Abstract
The ever-increasing amount of waste produced by the healthcare system is a growing burden worldwide. To effectively reduce waste, it is essential to know exactly what it is and to explore the factors influencing its amount. This study aims to analyze the amount of healthcare waste (HCW) and the change in that amount over time, as well as to explore and quantify the factors that influence hazardous healthcare waste (HHCW) in a university hospital. Descriptive statistical analysis, Spearman’s correlation and robust regression were performed to characterize the data. Our analysis revealed that the amount of HCW has been increased annually by 2.11%, and the generation rate ranges between 2.53 and 2.68 kg/bed/day. The amount of HHCW has increased by 20.19% over the 5-year period studied, with a generation rate varying between 1.13 and 1.31 kg/bed/day. It was found that surgical specialisms, anesthesiology and intensive care, and emergency patient care have higher rates of hazardous waste production. A significant positive correlation was found between the amount of hazardous waste and the incidence of healthcare-associated infections (r = 0.704), and the number of diapers used by adults and children (r = 0.555), whose significant predictive role was also confirmed by the robust regression.
Similar content being viewed by others
Introduction
Climate change is the largest and longest lasting global public health threat ever described [1]. The effects on health caused by anthropogenic climate change can be direct (e.g. the effects of heat waves, floods, storm-related deaths, injuries) and indirect (e.g. the incidence of vector-borne diseases, water quality, air quality, availability and quality of food). As a result, a huge additional burden appears in the health sector as well [2]. Despite efforts by healthcare systems to cope with the increasing disease burden, hospitals and other healthcare facilities are significant contributors to environmental pollution and the depletion of natural resources, which ultimately exacerbates the issue of climate change [3].
Due to world population growth and progress in access to medical services, in line with the development of the healthcare industry, the amount of healthcare waste (HCW) is also increasing at an exponential rate [4]. The legal regulation of waste generated in the healthcare sector may differ from region to region and country to country, but there are many differences even between the definitions used [5, 6]. According to the WHO, the term HCW includes all the waste generated within healthcare facilities, research centres and laboratories related to medical procedures [7]. As estimated by WHO in 2014, the amount of HCW in the countries of the world ranged from 0.5 to 3.0 kg/bed/day [7].
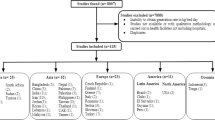
Hospitals in high-income countries generate, on average, more HCW than hospitals in low- and middle-income countries [8]. A study [6] that performed a meta-analysis of medical waste in 78 countries between January 2000 and May 2021 found an average of 2.04 kg of HCW generated per hospital bed per day (0.3–8.4 kg/bed/day). Singh et al. found that the smallest amount of HCW was generated in Africa, with an average of 1.17 kg/bed/day (0.4–2.5 kg/bed/day), followed by Asia with an average of 1.68 kg/bed/day (0.3–5.4 kg/bed/day). In Europe, the average HCW generation rate was already 2.61 kg/bed/day (0.3–4.4 kg/bed/day) and the largest amount of HCW was generated in America, with an average of 3.82 kg/bed/day (0.4–8.4 kg/bed/day). Other studies in Europe found that Greece (0.3 kg/bed/day) [9] had a lower HCW generation rate, while much higher HCW generation rates were reported in Turkey (2.11 kg/bed/day) [10], Portugal (2.5–4.5 kg/bed/day) [11] and France (3.3 kg/bed/day) [12].
Globally, the total mass of HCW is constantly increasing by 2–3% per year, which has only been exacerbated by the COVID-19 pandemic [13,14,15]. So far, approximately 8.4 million tons of pandemic-related plastic waste have been generated, 73% of which came from the healthcare sector [16]. The increase in the generation rate of HCW mostly affects developed countries, and the environmental and public health damage resulting from the difficulties of waste management and disposal are mainly problems of developing countries [7, 17].
Problems related to HCW are mainly caused by general legal deficiencies and contradictions, insufficient waste management knowledge and attitudes of employees, as well as inadequate identification, treatment, and disposal of waste [6, 18]. The effective treatment of HCW has significant public health, patient safety, environmental and economic benefits, which have already been investigated in numerous studies [19,20,21,22]. Despite different legal regulations and definitions, HCW is typically divided into two main groups: hazardous and non-hazardous (general) waste. General HCW does not pose a significant environmental or health risk, and its composition corresponds mostly to domestic waste [7]. Hazardous healthcare waste (HHCW) can represent a significant biological, chemical, physical or radioactive hazard (and often combinations of these), and their management requires special measures (selection, storage, transport, disposal) [23,24,25]. For this reason, the cost of treatment is ten times higher for hazardous waste compared to non-hazardous waste [26]. HHCW can be further divided into seven groups: infectious waste, pathological waste, sharp waste, chemical waste, pharmaceutical waste, cytotoxic waste, and radioactive waste [7]. About 90–95% of HHCW is infectious, which means a potential biological pathogenic attribute [7]. In these cases, an amount or concentration of microorganisms sufficient to cause a disease may be present [24, 27]. Pursuant to the WHO report [7], the proportion of non-HHCW can be set at 75–90%, and that of HHCW at 10–25% (infectious 10%, chemical/radioactive 5%). This distribution corresponds to that described in the international literature, although some authors have reported a much higher HHCW rate (39–42%) [28, 29]. In Greece, the amount of HHCW generated per day per hospital bed was determined on average at 0.7 kg, and the largest producers were university hospitals [9]. The amount of HHCW in Qatar’s hospitals ranged between 2.6 and 3.1 kg/bed/day, and showed a continuous increase [30]. According to the WHO’s estimate, there is an average of 0.2–0.5 kg of HHCW per hospital bed per day in each country [7]. During the COVID-19 pandemic, the generation rate of HHCW increased to 3.4 kg/bed/day worldwide, which is mostly due to the increased use of disposable personal protective equipment [16, 31].
In addition to COVID-19, another major burden on hospitals is the continued increase in healthcare-associated infections (HAIs) [32]. The total number of HAIs occurring in European hospitals can be estimated at around 4.5 million. On average, 1 in 15 hospitalized patients suffer from at least one HAI [33]. Effective infection control is the basis of protection against healthcare-related infections. Infection control activity using with the use of single-use medical devices and personal protective equipment contributes significantly to the increase in the amount of HHCW [34, 35].
Several studies have dealt with the factors affecting the amount of HCW [9, 12, 30, 36]. In most cases, the investigated factors were the type of hospitals, the number of beds, the number of inpatients, the number of outpatients, the number of patient days, the number of intensive care beds, and other special factors. It can be assumed that the amount of HCW can be influenced by many other factors besides these.
The amount of single-used adult and children’s diapers that have become waste could be an influencing factor. This is generally treated as non-hazardous waste and can account for around 1.5–4% of the total waste stream [37].
In Hungary, for the legal regulation of waste generated in the healthcare sector, Act CLXXXV of 2012 on waste and the EMMI regulation of the Act 12/2017 (VI.12.) is responsible for waste management activities related to waste generated at the healthcare provider [38, 39]. The law distinguishes between hazardous and non-hazardous waste and further divides HHCW into special HCW and chemical waste. Special HCW includes sharp or pointed instruments, waste contaminated with blood and secretions, blood and blood products, organ remains, waste from experimental animals, waste contaminated with cytostatics, microbiological waste, and waste generated during the care of an infectious patient. According to the law, single-use adult and children’s diapers are to be separated as general waste (with the exception of the diapers of infectious patients), but experience shows that the majority of Hungarian hospitals treat them as hazardous waste.
Although many studies have been conducted on HCW at a global level, our understanding of waste produced by hospitals in the Central European region is limited. Therefore, this work aims to provide an analytical study through the examination of HCW, which is currently experiencing a huge backlog, particularly in Central Europe. The study analyzes the amount, composition, and generation rate of HCW at a university hospital, tracks changes over time and compares the findings with other published data. Factors influencing HHCW are examined through correlation and regression analysis, with a focus on the impact of each medical specialty. The main goal of this study is to conduct a complex investigation of HCW and to identify and statistically validate new, so far unexplored factors affecting HHCW in order to promote higher quality and a safer environment for patients and healthcare workers in an environmental-friendly manner.
Materials and methods
Study area, and period
Our study was conducted at the University of Debrecen Clinical Centre Nagyerdei Campus (UDCC NC), Hungary. The statistical analysis covered waste from patient care and education/research activities generated between 2017 and 2021. The 5-year period corresponds to the statistical investigation, and the most recent data were available for the year 2021. The examined centre consists of 24 independent and separate clinics, 9 other therapeutic and diagnostic units, and 28 smaller educational/research institutions. At the clinics, specialism-specific care is provided, which is typically the treatment of a group of patients belonging to a specific specialism.
Data sources
Data on the amount of HCW generated at the UDCC NC area were collected at the institutional level from the National Environmental Protection Information System [41]. This online interface provides a direct connection to the IT system operated by the Ministry of Agriculture, where hospitals upload their waste usage data according to legal regulations. The distribution of the amount of special HHCW among clinics and medical specialisms was determined based on the distribution of containers used to collect hazardous waste. The amount and distribution of chemical and radioactive hazardous waste by clinics are documented by the responsible department of the UDCC NC (Department of Occupational Safety, Health Protection, and Environmental Protection).
The European Waste Catalog (EWC) codes are used to classify waste in Hungary [40]. Each EWC main group code can contain both hazardous and non-hazardous waste. HHCW is defined as waste that poses a biological, chemical, physical or radioactive hazard.
The number of beds and patient traffic data required for statistical examinations were collected from the annual publications of the National Health Insurance Fund of Hungary. These were the following: number of active beds, number of inpatients treated, number of patient days, bed occupancy percentage, and mortality percentage. Annual data on diaper use was provided by the UDCC NC Procurement Department.
To determine the annual number of HAIs, the MedWorkS microbiological information system’s MedBacter module was used. For accurate classification, additional information was obtained from the UDMED system, which is the medical system developed by the UDCC NC.
Medical specialisms
Twenty-two medical specialisms were identified at the UDCC NC (Table 3). The classification by medical specialism was determined by assigning corresponding specialism types to each active patient bed. Due to the clinic’s layout, it was not difficult to separate the HHCW amounts related to each medical specialism, as each clinic typically serves only one type of specialism.
Influencing factors
Precisely defined concepts were used to characterize the effect of factors potentially affecting the amount of HHCW.
Laboratory-proven, healthcare-related infections that developed more than 48 h after hospital admission are classified as HAIs. In order to examine the number of HAIs as a factor independent of the amount of waste, the incidence was calculated by determining the number of HAIs per 100,000 nursing days.
The Hospital Hygiene Department of the examined institution classifies the infections into the three main groups: antibiotic-sensitive infections, infections caused by multidrug-resistant (MDR) organisms, and colitis caused by the bacterium Clostridioides difficile (CDI). Of these, all waste from patients with MDR and CDI infections (as they require isolation) is classified as hazardous waste and thus contributes significantly to the amount of HHCW. Between 2017 and 2021, the following HAIs occurred most frequently in the UDCC NC area: MDR Enterobacter spp., MDR Stenotrophomonas malthophilia, Vancomycin-resistant Enterococcus, carbapenem-resistant Enterobacteriaceae, MDR Escherichia coli, MDR Pseudomonas aeruginosa, MDR Acinetobacter baumannii, MDR Klebsiella spp., Methicillin-resistant Staphylococcus aureus, and C. difficile.
Diaper usage data refer to the number of children’s and adult diapers ordered and used in the units of the studied institution. The diapers are available in several sizes (XS, S, M, L, XL), but all sizes were counted as one unit, as information on the actual weight was missing.
The average number of active beds is a weighted average of the number of operating hospital beds which also reflects the changes occurring during the relevant period. The number of inpatients refers to the total number of patients who were discharged from the hospital or transferred to another care facility or who died during the given period. A patient day was considered to be a full day (24 h) of care for an inpatient. The day of admission and departure was considered as a patient day. The bed occupancy percentage is the number of completed care days divided by the number of available care days and multiplied by 100. The mortality percentage is the number of deaths divided by the number of patients discharged alive and multiplied by 100. The surgical/non-surgical classification of each department was based on whether the department had its own operating theatre.
Data analysis
First, a descriptive statistical analysis was carried out. The composition of the HCW generated at UDCC NC between 2017 and 2021, and the distribution of each waste type were examined. The mass of waste generated in each year was determined, expressed in tons. In addition to the total amount of HCW, the amount of non-hazardous and hazardous waste was also examined to get a more accurate picture of the changes in each year and their possible causes. The HCW and HHCW generation rates were calculated for each year: the total annual HCW/HHCW quantity in kilograms was divided by the number of days in the given year and the number of active beds in the institution.
When examining the amounts of HHCW related to individual medical specialisms, the average waste amounts generated between 2017 and 2021 were calculated, not including the teaching/research activities and other therapeutic or diagnostic units. The percentage contribution of each specialism to all HHCW (produced by the specialisms) was analyzed, and the average number of active beds for each year was determined. Then the HHCW generation rates and their standard deviation was calculated. For all the examined factors, a ranking was established among the medical specialisms for easier comparison. To determine and characterize the relationship between the amount of HHCW and the potential influencing factors, a Spearman’s correlation using summarized data from the observed period was performed. The strength of the relationship was classified based on the “r” value: no relationship below 0.2, weak relationship from 0.2, moderate from 0.3, strong from 0.4, and very strong from 0.7 [41]. The results obtained are plotted on a dot diagram (Fig. 4).
Since the data are not normally distributed, robust regression was performed to confirm the correlation test. The amount of HHCW generated at the UDCC NC between 2017 and 2021 was given as the dependent variable, and the possible influencing factors as the independent variable. In our analysis, a p-value of less than 0.05 was considered significant. Intercooled Stata v17 was used for the analysis (ref: StataCorp. 2021. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC.)
Results
Composition of HCW
HCW at UDCC NC consists of hazardous and non-hazardous (general) waste. HHCW can be further divided into special HHCW, chemical and radioactive waste. The non-hazardous waste consisted of mixed municipal solid waste and other selectively collected waste. The detailed composition of HCW generated between 2017 and 2021 is presented in Table 1. The proportion of the annual hazardous waste in the examined period ranged between 44 and 49%, whiles non-hazardous waste was between 51 and 56%. 43–47% of all waste contains special HHCW, which accounted for an average of 96.43% of hazardous waste. The special HHCW was placed in bulk in a common waste collection container. Based on our observations, only sharp and pointed tools and instruments were collected selectively in a smaller container designed for this purpose, but in the end, this also went into the common bulk. These are disposed of outside the institution, by incineration (organ remains, waste from experimental animals, waste contaminated with cytostatics, microbiological waste, used adult and child diapers) or sterilization (sharp and pointed instruments, waste contaminated with blood/secretions, blood and blood products, waste from infectious patient care). It was also observed that used adult and child diapers (regardless of whether they come from infectious or non-infectious patients) are always separated as special HHCW. Looking at the number of diapers used, it was found that the UDCC NC units use an average of 363,248 diapers per year.
Chemical and radioactive waste accounted for only 1.5–2% of all waste during the research period, which represents 3.57% of HHCW. These were collected selectively, which were divided into 10 main EWC groups and radioactive waste. Most of the chemical waste came from the hazardous elements of the EWC 14, 15, 20 main groups (organic solvents, acid, alkali and contaminated packaging materials), which accounted for almost 88% of all chemical waste. 84.7% of the non-hazardous waste was mixed municipal solid waste, which was collected in bulk like residential waste. Sorted waste accounted for 15.3%, and the two most common types of waste (99%) came from the non-hazardous elements of the main groups 15 and 20 of the EWC (separated non-hazardous packaging waste, paper and cardboard).
HCW and HHCW volumes and waste generation rates
Table 2 shows the amount of waste generated between 2017 and 2021. The most HCW was generated in 2021 (1634 tons), the least in 2020 (1482 tons). It can be said that the amount of HCW increased by 9.49% during the 5 years of the study, an average of 2.11% per year. A decrease was only experienced in 2020. Within HCW, the amount of hazardous waste was also the largest in 2021 (796 tons). The volume of HHCW increased by 20.19% and showed an average annual growth rate of 4.38%.
Figure 1 shows the waste generation rates and their annual changes. The average daily amount of HCW per bed ranged between 2.53 and 2.68 kg/bed/day during the examined period. The generation rate of HHCW ranged from 1.13 to 1.31 kg/bed/day. Between 2017 and 2021, the HCW production rate of the investigated institution increased by 4.7%, and the HHCW production rate increased by 15.9%. The number of inpatients treated at UDCC NC ranged from 71,461 to 91,515. The highest number of patients were admitted to the facility in 2021 and the lowest in 2020.
HHCW quantities associated with medical specialisms
Table 3 presents the ranking of the medical specialisms based on their average contribution to HHCW, the number of active beds and the HHCW generation rate with its minimum and maximum value between 2017 and 2021. Figure 2 describes the relationship between HHCW quantities and waste production rates related to each specialism. Among the 22 specialisms of the examined university hospital, internal medicine (16.22%), anesthesiology and intensive care (10.09%), and surgery (9.39%) produced the largest amount of HHCW. Together, they accounted for 35.7% of all HHCW in the hospital. Otorhinolaryngology, rheumatology, and psychiatry contributed the least to HHCW, totaling less than 1%. In terms of HHCW quantities divided by the number of active beds, the medical specialisms producing the most per day are neurosurgery (3.2 kg/bed/day), heart surgery (2.52 kg/bed/day), and anesthesiology and intensive care (2.38 kg/bed/day). Their numbers were 111–183% higher than the 5-year specialism quantity average (1.13 kg/bed/day). No waste generation rate could be calculated for neonatology and dentistry, as there were no active beds in their cases. Medical specialisms showing the 5 highest deviations in HHCW production rates are illustrated in Fig. 3. The HHCW production rates of anesthesiology and intensive care, pulmonology, and emergency care increased continuously during the reviewed period. The biggest difference was seen in emergency care, where the number of HHCW per bed increased by almost 30 times in 2021 compared to 2017. However, there was a decrease in two surgical specialisms (general surgery and oro-maxillofacial surgery).
Potential factors influencing the amount of HHCW
Simple statistical analysis: The data showed a non-normal distribution. Spearman’s rank correlation was performed as a simple statistical analysis to examine the possible factors influencing the amount of HHCW. Figure 4 presents the factors that were hypothesized to be correlated with HHCW. According to the results, there is a significant and positive relationship with all the investigated factors (a p-value of less than 0.05 was considered significant). The incidence of HAIs (r = 0.704) showed a very strong correlation with the amount of HHCW. A strong relationship was verified with the mortality percentage (r = 0.563) and the number of diapers (r = 0.555). The weakest relationship was with the bed occupancy (r = 0.249).
Multiple statistical analysis: The results of the robust regression of factors potentially affecting the amount of HHCW are shown in Table 4 (a p-value of less than 0.05 was considered significant). A statistically significant positive relationship was shown with the incidence of HAIs (p < 0.001), the number of adult and child diapers (p = 0.008), and the surgical/non-surgical nature of the care unit (p = 0.032). Bed occupancy gave a borderline significant p-value (p = 0.052). Our results showed that the year of waste generation has no statistically measurable effect on the amount of HHCW generated (reference year: 2017).
Discussion
A high rate of HHCW (average 46.42%) was found in the university hospital studied. This is significantly different from the WHO estimate of 10–25%, but other authors have reported higher HHCW rates [28, 29]. This can be explained by the excess amount of hazardous waste from teaching/research activities, which is typical for university hospitals. The low share of selectively collected HHCW (3.57%) is largely due to national legislation, which does not require the sorting of special HHCW. Furthermore, the treatment of adult and children’s diapers as hazardous waste can also be a significant contributing factor.
The amount of waste generated and the waste production rate over the period under study clearly show a steady increase (Table 2 and Fig. 1), at a rate (2.11% on average) in line with the 2–3% annual increase reported in the literature [13]. Hazardous waste has increased faster than non-hazardous, which can be explained by the increasing use of single-use medical devices and personal protective equipment (they are mostly contaminated with blood, exudate, chemical substances, and contain sharp parts and should therefore be separated as hazardous waste).
A decrease in the volume of HCWs was only observed in 2020 (5.1% on average), probably caused by a decrease in patient flows due to the first wave of the COVID-19 pandemic. During this period, the number of people seeking specialist care decreased and elective interventions were postponed. This is confirmed by the inpatient data shown in Fig. 1, which shows a significant decrease (18.75%) in inpatient admissions in 2020 compared to the previous year. The amount of HCW has decreased to a much lesser extent than the number of admitted inpatients. The reason for the discrepancy is the changed patient population due to COVID-19 and the infection control measures introduced due to the pandemic. The patients infected with COVID-19 needed longer care, the patients’ condition worsened due to the postponed operations, and they needed more invasive interventions and medical devices. Wearing a mask was mandatory and special attention was paid to the use of other personal protective equipment (PPE), which increased the amount of waste.
Comparing our results with the HCW generation rates of other hospitals, it was found that they correspond to both WHO estimates (0.5–3.0 kg/bed/day) and the European hospitals averages (0.3–4.5 kg/bed/day) [6, 7, 9,10,11,12]. Regarding HHCW, literature sources have reported significant differences between hospitals (for example, due to different classification, legal regulations, type of institution and different economic situation), which makes comparisons difficult. Compared to the WHO estimate of 0.2–0.5 kg/bed/day, the average amount of HHCW experienced by us is more than 2.5 times higher [7]. However, studies in the Middle East region (Qatar, Iran, Jordan, Kuwait) have described even higher HHCW generation rates (2.6–3.81 kg/bed/day) [17, 30, 42, 43].
Significant differences in HHCW production were observed among medical specialisms (Table 3, Figs. 2, 3). The specialisms with the highest average number of beds produced the most HHCW. It is understandable that the more active beds there are in a specialism, the higher the number of patients there are to be treated, resulting in a higher amount of waste. From the production rates and their standard deviations, it is possible to deduce the characteristics associated with the occupations that influence the amount of HHCW. Previous studies have shown a prominent contribution of surgery and intensive care to HHCW, which was confirmed in this study [12, 36, 44].
It was found that surgical specialisms (heart surgery, neurosurgery, urology, dermatology, oro-maxillofacial surgery), as well as anesthesiology and intensive care and emergency patient care are characterized by higher HHCW production rates (Fig. 2). This is because these specialisms use most single-use medical devices (single-use breathing tubes, endoscopes, surgical instruments, infusion sets, etc.) and personal protective equipment. Another possible explanation is that surgery and intensive care increase the risk of HAIs, leading to an increase in infectious waste.
Over the 5 years under review, there was a marked variation in HHCW production rates for some specialisms. (Fig. 3) In anesthesiology and intensive care, the HHCW production rates increased by more than 160%, with a continuous growth. This can also be seen in the case of pulmonology, where the increase was almost 225% between 2017 and 2021. Both specialisms showed higher increases during the pandemic period, which is understandable, since the COVID-19 infected patients requiring inpatient care burdened these two specialisms the most. The institution’s waste collection policy did not change significantly during the pandemic, but specialism-specific COVID-19 care was implemented.
In the case of the two surgical specialisms, however, the pandemic had the opposite effect, as elective surgery was postponed, thus reducing the amount of HHCW. The reason for the drastic increase observed in emergency patient care is that in 2018, the care area of this specialism expanded and thus the number of active beds as well. In 2021, due to the COVID-19 pandemic, the investigated university hospital was designated as a regional emergency provider for both children and adults. This caused a significant increase of 73% in the amount of HHCW generated per bed per day.
The study showed that several factors influence the amount of HHCW in the university hospital studied (Fig. 4 and Table 4). The results of simple and multiple statistical analysis showed a very strong positive relationship between HHCW and Incidence of HAIs (per 100,000 nursing days). An increase in the incidence of HAIs by 1 resulted in an additional 16.68 kg of HHCW by increasing the amount of infectious waste. It is likely that the incidence of HAIs has an even greater effect (and thus is an important predictor) on the HHCW amount. It not only increases the number of single-use care devices and personal protective equipment used, but also the number of care days. Additional patients can become infected, and since the isolation of patient contacts is also necessary, HAIs contribute to the increase of HHCW on several levels.
Regarding the examined period, it has been shown that a unit increase in the number of adult and child diapers increases HHCW by 0.17 kg, with a strong correlation. This has a significant impact on the amount of HHCW when considering that the studied institution uses on average more than 363,000 adult and children’s diapers per year. Our studies did not prove the influence and predictive effect of the mortality percentage and the individual years (and thus the pandemic period of COVID-19) on the amount of HHCW. The bed occupancy rate, which showed a borderline significant effect, did not prove to be an influencing factor beyond reasonable doubt. Therefore, it was discarded as a factor influencing the amount of HHCW. The correlation revealed for medical specialisms—that surgery (surgical/non-surgical) is a significant determinant of HHCW volume—was also confirmed in the statistical tests.
Conclusions
The analyzes revealed that the amount of HCW in the university hospital under investigation has been increasing continuously, but at a rate consistent with the literature. The waste composition examination indicated a high proportion of HHCW, which can be attributed to the institution’s active educational and research activities. The HCW and HHCW generation rates were in line with the global and European averages, and HHCW generation values showed twice the annual increase compared to HCW values. It was found that surgical and medical specialisms with a high number of invasive interventions had significantly higher HHCW generation rates.
Overall, it can be said that the COVID-19 pandemic had a significant impact on the amount of HHCW only at the level of individual specialisms (anesthesiology and intensive care, pulmonology, and emergency care) in the examined institution. At the institutional level, its indirect negative impact on the treated inpatients can only be mentioned.
Several studies have already proven that the amount of HHCW is influenced by many factors (for example, the number of active beds, the number of inpatients and outpatients, the number of nursing days, etc.). Our study identified influencing factors that have not been revealed so far, thereby contributing to the expansion of our knowledge about HHCW management. The statistically significant effect of previously undescribed new factors was demonstrated, such as the incidence of HAIs and the number of adult and child diapers used.
Based on our results, it can be concluded that the special HHCW should be collected selectively in the studied institution in order to understand its more precise composition. Diapers from non-infectious patients do not require special measures (collection, storage, disposal) and do not need to be treated as hazardous waste under Hungarian legislation. The different practices of the institution under investigation can be explained mainly by the fact that the container used for the collection of HHCW is airtight (it protects against unpleasant odors) and, therefore, more suitable for the placement of the diapers. A solution could be to treat the diapers not as hazardous waste but to collect them in a special (airtight) container. By improving infection control activities, the number of HAIs and thus the amount of HHCW generated during their care can be reduced.
The results of the tests carried out can aid in the more effective planning and implementation of measures aimed at reducing HCW. This leads to a safer environment for patients and staff and contributes to environmental protection.
References
Watts N, Amann M, Ayeb-Karlsson S et al (2018) The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health. Lancet 391:581–630. https://doi.org/10.1016/S0140-6736(17)32464-9
IPCC (2022) Summary for policymakers. IPCC
Yin H, Sharma B, Hu H et al (2024) Predicting the climate impact of healthcare facilities using gradient boosting machines. Clean Environ Syst 12(5):100155. https://doi.org/10.1016/j.cesys.2023.100155
Joneghani NM, Zarrinpoor N, Eghtesadifard M (2022) A mathematical model for designing a network of sustainable medical waste management under uncertainty. Comput Ind Eng 171:108372. https://doi.org/10.1016/j.cie.2022.108372
Lee SM, Lee D (2022) Effective medical waste management for sustainable green healthcare. Int J Environ Res Public Health 19:14820. https://doi.org/10.3390/ijerph192214820
Singh N, Ogunseitan OA, Tang Y (2021) Medical waste: current challenges and future opportunities for sustainable management. Crit Rev Environ Sci Technol 52:2000–2022
WHO (2014) Safe management of wastes from health-care activities, 2nd edn. World Health Organization (WHO), Geneva
Letho Z, Yangdon T, Lhamo C et al (2021) Awareness and practice of medical waste management among healthcare providers in National Referral Hospital. PLoS ONE 16:e0243817. https://doi.org/10.1371/journal.pone.0243817
Sepetis A, Zaza PN, Rizos F, Bagos PG (2022) Identifying and predicting healthcare waste management costs for an optimal sustainable management system: evidence from the Greek public sector. Int J Environ Res Public Health 19:9821. https://doi.org/10.3390/ijerph19169821
Çetinkaya AY, Kuzu SL, Demir A (2020) Medical waste management in a mid-populated Turkish city and development of medical waste prediction model. Environ Dev Sustain 22:6233–6244. https://doi.org/10.1007/s10668-019-00474-6
Lee B-K, Ellenbecker MJ, Moure-Ersaso R (2004) Alternatives for treatment and disposal cost reduction of regulated medical wastes. Waste Manag 24:143–151. https://doi.org/10.1016/j.wasman.2003.10.008
Bdour A, Altrabsheh B, Hadadin N, Al-Shareif M (2007) Assessment of medical wastes management practice: a case study of the northern part of Jordan. Waste Manag 27:746–759. https://doi.org/10.1016/j.wasman.2006.03.004
Li H, Dietl H, Li J (2021) Identifying key factors influencing sustainable element in healthcare waste management using the interval-valued fuzzy DEMATEL method. J Mater Cycles Waste Manag 23:1777–1790. https://doi.org/10.1007/s10163-021-01233-4
Zhao H, Liu H, Wei G et al (2021) Comparative life cycle assessment of emergency disposal scenarios for medical waste during the COVID-19 pandemic in China. Waste Manag 126:388–399. https://doi.org/10.1016/j.wasman.2021.03.034
Wang F, Yu L, Long J et al (2023) Quantifying the spatiotemporal evolution characteristics of medical waste generation during the outbreak of public health emergencies. J Mater Cycles Waste Manag 25:221–234. https://doi.org/10.1007/s10163-022-01523-5
Peng Y, Wu P, Schartup AT, Zhang Y (2021) Plastic waste release caused by COVID-19 and its fate in the global ocean. Proc Natl Acad Sci U S A 118:e2111530118. https://doi.org/10.1073/pnas.2111530118
Alagha O, Alomari A, Jarrah N (2018) Medical waste management and production rate in the Eastern Province of the Kingdom of Saudi Arabia. Euro-Mediterr J Environ Integr 3:35. https://doi.org/10.1007/s41207-018-0078-5
Hassan MM, Ahmed SA, Rahman KA, Biswas TK (2008) Pattern of medical waste management: existing scenario in Dhaka City, Bangladesh. BMC Public Health 8:36. https://doi.org/10.1186/1471-2458-8-36
Ranjbari M, Shams Esfandabadi Z, Shevchenko T et al (2022) Mapping healthcare waste management research: past evolution, current challenges, and future perspectives towards a circular economy transition. J Hazard Mater 422:126724. https://doi.org/10.1016/j.jhazmat.2021.126724
Kleber J, Cohen B (2020) Reducing waste and increasing sustainability in health care settings. AJN Am J Nurs 120:45–48
Slutzman JE, Bockius H, Gordon IO et al (2022) Waste audits in healthcare: a systematic review and description of best practices. Waste Manage Res 41:3–17. https://doi.org/10.1177/0734242X221101531
Takunda S, Steven J (2023) Medical solid waste management status in Zimbabwe. J Mater Cycles Waste Manag 25:717–732. https://doi.org/10.1007/s10163-022-01578-4
Awodele O, Adewoye AA, Oparah AC (2016) Assessment of medical waste management in seven hospitals in Lagos, Nigeria. BMC Public Health 16:269. https://doi.org/10.1186/s12889-016-2916-1
Homayouni Z, Pishvaee MS (2020) A bi-objective robust optimization model for hazardous hospital waste collection and disposal network design problem. J Mater Cycles Waste Manag 22:1965–1984. https://doi.org/10.1007/s10163-020-01081-8
Makan A, Fadili A (2020) Sustainability assessment of healthcare waste treatment systems using surrogate weights and PROMETHEE method. Waste Manage Res 39:73–82. https://doi.org/10.1177/0734242X20947162
Amariglio A, Depaoli D (2021) Waste management in an Italian Hospital’s operating theatres: an observational study. Am J Infect Control 49:184–187. https://doi.org/10.1016/j.ajic.2020.07.013
Hachicha W, Mellouli M, Khemakhem M, Chabchoub H (2014) Routing system for infectious healthcare-waste transportation in Tunisia: a case study. Environ Eng Manag J 13:21–28. https://doi.org/10.30638/eemj.2014.004
Mmereki D, Baldwin A, Li B, Liu M (2017) Healthcare waste management in Botswana: storage, collection, treatment and disposal system. J Mater Cycles Waste Manag 19:351–365. https://doi.org/10.1007/s10163-015-0429-0
Wilujeng S (2019) Medical waste management in private clinics in Surabaya and factors affecting it. Int J GEOMATE 16:34–39. https://doi.org/10.21660/2019.55.4606
Al NH, Izuka K, Edquibal C et al (2021) Quantitative assessment of medical waste management in Hamad Medical Corporation—Qatar. Occup Dis Environ Med 09:112–126. https://doi.org/10.4236/odem.2021.93009
UNEP (2020) Waste management during the COVID-19 pandemic: from response to recovery
ECDC (2013) Point prevalence survey of healthcareassociated infections and antimicrobial use in European acute care hospitals. ECDC, Stockholm
Suetens C, Latour K, Kärki T et al (2018) Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Eurosurveillance 23:1. https://doi.org/10.2807/1560-7917.ES.2018.23.46.1800516
Daschner FD, Dettenkofer M (1997) Protecting the patient and the environment—new aspects and challenges in hospital infection control. J Hosp Infect 36:7–15. https://doi.org/10.1016/S0195-6701(97)90086-4
Ivanović T, Gräbsch C, Som C, Nowack B (2023) The effect of the Sars-Cov-2 pandemic on the use of personal protective equipment in hospitals. J Mater Cycles Waste Manag 25:3093–3103. https://doi.org/10.1007/s10163-023-01745-1
Idowu I, Alo B, Atherton W, Al Khaddar R (2013) Profile of medical waste management in two healthcare facilities in Lagos, Nigeria: a case study. Waste Manag Res 31:494–501. https://doi.org/10.1177/0734242X13479429
Odia EO, Adekunle SA (2017) Green purchasing behaviour among nursing mothers. Afr J Econ Manag Stud 8:147–159. https://doi.org/10.1108/AJEMS-08-2016-0116
Law (2012) Law CLXXXV of 2012 on waste. Hungarian Gazette Date:30.11.2012
Regulation (2017) 12/2017. (VI.12.) EMMI regulation on waste management activities related to waste generated by healthcare providers. Hungarian Gazette Date:10.08.2017
EU (2004) European waste catalogue. Commission Decision 2000/532/EC
Dancey CRJ (2004) Statistics without maths for psychology: using SPSS for windows. Prentice-Hall, London
Sartaj M, Arabgol R (2015) Assessment of healthcare waste management practices and associated problems in Isfahan Province (Iran). J Mater Cycles Waste Manag 17:99–106. https://doi.org/10.1007/s10163-014-0230-5
Hamoda HM, El-Tomi HN, Bahman QY (2005) Variations in hospital waste quantities and generation rates. J Environ Sci Health A 40:467–476. https://doi.org/10.1081/ESE-200045650
Komilis D, Katsafaros N, Vassilopoulos P (2011) Hazardous medical waste generation in Greece: case studies from medical facilities in Attica and from a small insular hospital. Waste Manage Res 29:807–814. https://doi.org/10.1177/0734242X10388684
Funding
Open access funding provided by University of Debrecen.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kaposi, A., Nagy, A., Gomori, G. et al. Analysis of healthcare waste and factors affecting the amount of hazardous healthcare waste in a university hospital. J Mater Cycles Waste Manag 26, 1169–1180 (2024). https://doi.org/10.1007/s10163-024-01890-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10163-024-01890-1