandemic
Since the declaration of the COVID-19 disease as a global pandemic, many researchers have launched various innovations to adopt technology trends within healthcare systems. As illustrated by Google Trends, the interest in digital health has been increasing in the world since January 2020 (see Fig. 1). As shown in Fig. 1, the search about digital health strategies and techniques has grown during the COVID-19 pandemic propagation, whereby all governments and hospital systems around the world want to adopt to replace complex manual operations to support the fight against the COVID-19 pandemic. Lately, the use of digital health applied in most parts of the world for routine visits, and to those who expose a high risk of spreading the disease, digital health helps prevent the disease spread to the health centers. Many digital solutions, such as 3D printing, which helps in decision-making techniques, have been put in place by many health centers such as hospitals, putting much effort into solving personal protective equipment’s inadequacy. Monitoring COVID-19 patient systems allow doctors to monitor COVID-19 patients at their respective homes; This has helped reduce congestion in hospitals. The hospitals are using IT experts to provide technical support to develop a new method to help fight the disease on a short-term basis. The use of a digital method is the most effective way to fight this pandemic. Referring to [13,14,15,16], the governments of different countries should use the following questions to analyze the effects of COVID-19 and develop strategies about the best possible way to handle such a pandemic in the future:
-
1.
How did the COVID-19 pandemic affect user requirements and behaviors?
-
2.
What new care services deployed to handle COVID and non-COVID case should be maintained in normal and abnormal contexts?
-
3.
How should experts expect the current models to handle changes?
-
4.
How do we maintain reliable operations to cope with the future pandemics, including a potential decline in COVID-19 in the winter?
In fact, the responses can give solutions to address the accelerated spread as of COVID-19 well as provide innovative digital ideas for the same reason.
2.2 Technology solutions handling digital health sector
Health literacy is the intensity to which people can learn, process, and comprehend fundamental health knowledge and services required in making critical health decisions [17]. Digital health literacy utilizes a similar definition but in relation to technology. Digital health relates to the medium used in delivering the information and how the recipient understands this information. Technology solutions can be utilized in increasing the transparency and access to information, and in improving how patients communicate with their healthcare service providers. Nonetheless, it is important to understand how technology can be used to address health literacy. According to the best practices of improving health knowledge, providing patients with information is not enough ([18, 19]). To ensure effectiveness, technology solutions should not only improve numerical and literacy skills, but they should also improve critical and functional skills. For instance, these technologies should improve shared decision making, improve communication with healthcare service providers, and assist in navigating the healthcare system [20]. Table 1 contains examples and opportunities for various modern and emerging technologies being utilized in the healthcare sector. Artificial Intelligence/Machine Learning (AI/ML) is providing opportunities to improve the healthcare industry [21]. AI/ML can also be applied in improving health systems literacy skills based on the various dimensions of health management such as behavioral, medical, social, and demographic signatures of a person [22]. It can be incorporated into monitoring personality traits and learning preferences to create a dynamic and personalized experience. When using AI/ML, one signature for each patient can be created [23].
In the last 5 years, over $30 billion has been invested in AI by companies such as Microsoft Facebook, and Google, and 90% was allocated to research and development [24]. Since there is a huge interest in such technologies, especially in the healthcare industry, many vendors who claim to be using AI are approaching individual practitioners and hospitals. It is important for buyers to beware since, in most cases, the algorithm used is basic with no implementation of AI. AI can be utilized in the healthcare system since it can handle and optimize large and complicated data sets collected in complex environments. It can also be used in patient care by monitoring the several measures that are subject to change. Most of these steps involve both human interaction and the use of machines making them less deterministic and more stochastic compared to traditional systems. To manage such variations, it is essential to have a centralized and predictive command and control system that can manage large and complicated data sets and continually learn through experience by optimizing the algorithm used to make predictions. Moreover, the human–AI interfaces gains some degree of human-like cognitive, self-executing, and self-adaptive capabilities and autonomy, and generating unexpected outputs that require non-deterministic interactions [11]. A good example is UCHealth in Colorado, which is a health system that delivers a high-quality patient care as well as a high-quality patient experience. It utilizes AI to optimize surgical schedules [25]. The AI system evaluates historical information and the future demand to create predictions in the operating room. Since the inception of this technology, the operating room has recorded an increase in revenue by 4% by increasing block releases by 47%. Additionally, through this system, six more surgeons have been absorbed through optimization and not an increase in staffed operating room block allocations [26]. Recently, the Deep Learning (DL) methods using different medical imaging modalities like Computer Tomography (CT) and X-ray scans might serving for COVID-19 diagnosis [27,28,29].
2.3 Co-design methodologies
Sanders and Stappers used the term “co-design” to refer to collective creativity as it applied in the entire design process [9]. In a co-design approach, diverse experts, like researchers, designers, developers, and expert managers [30] are included directly in the product concept. In many service design projects, co-design is seen as a success key and promotes user satisfaction. In the co-design approach, users are therefore engaged directly throughout the design process of product development. In the healthcare sector, the state-of-the-art approaches aimed at developing and evaluating new service models, with the goal to help people to better experience and engage in their well-being and in the management of their health and that of their families. First, the co-design was intended to increase the value of the consumer. Secondly, it was a vision to stimulate patient families’ creativity, and could encourage their doctors to think more creatively. Briefly, the expected benefits of co-design are to produce innovative ideas as input for new service creation. The goal of organizing co-design is to promote the commitment of patients involved in the service design project to enhance healthcare processes. In order to further support the co-design practices during the service design phase, there is a need for understanding methods and tools to decide on selecting a design strategy to adopt. Several strategies have been proposed to collaborate with end-users to better realize the potential of co-design, such as organizing workshops, focus groups, and/or interviews for patients and their families, gathering patient diary studies, making usability tests and/or cognitive walkthroughs, etc. In fact, one uses such techniques in order to recognize issues, to suggest opportunities for establishing a new design over an existing product. It is worth noting that it is crucial to identify the right people to be involved in measuring, evaluating, and improving experience. End-users can have many roles in a design process, such as user, tester, manager, admin, and designer [31]. Similarly, Pahl et al. [32] specified that the engineering design methods must integrate the priorities of the end-user. As illustrated in Fig. 2, according to Pahl et al., the system design process starts with user needs and involves the user’s engagement. In this context, we summarize: (1) some theoretical underpinnings of engagement techniques and (2) co-designing tools for collecting, analyzing, and presenting patient experience data in DHS in order to optimize the engagement with co-design that impact the clinical outcomes (Table 2).
-
1.
Software-In-the-Loop (SIL): It is much better to build a digital service by using an existing built at a very early stage. In other words, one can improve an existing project where the strategy for implementing the service has already been developed. In addition to the features to be implemented and the internal workflow and assigned roles. Moreover, all end-users’ choices, recommendations, and final experiences have been documented. This initial investment helps to start delivering and growing the service organically, reducing the level of risk taken. The initial phase is to incorporate the collected production code into mathematical simulations, giving engineers useful, practical for analyzing the multipart systems’ detailed plans. Engineers can substitute the costlier systems by analyzing and altering their original test codes using directly connected software to digital systems. The prior testing of the organization software before installing the hardware part fastens then the development process. More efficient software developed to function by SIL enables the detection of a defect at an early stage.
-
2.
Human-In-the-Loop (HIL) is defined as a model that requires human interaction allowing participants to interact with realistic models and attempt to perform as they would in an actual scenario [34]. HIL also refers to the need to have a certain degree of human supervision in fields where errors can cost much more than just profits such as AI and ML based systems.
-
3.
Re-configurable systems: System configurability is the technique used to design a customizable model/system that specifies how different end-users perform similar functions. Therefore, the systems can be personalized after manufacturing to fit a specific users’ requirements to be used more efficiently for them. This method involves a configuration phase followed by an execution phase or have concurrent (partial) configuration and execution [35].
-
4.
Model-in-the-Loop (MiL): In the early stages of MiL testing, not only the environment components, but also the test object are only available as an executable or mathematical model. MiL tests can be run on standard PCs and used for the creation of functions that will not be realized with future software [36].
-
5.
Hardware-in-the-Loop (HaiL) tests differ from previous procedures in that the system to be tested is usually a real component that is integrated into a simulation environment. Individual components of the environment, such as actuators or sensors, may also be available as real hardware if they are difficult to model or their corresponding models are not guaranteed to be real-time capable [37].
-
6.
Personas The Personas technique can be adapted to support the development of human-centered AI applications for AI toolbox. The toolbox contains guidelines and material supporting persona development for AI as well as templates and pictures for persona visualization. It is ready to use and freely available to the international research and development community [11].
-
7.
Cognitive walkthrough (CW) is an efficient method that allows obtaining feedback on an innovative service at early stages, by walking some stakeholders through the new desired experience and asking them to comment. The walkthrough definition just requires some low-fidelity expected interfaces or sketches to support the explanation. Wharton et al. [38], suggested the following CW analysis questions:
-
(a)
Will the user attempt to accomplish the goal of the task (does the user understand that this task is necessary to accomplish the business goal)?
-
(b)
Will the user note that the right feature is available. For example, is the logo exists?
-
(c)
Will the user understand and be aware that the wanted task can be accomplished by the feature?
-
(d)
Does the user get feedback? Will the user know that they have done the right requirement after performing the function?
-
(a)
-
8.
Backcasting Is a method often applied in a workshop form with stakeholders participating. According to J. Holmberg and K. Robert, backcasting is “a method in which the future desired conditions are envisioned and steps are then defined to attain those conditions, rather than taking steps that are merely a continuation of present methods extrapolated into the future” [39]. When problems at hand are complicated and when existing patterns are part of the problems, backcasting is helpful. The planning starts with a determination of the requirements. Then, it consists of collecting insights in a strategic way.
-
9.
Prototyping Digital health prototypes might inform and learn users about the new or redesigned features. If the prototype is robust or mature enough to be deployed, it will be more clear and easy to use. Both patients and clinicians need easy access to the development team via a message module [40].
Involving patients in making-decisions regarding digital technology for health services was through a range of engagements blend participatory action research methods with design thinking to co-design [41,42,43]. In this context, Table 3 illustrates best practices for involving patients in making-decisions’ regarding digital technology for health services. Such practices facilitate the user research interviews through a range of engagements that blend participatory action research methods with design thinking to co-design and somehow this will be connected to the COVID-19 research.
User-based approach adopted from Pahl et al. [32]
3 Research methodology
We introduce our literature survey with systematic review guidelines on co-design in digital health research via using technologies aimed at improving the quality of health care. Indeed, information and communication technology can contribute mainly to the success of the clinical, social, financial, and economic systems. In fact, one shall look for new ways of overcoming the inconsistent processes across the healthcare system such as the duplicated work and the inability to identify cost savings and uncover opportunities for increased revenue. We follow the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) for the state-of-the-art analysis [51]. The systematic review aimed to identify relevant studies focusing on co-designing in the domain of digital health. The review methods were guided by PRISMA (see Fig. 5). PRISMA is an evidence-based list of items that should be reported in systematic reviews and meta-analyses.
3.1 Step 1: Data sources and retrieval
The search was conducted in four electronic databases: Web of Science (WoS), PubMed, Scopus, and EBSCO-SocINDEX, including papers published between 2005 and 2020. Figure 3 shows the numbers of papers retrieved from each database. The key search terms are depicted in Fig. 4. To identify articles, we searched for the explicit use of the free-terms “co-design,” “collaborative design,” “participatory design,” “creative design,” “creative collaboration,” “digital health,” “e-health,” “electronic health,” “technology health,” and “technological health” such as AI, IoT, 5G, Machine learning, and Remote monitoring. Furthermore, in this research study, we were seeking research articles in which articles’ authors obviously recognize their development method as co-design of digital health technologies. However, some research articles were excluded, in case they did not meet the main goal of this paper, and/or were technology-based design solutions for physical health instead of digital health. To reduce the risk of failing to recognize relevant reviews, we performed a manual search of key journals and reference lists in recent reviews and guidelines that were grasped by the initial literature search. An inclusive database search for individual PRISMA was also conducted to define new appraisals/experiments that were published with highly cited in peer-reviewed regarding the sample of task force guidelines and systematic reviews. These database searches, followed the same processes as mentioned above. Each fetched title, keywords, and abstract was reviewed for significance and relevance to this research study and removed duplication, before carrying out full-text screening.
3.2 Step 2: Data collection
The search results returned 139 papers; these papers were distributed between the four databases shown in Fig. 5. The duplicate articles were removed from the data collection and left 103 unique papers. Investigation of the abstracts, titles, and keywords specified 66 papers that did not meet the inclusion criteria described in the next paragraph. The remaining 37 papers were read in full-text, and further 15 papers were excluded. In total, 22 papers were included. Inclusion criteria comprised different types of publications in the selected databases that observed digital health via digital and mobile technologies in substantial ways. According to the WHO [52], digital health is based on four key users, namely (1) Users of health services, including health promotion activities, (2) Healthcare providers who are members delivering health services, (3) Health system, and (4) Resource managers, who are involved in the administration and control of public health systems and data services to support a variety of activities related to data collection, management, use, and exchange. Publications were included if they addressed trending technologies in the health sector, including AI/machine learning, IoT, Apps, and Remote monitoring. Some publications were excluded if the main ideas were mentioned and discussed only as examples or widespread of a general discussion of digital health or technologies and in passing.
3.3 Step 3: Data analysis and results synthesis
The collected data were analyzed manually and a meta-analysis was carried out by authors’ observations based on the flowchart process of PRISMA (see Fig. 5). Our principal analysis aimed to explore (i) the effect of digital health on varied stakeholders (patients, providers, and medical and paramedical staff in the health sector), (ii) the effect of four main categories of digital health via trending technologies based on co-design tools/methods complexity, and (iii) how the recently co-design methodologies handle existing health systems and technologies in order to innovate for their improvement and consequently pave a pathway for success versus the COVID-19 pandemic. The objective of our secondary analysis was to identify the impact of the use of the health digitization methods for regular low acuity visits or high-risk patients who need to avoid exposure crowded and contagious clinical sites. The authors have discussed the findings iteratively, disclosing the association between each digital health issue and co-design methodologies via using technologies. Further details about data results are presented and synthesized in the discussion section.
4 Literature survey results
This systematic review has certain limitations. In fact, it was designed and built based on four restricted electronic databases. We did not consider “Gray literature,” which might offer pertinent material and information from international health organizations (i.e., WHO, Global Forum for Health Research, Foundation for Innovative New Diagnostic) and non-governmental organizations (i.e., Save the Children U.K., FDA, International Crisis Group, etc.). Moreover, the news media and social media networks were not been reviewed. A further limitation was that many papers were qualitative and addressed personal perspectives as opposed to empirical studies. Such studies should be considered to better understand these dimensions, which could influence the authors’ point views by the selection of papers. Therefore, such restrictions are inherent to this kind of research and caution is needed in generalizing the findings (see Sect. 5).
4.1 Co-design for DHT at a glance: a reflection on the literature
According to the WHO [53], healthcare and public health policy should be adjusted in regard to how they are designed and delivered to do things differently and come up with new ideas. Therefore, the idea of the “digitally engaged patient” serves as a good place to start. Digitally engaged patient is a term used by Lupton [54] to describe “lay people that are ideally willing to seek relevant health and medical information actively, engage in their own health care and take up behaviors that preserve and maintain good health, in the attempt to shift burden of such responsibilities from the state to the individual.” Moreover, Greenhalgh et al. [55] encouraged people to freely engage in self-care activities utilizing digital health technologies in order to enhance their productivity, pleasure, and health. Related to Urban [56], older persons are increasingly using heart rate trackers, which were initially made for the aim of maximizing physical exercise, to keep track of their bodies’ activities and performance. As a result, the principles embodied in digital health technologies urge the user to become a “patient who is digitally engaged” [57]. These studies concluded that the co-designed ideas of community hub digital health interventions and digital video consultations could reduce, rather than intensify, health and well-being difficulties in the community. The idea is based on entailing the participation of stakeholders and end-users in various stages of the development cycle of a solution or service using specific techniques (i.e., interviews, surveys, focus groups, brainstorming sessions, co-creation workshops, iterative designs, etc.). In this context and based on [58, 59], a wide range of various researches are currently available and function for digital health care, we will detail, as shown in Table 4. The main aspects that deal with the co-design principles include:
-
Establishing co-creation There exists a group that helps coordinate contributions by different partners;
-
Engaging the stakeholders There exists a group of providers that facilitates induction within the context of their work;
-
Offering open data Working with a user-friendly interface for inputting data by participants;
-
Sustaining the software or service Identifying stakeholders who are able to sustain and improve the services.
As illustrated in Table 4, several proposals dealt only with the principle of engaging the stakeholders, such as [60,61,62,63]. BlueStar [60] was the first smartphone application in the United States to receive approval from the Food and Drugs Administration to care patients with diabetes mellitus. It investigates the individual digital health needs through a focus group discussion. Similarly, Koyama et al. [61], suggested and built a system, which through a remote had the ability to communicate using videos, images and voice notes, auto-uploading essential data and referencing and finally, drip infusion control. The proposed system was based on engaging the stakeholders through distributing a set of open-ended questions. Lowry et al. [62] adopted the health record systems in hospitals. Their proposal highlighted the importance of the users’ interactions, particularly they may be mainly for pediatric care. It is essential to consider the recommendations concerning identification, vaccination, newborn care, and radiography. Experts in various relevant fields provided a critical review via engaging all stakeholders. Andersen [63] developed a mobile and a web app that ensured proper coordination and communication between the medical professionals and the patients. The App has enabled cardiac patients to access the feedback from their most convenient places, even while traveling. Andersen collaborated with a combination of professionals in various fields who help to develop a digital platform while focusing on establishing co-creation principles (see Table 4). Similarly and with COVID-19 pandemic propagation, Otoom et al. [22] focused also on the engagement of stakeholders, establishing co-creation as well as the offering open data, by developing a system that contains sensors detecting the temperature, audio motion of the heart, and oxygen sensors to help detect symptoms of COVID-19. While other researches like [64, 65] were focused on establishing co-creation, engaging the stakeholders, and sustaining the software or service (illustrated in Table 4).
Kakkar et al. [66] combined cloud and IoT technology to find a healthcare service for children. Considering that specific child faces issues to express their needs, the authors proposed a model where they use wearable IoT devices to detect the blood pressure and heart rate. The collected data is transmitted to the parents and their respective registered physicians based on the event triggers. Pervasive monitoring of health data might collect huge amounts of data, so proposed decision algorithms would raise alert notifications and forward the conditional data for further interactions. End-users collaborate to improve the proposed architecture by offering multiple choice questions to both parents and doctors.
4.2 Applied co-design techniques in DHS: a survey of the literature
Holzinger, in [10], suggested that interactive machine learning (iML) helps interacting with agents and consequently it can optimize their learning behavior (i.e., The author adopted the HIL methodology of co-design approach). He specified that iML can be of particular interest to solve problems in health informatics. For example, the doctor-in-the-loop can help, where human expertise and long-term experience can assist in solving problems which otherwise would remain NP-hard. Therefore, the author emphasized that successful application of machine learning for health informatics requires the effort of experts from seven different disciplines including data science, machine learning algorithms, graph theory/network science, computational topology, entropy, data visualization and visual analytics, and privacy, data protection, safety, and security. The authors, in [12], presented a co-design framework for healthcare innovation, which is divided into seven steps within three stages: (1) pre-design including the contextual inquiry and preparation and training; (2) co-design consisting in framing the issue, generative design and sharing ideas; and (3) post-design comporting the data analysis and requirements translation. They used Personas to support the co-designing care interventions within the health applications. The aim of the work described in [65] was to develop a prototype of game-based eHealth intervention to address the psychological needs of young people with long-term health conditions in New Zealand. The game was based on the principles of cognitive behavior therapy (CBT), where during the first phase of the study, up to 48 young people were invited to participate in a 3-stage series of co-design workshops. In the second phase of the study, a further 20 young people were recruited to evaluate its acceptability, usability, and preliminary efficacy. Georgsson et al. [67] suggested an improved Cognitive Walkthrough (CW) approach for starting validation with a Think Aloud protocol (TA) to evaluate the effectiveness, efficiency, and user acceptance in a case study of diabetes patient users using a mobile Health (mHealth) self-management application. Indeed, the TA protocol is a tool used in product design and development to collect data in usability tests when involving participants thinking as they are performing a set of specified functions. Diabetes patients can monitor blood sugar levels, insulin, food, and physical functions using the mHealth application. The mHealth app uses a Bluetooth network to transmit data related to sugar levels in the blood to the glucometer or manually entered. The app displays the results in a graphical presentation, allowing the patient to critically analyze the diet’s conditions and make the proper decision. The feedback is reported back by the display of some coolers, for example the red shows that the blood sugar is below the required level, green indicates normal level while the yellow shows that the blood level is above the required level. The TA protocol is used for user testing. Thus, users may complete a set of representative tasks during their interactions when verbalizing their thoughts. Recent research on COVID-19 suggested that CT imaging might be useful to assess disease progression in addition to diagnosis the disease. Brown et al. [64] proposed a co-design approach to create a DHT service such as Mobile location-based service for people with dementia to support their everyday activities. In this study, the authors, first, set out to understand the experiences of people living with dementia and their careers using semi-structured interviews. Secondly, they followed a systematic review process (i.e., systematic review guidelines and steps) in order to support the patients’ participation when designing digital health services.
5 Discussion and research findings
Our results have implications for policy makers, practitioners, researchers and digital health organizations who want to implement DHTs. Indeed, as illustrated previously, the user-centered design framework provides a robust yet under-used framework for the review of current and potential methods for developing tools for patient usage. Indeed, co-design as a concept is usually utilized to accomplish collective creativity. In addition, the ability to improve the service usability requires to explore variation in stakeholder perspectives with and across disciplines. Thus, the co-design methodology necessitates dynamic design process construction and design tool selection in response to stakeholder perspectives. Moreover, the stakeholders may collaborate around designing, developing, and delivering innovative digital healthcare services to work in real life. Indeed, as depicted in Table 4, clinicians and health organizations’ staff must be convinced of the opportunities to co-design digital health technology tools and to re-configure their workflows as many studies have attempted to use.
-
1.
Mobile Ad-hoc NETworks (MANETs) are prevalent in healthcare monitoring of high blood pressure, high cholesterol levels, and various heart conditions like syncope, third murmurs, atrial fibrillation, etc. The characteristic mobility of the health monitoring devices, as well as the inherently dynamic network topology, can improve health outcomes by providing personalized services to meet patient needs, reducing communication gaps, and improving patient engagement in caregiver care and self-care [68];
-
2.
IoT plays a crucial role in the healthcare sector by using sensors to monitor the condition of a patient and utilizing historical data to understand the health conditions of a patient [66, 69, 70]. Through IoT, computing devices are interconnected, and data can be transferred from one location to another. Additionally, IoT is improving communication by reducing human to human interaction and human to computer interactions. Sensors are utilized in different forms, such as security systems, home appliances, lighting fixtures, thermostats, smart home systems, covering devices, and hospital systems. These devices can also be connected to other systems, such as smartphones and smart speakers. IoT sensors are mainly used in the healthcare industry to manage the flow of patients;
-
3.
Social media in the public health sector is so crucial, because it generates real-time sensitive data. Thus, it can be considered as a sensor for infectious disease monitoring and detection. The different technologies used, obviously, help in improving machine to machine communication, exchange of information, data movement, and data interoperability. Effective use of such technologies has led to a decline in the number of patient visits, hence improving allocations and planning [71] as well as to underlie the co-design methodology. However, several important limitations can affect the co-design approach in digital health, such as bias for a group of patients. According to Nusir et al. [72], efforts to reduce this risk should therefore be made by identifying potential bias in advance, providing standardized procedures, using external sources for task recognition, and involving other researchers in task creation and validation, results coding and interpretation, as well as guideline reviews. When multiple participants are involved in the testing process; Consequently, many tests will be done, this can increase the likelihood of discovering innovations. In other words, it should evaluate the proposed system for different scenarios to be sure that is an effective one. By using decision support apps, disease management can be done outside the hospital easily, and it also empowers patients to optimize their conditions. Nonetheless, the key to the success of them lies in how complex and user-friendly they are for patients. Recently, U.S. Food and Drug Administration (FDA) released a draft covering some critical and significant recommendations concerning the use of patient and clinical decision-making devices [73], such as:
-
Developing approachable and non-harmful designs of devices used;
-
Selecting the most suitable themes and colors of devices;
-
Developing modest and attractive designs of devices;
-
Complying with UI principles which includes, using well recognizable icons, readable and inclusive large fonts, high-quality images while designing the healthcare devices.
-
-
4.
For IoT-based healthcare solutions, there are several enabling technologies:
-
Grid or Cloud Computing may provide ubiquitous access to common resources for performing operations to meet different needs;
-
Big Data can help increase health analysis efficiency and monitoring instruments and systems; this is made possible by dealing with a large amount of medical sensors’ data;
-
Big Data can include huge amounts of essential health data generated from diverse medical sensors and provide tools for increasing the efficiency of relevant health diagnosis and monitoring methods and stages;
-
Doing simple, intuitive, and attractive designs;
-
Networks for short-scale communications (e.g., WPANs, WBANs, WLANs, 6LoWPANs, and WSNs) and large-scale communications (e.g., any kind of cellular network) might be part of the infrastructure of the IoT-based healthcare network;
-
Wearables can achieve patient engagement and consequently, population health improvements can be facilitated;
-
The DL and ML should be the future health technology investments and the healthcare responsibles must deploy to have AI help with clinical decision making and to predict patient outcomes;
-
AI-based algorithms can be developed and used in personal healthcare monitoring. Additionally, in order to better predict disease outbreaks in advance based on logged healthcare data.
-
-
5.
The large-scale adoption of such technologies also presents an enormous and unimagined potential for novel, unforeseen threats. Therefore, all stakeholders - governments, policymakers, and industry - must work with academia to ensure that new technologies are developed with these potential threats in mind and that the security, traceability, transparency, explainability, validity, and verifiability of AI applications in our everyday lives are ensured. It is the responsibility of all stakeholders to ensure the use of trustworthy and ethically reliable AI and to avoid the misuse of AI technologies [74, 75].
Finally, one can conclude, first, the strong relation between the implemented functional and non-functional requirements from presented solutions and the enabling technologies (see Table 2). For example, it is possible to verify that most of the big data platforms handle data management and processing. Cloud computing platforms might handle data access and service management. Second, the most proposed digital technology solutions are concerned with scalability, configurability, extensibility that is mostly offered by big data-based solutions, and interoperability mostly offered by IoT-based solutions. Third, the implementation of such solutions must be done carefully to reduce harms.
6 Conclusion and future directions
The results and observations showed the importance and the limitation of critical and significant recommendations that should be followed by those involved in digital health technology research and management. We concluded that there is a strong relationship between functional and non-functional requirements implementing DHT solutions and these enabling technologies. For instance, mobile apps are designed to promote user flexibility in the domain of health systems and enabling technologies like Cloud Computing, Big data, IoT, AI, networks and wearables. In addition, we noticed that digital health technology research is an extraordinary opportunity to promote an effective change in order to avoid the Infectious transmission diseases (i.e., COVID-19), which are commonly transmissible through direct touch or contact. With the advent of the COVID-19 pandemic, researchers have turned to digital health technologies to help both medical staff and patients track disease transmission and analyze the disease symptoms. In this context, we plan to address the COVID-19 pandemic by developing a novel framework taking into consideration the current digital technologies. Indeed, we aim to conduct research on how to enable healthcare organizations to process social media data in real time and to develop a model that manages the data and can reliably detect COVID-19 disease cases.
References
Mellodge, P., Vendetti, C.: Remotely monitoring a patient’s mobility: a digital health application. IEEE Potentials 30(2), 33–38 (2011)
Deen, M.J.: Information and communications technologies for elderly ubiquitous healthcare in a smart home. Personal Ubiquitous Comput. 19(3), 573–599 (2015)
Magnustulip, R.: The definition of digital health. http://www.healthissocial.com/2015/02/18/the-definition-of-digital-health/, Retrieved 16 Mar 2022 (2015)
Sonnier, P.: The Story of digital health. https://storyofdigitalhealth.com/, Retrieved 02 Apr (2022)
Akbarzada, S., Mackey, T.K.: The Syrian public health and humanitarian crisis: a displacement in global governance? Glob.Public Health. Taylor. 13(7), 914–930 (2018)
Becker, G.G., Hansoti, T.K., Bartels, B., Hayward, S., Hexom, A.S., Lunney, B.J., Marsh, K.M., Osei-Ampofo, R.H., Trehan, M., Chang, I., Levine, J., Anderson, A.C., Balhara, R.E., Becker, K.S., Beyene, O.K., Bills, T., Bloem, C.B., Bonney, C., Bustamante, J., Chan, N.D., Coker, J., Cook, A., Grover, J., Hauswald, E., House, M., Glover, E.J., Jacquet, P., Jenson, G.A., Kearney, A., Koval, A., Koutroulis, K., Kivlehan, I., Lam, S., Mahal, C., Magnus, J., Modi, D., Nicholson, P., Pousson, B., Quao, A., Rybarczyk, N.S.A., Selvam, M., Silvestri, A., Schultz, D., Winders, M., T, W.: Global emergency medicine: a review of the literature from 2016. Acde. Emerg. Med. 24(9), 1150–1160 (2017)
Riaz, M.S., Atreja, A.: Personalized technologies in chronic gastrointestinal disorders: self-monitoring and remote sensor technologies. Clin. Gastroenterol. Hepatol. Elsevier 14(12), 1697–1705 (2016)
Ardito, C., Desolda, G., Lanzilotti, R., Malizia, A., Matera, M., Buono, P., Piccinno, A.: User-defined semantics for the design of iot systems enabling smart interactive experiences. Personal Ubiquitous Comput. 24(6), 781–796 (2020)
Sanders, E.B.-N., Stappers, P.J.: Co-creation and the new landscapes of design. Co Design 4(1), 518 (2008)
Holzinger, A.: Interactive machine learning for health informatics: when do we need the human-in-the-loop? Brain Inf. 3(2), 119–131 (2016)
Holzinger, A., Kargl, M., Kipperer, B., Regitnig, P., Plass, M., Müller, H.: Personas for artificial intelligence (ai) an open source toolbox. IEEE Access 10, 23732–23747 (2022)
Bird, M., McGillion, M., Chambers, E.M., Dix, J., Fajardo, C.J., Gilmour, M., Levesque, K., Lim, A., Mierdel, S., Ouellette, C., Polanski, A.N., Reaume, S.V., Whitmore, C., Carter, N.: A generative co-design framework for healthcare innovation: development and application of an end-user engagement framework. Res. Involv. Engagem. 7(1), 1–12 (2021)
Sheth, J.: Impact of COVID-19 on consumer behavior: Will the old habits return or die? J. Bus. Res. 117, 280–283 (2020)
Sagan, A., Webb, E., Azzopardi-Muscat, N., de la Mata, I., McKee, M., Figueras, J.: Health systems resilience during COVID-19: lessons for building back better. Health policy series. World health organization. Regional Office for Europe, p. 108 (2021)
Liu, Q., Luo, D., Haase, J.E., Guo, Q., Wang, X.Q., Liu, S., Xia, L., Liu, Z., Yang, J., Yang, B.X.: The experiences of health-care providers during the COVID-19 crisis in china: a qualitative study. Lancet Glob. Health 8(6), 790–798 (2020)
Ma, J., Sallis, J.F.: A national strategy for COVID response and pandemic preparedness must address noncommunicable chronic diseases. J. Gen. Intern. Med. 37(11), 2853–2854 (2022)
Parker, R., Ratzan, S.C.: Health literacy: a second decade of distinction for Americans. J. Health Commun. 15(sup2), 20–33 (2010)
Brega, A.G., Freedman, M.A.G., LeBlanc, W.G., Barnard, J., Mabachi, N.M., Cifuentes, M., Albright, K., Weiss, B.D., Brach, C., West, D.R.: Using the health literacy universal precautions toolkit to improve the quality of patient materials. J. Health Commun. 20(sup2), 69–76 (2015)
Cozza, M., Angeli, A., Tonolli, L.: Ubiquitous technologies for older people. Personal Ubiquitous Comput. 21(3), 607–619 (2017)
Dunn, P., Conard, D.: Improving health literacy in patients with chronic conditions: a call to action. Int. J. Cardiol. 273, 249–251 (2018)
Fogel, A.L., Kvedar, J.C.: Artificial intelligence powers digital medicine. Dig. Med. 1(1), 5 (2018)
Otoom, M., Otoum, N., Etoom, Y., Banihani, R., Alzubaidi, M.A.: An iot-based framework for early identification and monitoring of COVID-19 cases. Biomed. Signal Process. Control 62, 102149 (2020)
Topol, E.J.: High-performance medicine: the convergence of human and artificial intelligence. Nat. Med. 25(1), 44–56 (2019)
Bughin, J., Hazan, E., Ramaswamy, S., Chui, M., Allas, T., Dahlstrom, P., Henke, N., Trench, M.: Artificial intelligence: the next digital frontier? In: artificial intelligence: the Next Digital Frontier?, Proceedings of Business (2017)
Lavine, K.: AI in the operating room: How Colorado health systems are harnessing big data to improve care (and save money). Denver Business Journal, Denver Business Journal (2018)
Bini, S.A.: Artificial intelligence, machine learning, deep learning, and cognitive computing: What do these terms mean and how will they impact health care? Artificial intelligence, machine learning, deep learning, and cognitive computing: what do these terms mean and how will they impact health care? J. Arthroplast. 33(8), 2358–2361 (2018)
Chao, H., Fang, X., Zhang, J., Homayounieh, F., Arru, C., Digumarthy, S., Babaei, R., Mobin, H.K., Saba, L., Carriero, A., Falaschi, Z., Pasche, A., Wang, G., Kalra, M., Yan, P.: Integrative analysis for patient outcome prediction. Med. Image Anal. 6, 101844 (2020)
Islam, M.M., Karray, F., Alhajj, R., Zeng, J.: A review on deep learning techniques for the diagnosis of novel coronavirus (COVID-19). IEEE Access 9, 30551–30572 (2021)
Tilborghs, S., Dirks, I., Fidon, L., Willems, S., Eelbode, L., Bertels, J., lsen, B., Brys, A., Dubbeldam, A., Buls, N., Gonidakis, P., Sánchez, S.A., Snoeckx, A., Parizel, P.M., Mey, J.D., Vandermeulen, Vercauteren, T., Robben, D., Smeets, D., Frederik Maes, D., Vandemeulebroucke, J., Suetens, P.: Comparative study of deep learning methods for the automatic segmentation of lung, lesion and lesion type in ct scans of COVID-19 patients. Preprint. ArXiv. 2020;arXiv:2007.10416v1 (2020)
Visser, F.S., Stappers, P.J., Lugt, R.V.D., Sanders, E.B.: Context mapping: experiences from practice. CoDesign 1(2), 119–149 (2005)
Druin, A.: The role of children in the design of new technology. Behav. Inf. Technol. 21(1), 1–25 (2002)
Pahl, G., Beitz, W., Feldhusen, J., Grote, K.H.: Engineering design: a systematic approach. Solid mechanics and its applications, Springer, London (2007)
Morsi, Y.S., Anupam, S., Chandra, P.R.: Optimizing assistive technologies for aging populations. IGI Glob. 494, 494 (2016)
Waibel, A., Stiefelhagen, R., Carlson, R., Casas, J., Kleindienst, J., Lamel, L., Lanz, O., Mostefa, D., Omologo, M., Pianesi, F., Polymenakos, L., Potamianos, G., Soldatos, J., Sutschet, G., Terken, J.: Computers in the Human Interaction Loop, pp. 1071–1116. Springer, Boston (2010)
Teich, J.: Hardware/software codesign: The past, the present, and predicting the future, In: Proceedings of the IEEE 100(Special Centennial Issue), 1411–1430 (2012)
Schauffele, J., Zurawka, T.: Grundlagen, Prozesse. Springer, Methoden und Werkzeuge Effizient Einsetzen. Automotive Software Engineering (2016)
Isermann, R., Schaffnit, J., Sinsel, S.: Hardware-in-the-loop simulation for the design and testing of engine-control systems. Control Eng. Pract. 7(5), 643–653 (1999)
Wharton, C., Rieman, J., Lewis, C., Polson, P..: In: Nielsen, J., Mack, R.L. (eds.) The cognitive walkthrough method: a practitioner’s guide, pp. 105–140. Wiley, Usability inspection methods (1994)
Holmberg, J., Robért, K.H.: Backcasting from non-overlapping sustainability principles: a framework for strategic planning. Int. J. Sustain. Dev. World Ecol. 7, 1–18 (2000)
Arrivillaga, M., Bermúdez, P.C., García-Cifuentes, J.P., Botero, J.: Innovative prototypes for cervical cancer prevention in low-income primary care settings: a human-centered design approach. PLOS ONE 15(8), 0238099 (2020)
Perestelo-Perez, L., Rivero-Santana, A., Alvarez-Perez, Y., Duarte-Díaz, A., Ramos-García, V., Torres-Castaño, A., Abt-Sacks, A., Toledo-Chavarri, A., Alonso-Coello, P., Orrego, C., Serrano-Aguilar, P.: Shared decision-making in Spain in 2022: an updated revision of the current situation. Zeitschrift für Evidenz, Fortbildung und Qualität im Gesundheitswesen 171, 122–128 (2022)
Small, N., Ong, B.N., Lewis, A., Allen, D., Bagshaw, N., Nahar, P., Sanders, C., Hodgson, D., Dehghan, A., Sharp, C., Dixon, W., Lewis, S., Kontopantelis, E., Daker-White, G., Bower, P., Davies, L., Kayesh, H., Spencer, R., McAvoy, A., Boaden, R., Lovell, K., Ainsworth, J., Nowakowska, M., Shepherd, A., Cahoon, P., Hopkins, R., Nenadic, G.: the DEPEND team: co-designing new tools for collecting, analysing and presenting patient experience data in nhs services: working in partnership with patients and carers. Res. Involv. Engagem. 7(1), 85 (2021)
Islind, A.S., Lindroth, T., Lundin, J., Steineck, G.: Co-designing a digital platform with boundary objects: bringing together heterogeneous users in healthcare. Health Technol. 9(4), 425–438 (2019)
Peyrard, E., Chamaret, C.: Designing for all but with whom? three cases of codesign with disabled persons. Technical report (2020)
Lindberg, O.: User research: best practices and methodologies. Xd Ideas. Accessed 28 Oct 2022 (2020). https://xd.adobe.com/ideas/process/user-research/user-research-best-practices-methodologies/
Vindrola-Padros, C., Chisnall, G., Cooper, S.: Carrying out rapid qualitative research during a pandemic: emerging lessons from COVID-19. Qual. Health Res. 30(14), 2192–2204 (2020)
Siang, T.Y.: Brainstorming. Interaction design foundation. Accessed 28 Oct 2022 (2020). https://www.interaction-design.org/literature/topics/brainstorming
DaSilva, J.: A guide to competitive analysis for UX design. Xd Ideas. Accessed 28 Oct 2022 (2020). https://xd.adobe.com/ideas/process/user-research/guide-to-competitive-analysis-ux-design/
Howard, Z., Somerville, M.M.: A comparative study of two design charrettes: implications for codesign and participatory action research. CoDesign 10(1), 46–62 (2014)
George, T.: What is an observational study? Guide and examples. Scribbr. Accessed 28 Oct 2022 (2022). https://www.scribbr.com/methodology/observational-study/
Liberati, A., Altman, D.G., Tetzla, J., Mulrow, C., Gotzsche, P.C., Ioannidis, J.P., Clarke, M., Devereaux, P.J., Kleijnen, J., Moher, D.: The prisma statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 62(10), 1–34 (2009)
WHO: Classification of digital health interventions v1.0: a shared language to describe the uses of digital technology for health. Technical report (2018)
WHO: Innovative care for chronic conditions : building blocks for actions (global report). Non-communicable Diseases and Mental Health Cluster (2002)
Deborah, L.: Digital Health: Critical and Cross-Disciplinary Perspectives. Handbook of Ambient Intelligence and Smart Environments, Routledge Taylor (2017)
Greenhalgh, T., Hinton, L., Finlay, T., Macfarlane, A., Fahy, N., Clyde, B., Chant, A.: Frameworks for supporting patient and public involvement in research: systematic review and co-design pilot. Health Expect. 22(4), 785–801 (2019)
Urban, M.: Embodying digital ageing: Ageing with digital health technologies and the significance of inequalities. Medicine, Political Science, p. 163–178 (2017)
McVean, S.: Digital health technologies in a deprived community: a qualitative co-design study. PhD thesis (2020). https://rgu-repository.worktribe.com/output/1239514
Coulter, A., Locock, L., Ziebland, S., Calabrese, J.: Collecting data on patient experience is not enough: they must be used to improve care. BMJ Clin. Res. 348(1), g225 (2014)
Perry, M.L., Morken, V., Peipert, D.J., Yanez, B., Garcia, F.S., Barnard, C., Hirschhorn, R.L., Linder, A.J., Jordan, N., Ackermann, T.R., Harris, A., Kircher, S., Mohindra, N., Aggarwal, V., Frazier, R., Coughlin, A., Bedjeti, K., Weitzel, M., Nelson, C.E., Elwyn, G., Van Citters, D.A., O’Connor, M., Cella, D.: Patient-reported outcome dashboards within the electronic health record to support shared decision-making: protocol for co-design and clinical evaluation with patients with advanced cancer and chronic kidney disease. JMIR Res. Protoc. 11(9), 38461 (2022)
Muoio, D.: BlueStar’s eighth FDA clearance adds long-acting basal insulin support for Type 2 patients. Accessed 9 Sept 2022 (2020). https://www.mobihealthnews.com/news/bluestars-eighth-fda-clearance-adds-long-acting-basal-insulin-support-type-2-patients
Koyama, A., Arai, J., Sasaki, S., Barolli, L.: Design, field experiments and evaluation of a web-based remote medical care support system. Int. J. Web Grid Serv. 4(1), 80–99 (2008)
Lowry, S.Z., Quinn, M.T., Ramaiah, M., Brick, D., Patterson, E.S., Zhang, J., Abbott, P., Gibbons, M.C.: A Human Factors Guide to Enhance EHR Usability of Critical User Interactions when Supporting Pediatric Patient Care. NIST. Accessed 31 Mar 2022 (2012). https://www.nist.gov/publications/nistir-7865-human-factors-guide-enhance-ehr-usability-critical-user-interactions-when
Andersen, T.O.: Large-scale and long-term co-design of digital health. Assoc. Comput. Mach. 26(5), 74–77 (2019)
Brown, A., O’Connor, S.: Mobile health applications for people with dementia: a systematic review and synthesis of qualitative studies. Inf. Health Soc. Care. 45(4), 343–359 (2020)
Thabrew, H., Stasiak, K., Merry, S.: Protocol for co-design, development, and open trial of a prototype game-based ehealth intervention to treat anxiety in young people with long-term physical conditions. JMIR Res. Protoc. 6(9), e171 (2017)
Kakkar, A., Garg, A.: Pervasive health monitoring of special child using iot and cloud technologies. In: International conference on intelligent computing and control systems (ICCS), pp. 98–102 (2019)
Georgsson, M., Staggers, N., Arsand, E., Kushniruk, A.: Employing a user-centered cognitive walkthrough to evaluate a mhealth diabetes self-management application: a case study and beginning method validation. J. Biomed. Inf. 91, 103–110 (2019)
Mindo, K.: Implementing a fused machine learning model for the provision of smart health care in manets. Int. J. Comput. Sci. Inf. Secur. (IJCSIS) 17(9), 33 (2019)
Dachyar, M., Zagloel, T.Y.M., Saragih, L.R.: Knowledge growth and development: internet of things (IOT) research, 2006–2018. Heliyon 5(8), 02264 (2019)
Abdelgawad, A., Yelamarthi, K., Khattab, A.: Iot-based health monitoring system for active and assisted living. Conference on smart objects and technologies for social good (GOODTECHS), Springer, Cham, pp.11–20 (2016)
Zgheib, R., Conchon, E., Bastide, R.: In: Ganchev, I., Garcia, N.M., Dobre, C., Mavromoustakis, C.X., Goleva, R. (eds.) Semantic middleware architectures for IoT healthcare applications, pp. 263–294. Springer, Cham (2019)
Nusir, M., Tariq, U., Ahanger, T.A.: Engaging diverse stakeholders in interdisciplinary co-design project for better service design. J. Cases Inf. Technol. (JCIT) 23(4), 1–29 (2021)
Industry, Food, Staff, D.A.: Clinical Decision Support Software. Food and Drug Administration (FDA). Accessed 6 Mar 2020 (2019). https://www.fda.gov/regulatory-information/search-fda-guidance-documents/clinical-decision-support-software
Holzinger, A., Weippl, E., Tjoa, A.M., Kieseberg, P.: Digital transformation for sustainable development goals (sdgs) : a security, safety and privacy perspective on ai. In: Holzinger, A., Kieseberg, P., Tjoa, A.M., Weippl, E. (eds.) Mach. Learn. Knowl. Extr., pp. 1–20. Springer, Cham (2021)
Nebeker, C., Torous, J., Bartlett Ellis, R.J.: Building the case for actionable ethics in digital health research supported by artificial intelligence. BMC Med. 17(1), 137 (2019)
Acknowledgements
This study is supporting via funding from Prince Sattam bin Abdulaziz University project number (PSAU/2023/R/1444).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nusir, M., Rekik, M. Systematic review of co-design in digital health for COVID-19 research. Univ Access Inf Soc 23, 637–651 (2024). https://doi.org/10.1007/s10209-022-00964-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10209-022-00964-x