Abstract
Background
Chronic kidney disease–mineral and bone disorder (CKD–MBD), nutritional status, and uremia management have been emphasized for bone management in hemodialysis patients. Nevertheless, valuable data on the importance of muscle mass in bone management are limited, including whether conventional management alone can prevent osteoporosis. Thus, the importance of muscle mass and strength, independent of the conventional management in osteoporosis prevention among hemodialysis patients, was evaluated.
Methods
Patients with a history of hemodialysis 6 months or longer were selected. We assessed the risk for osteoporosis associated with calf circumference or grip strength using multivariable adjustment for indices of CKD–MBD, nutrition, and dialysis adequacy. Moreover, the associations between bone mineral density (BMD), calf circumference, grip strength, and bone metabolic markers were also evaluated.
Results
A total of 136 patients were included. The odds ratios (95% confidence interval) for osteoporosis at the femoral neck were 1.25 (1.04–1.54, P < 0.05) and 1.08 (1.00–1.18, P < 0.05) per 1 cm shorter calf circumference or 1 kg weaker grip strength, respectively. Shorter calf circumference was significantly associated with a lower BMD at the femoral neck and lumbar spine (P < 0.001). Weaker grip strength was also associated with lower BMD at the femoral neck (P < 0.01). Calf circumference or grip strength was negatively correlated with bone metabolic marker values.
Conclusion
Shorter calf circumference or weaker grip strength was associated with osteoporosis risk and lower BMD among hemodialysis patients, independent of the conventional therapies.
Similar content being viewed by others
Introduction
Osteoporosis is one of the major problems in the aging society, as it not only impairs the quality of life because of fractures but also increases the risk of mortality [1]. The frequency of femoral neck fractures is approximately fivefold to sixfold higher in dialysis patients than in healthy subjects [2]. In addition, hemodialysis patients with fractures have an approximately fourfold higher mortality risk [3]. Patients with chronic kidney disease (CKD) are afflicted with several bone metabolism-related conditions, one of which is the CKD-mineral and bone disorder (CKD–MBD) [4]. Typically, CKD causes secondary hyperparathyroidism with increased fibroblast growth factor 23, parathyroid hormone (PTH), and serum phosphorus (P), which affects bone metabolism. Moreover, uremic substances are detrimental to the bone and reduce elastic mechanical properties [5]. For these disease-specific conditions, the Kidney Disease Improving Global Organization and The European Renal Association–European Dialysis and Transplant Association have indicated the importance of controlling CKD–MBD, nutrition, and dialysis adequacy in the bone management of dialysis patients [6, 7].
On the other hand, sarcopenia, which is an equally important problem in an aging society, is exacerbated by CKD because of uremic toxins, oxidative stress, chronic inflammation, and malnutrition [8]. Approximately, 20% of dialysis patients have been reported to have sarcopenia [9]. Thus, hemodialysis patients have specific bone and muscle pathologies.
Bone mineral density (BMD) management is clinically important in osteoporosis and fracture prevention because osteoporosis is diagnosed through bone mass, and low BMD is a risk factor for fractures in hemodialysis patients [10]. Although previous studies have reported the association between low BMD and loss of appendicular skeletal muscle mass in the general population [11, 12], literature elucidating whether a similar relationship also applies to hemodialysis patients is limited. Furthermore, it is unclear whether managing CKD–MBD, nutrition, and uremia alone is sufficient to prevent osteoporosis in hemodialysis patients. In this study, we investigated whether the association between osteoporosis and muscle mass or strength was independent of conventional management to explore the importance of muscle mass and strength for preventing osteoporosis among hemodialysis patients.
Materials and methods
Study design and participants
This is a single-center, cross-sectional study. We screened patients aged over 20 years, who underwent hemodialysis three times a week at Kamiooka Jinsei Clinic (Yokohama, Japan) between July 2020 and April 2021. 200 individuals, who had a history of hemodialysis longer than 6 months and consented to this study, were selected. Among these 200 candidates, we excluded 64 patients (1) who had a history of lower-limb amputation, paralysis of limbs, use of steroids, or bone metastasis of cancer; (2) who were currently undergoing peritoneal dialysis; (3) who were currently receiving anti-osteoporosis drugs; or (4) whose record included a missing value required in the study. Finally, 136 patients were included in our analysis.
Measurement
Bone mineral density
Mean BMD at each position of the lumbar spine (L2–4) and femoral neck was measured by dual-energy X-ray absorptiometry (DXA, Aria Chorale; GE Healthcare Japan Corporation, Tokyo, Japan). For measurement of the lumbar spine, vertebrae with focal changes (i.e., sclerotic changes) or artifacts were excluded. The mean BMD of two or more vertebrae, their T-score, and young adult mean (YAM) were evaluated. Osteoporosis was defined as T-score ≤ − 2.5 in accordance with the definition of the World Health Organization (WHO) [13].
Muscle mass and strength
We measured calf circumference and grip strength [14]. For calf circumference, the circumference of the thickest part of the lower leg was measured with a measuring tape, and the mean value of both sides was calculated. Grip strength was measured using a digital grip strength system (jammer type, MG-4800; MORITOH Co., Aichi, Japan), with the elbow joint bent at a 90° angle in the sitting position. The measurements were taken four times, alternating left and right twice, and the maximum value was obtained.
Nutritional indices
We calculated two nutritional indices, Nutritional Risk Index for Japanese Hemodialysis Patients (NRI-JH) and Geriatric Nutritional Risk Index (GNRI), to assess the nutritional state of each participant [15, 16].
Bone metabolic markers
We measured bone-specific alkaline phosphatase (BALP) and total type I procollagen N-terminal propeptide (P1NP) as bone formation markers and serum tartrate-resistant acid phosphatase 5b (TRACP-5b) as bone resorption marker [17].
Others
Blood samples were obtained on the first dialysis day of the week, 2 days after the previous dialysis day. The behavioral characteristics and clinical history were obtained using a questionnaire and medical records. For details of our methods, see Supplementary methods
Statistical analyses
All analyses were performed by EZR on R Commander version 1.55. Significance was defined as P < 0.05 using two-sided tests.
First, we estimated the odds ratio (OR) for osteoporosis per 1 cm shorter calf circumference or 1 kg weaker grip strength using logistic regression models. Model 1 was unadjusted. Model 2 was adjusted for age, sex, history of diabetes, current smoking status, and habitual alcohol drinking. Model 3 was adjusted for the covariates included in Model 2 as well as serum hemoglobin (Hb), NRI-JH score, intact PTH (iPTH), and Kt/V. Covariates were selected a priori [18, 19]. Since we expected calf circumference and grip strength to be strongly correlated with BMI, we did not select BMI in our main models to avoid multicollinearity. Instead, we analyzed models that included height or DW as sensitivity analyses to ensure that the results did not change when taking body size into account. To confirm the linear relationship between calf circumference or grip strength and the risk for osteoporosis, we estimated adjusted ORs using the covariates in Model 3 between the tertiles based on calf circumference [i.e., Low ≤ 33.4, 33.5 ≤ Medium ≤ 36.5, 36.6 ≤ High (cm)] or grip strength [i.e., Low ≤ 22.3, 22.8 ≤ Medium ≤ 30.9, 31.2 ≤ High (cm)] using the highest group as a reference.
Second, we estimated the Pearson’s product–moment correlation coefficients and 95% confidence interval (CI) for the correlation between BMD and calf circumference or grip strength.
Third, we used multiple linear regression models to calculate standardized β and 95% CI for the association of BMD with calf circumference or grip strength. The linear models were adjusted for the same covariates as in the logistic regression models.
Fourth, we assessed the association between bone metabolic markers and calf circumference, grip strength, or BMD by scatter plotting and correlation tests.
Sensitivity analyses
We performed the following sensitivity analyses by modifying some of the covariates included in Model 3: (1) additionally adjusted for height or dry weight when assessing calf circumference or grip strength, respectively; (2) used GNRI score instead of NRI-JH score; (3) used serum albumin (Alb) instead of NRI-JH score; (4) used corrected serum calcium (Ca) and P levels instead of iPTH; (5) used CKD–MBD drug (i.e., vitamin D receptor activators, phosphate binders, or calcimimetics) instead of iPTH; (6) used log-transformed hemodialysis duration instead of Kt/V.
Subgroup analyses by iPTH or sex
To check the heterogeneity in the association between BMD and calf circumference or grip strength by the levels of iPTH, we performed the subgroup analysis between the low- and high-iPTH groups (i.e., iPTH < 147.5 pg/mL, iPTH ≥ 147.5 pg/mL according to the median value) and included multiplicative interaction terms in the regression models. We also performed subgroup analyses of the female and male groups.
Results
Clinical characteristics
The final analytic sample included 136 patients. Table 1 shows the baseline characteristics. The mean ± standard deviation (SD) of age was 67.4 ± 12.7 years and 25.0% of the subjects were female. The levels of BMD at the femoral neck and lumbar spine were 0.8 ± 0.1 g/cm2 and 1.2 ± 0.3 g/cm2, respectively. The mean calf circumference was 35.3 ± 4.0 cm and the grip strength was 26.9 ± 9.7 kg.
Risk for osteoporosis among hemodialysis patients with decreased calf circumference or grip strength
Forty-five patients, consisting of 23/34 (67.6%) women and 22/102 (21.6%) men, were diagnosed with osteoporosis at the femoral neck. At the lumbar spine, six patients (all women) were diagnosed with osteoporosis. As shown in Table 2, when the risk for osteoporosis diagnosed at the femoral neck was assessed, the estimated OR (95% CI) for osteoporosis per 1 cm shorter calf circumference was 1.25 (1.04–1.54, P < 0.05). The estimated OR for osteoporosis per 1 kg weaker grip strength was 1.08 (1.00–1.18, P < 0.05). In the analysis with calf circumference as a variable (model 3), being female was a significant risk factor for osteoporosis. Furthermore, when calf circumference was divided into three groups according to the tertiles in Fig. 1, the shortest group (Low) and the intermediate group (Medium) were at significantly higher risk for osteoporosis compared to the longest group (High) [OR 6.38 (1.46–32.53), P < 0.05; OR 3.92 (1.07–17.03), P < 0.05, respectively]. For grip strength, although not significant, the Low and Medium groups showed higher ORs compared to the High group in terms of the point estimates [OR 4.80 (0.96–28.60), P = 0.06; OR 3.70 (0.96–18.38), P = 0.06, respectively]. No evidence was found to suggest that there was a non-linear relationship between decreased calf circumference or grip strength and the risk for osteoporosis.
Risk for osteoporosis in tertiles based on calf circumference. Adjusted estimated odds ratios (95% confidence intervals) for osteoporosis in tertiles based on calf circumference [i.e., Low ≤ 33.4 vs. 33.5 ≤ Medium ≤ 36.5 vs. 36.6 ≤ High (cm)] are shown. The estimated odds ratios were adjusted for age, sex, history of diabetes, current smoking status, habitual alcohol drinking, hemoglobin, NRI-JH score, iPTH, and Kt/V. iPTH = intact parathyroid hormone; NRI-JH = nutritional risk index for Japanese hemodialysis patients. *P < 0.05
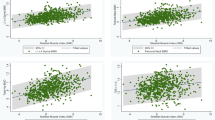
Association between BMD and muscle mass and strength
As shown in Fig. 2, calf circumference was significantly correlated with BMD at both the femoral neck [r (95% CI) = 0.53 (0.40–0.64), P < 0.001] and the lumbar spine [0.41 (0.26–0.54), P < 0.001]. Similarly, grip strength showed correlations with BMD at both the femoral neck [0.56 (0.43–0.66), P < 0.001] and the lumbar spine [0.32 (0.16–0.46), P < 0.001] (Fig. 3).
Scatter plots of the relationships between BMD and calf circumference. Scatter plots of the relationships between BMD at the a femoral neck or b lumbar spine and calf circumference among hemodialysis patients are shown. Each circle represents an individual value. The black lines represent simple linear regression models. The P values were calculated for Pearson’s product–moment correlation coefficients (r-values). BMD bone mineral density
Scatter plots of the relationships between BMD and grip strength. Scatter plots of the relationships between BMD at the a femoral neck or b lumbar spine and grip strength among hemodialysis patients are shown. Each circle represents an individual value. The black lines represent simple linear regression models. The P-values were calculated for Pearson’s product–moment correlation coefficients (r-values). BMD = bone mineral density
In the unadjusted model of linear regression analyses (Table 3), calf circumference and grip strength were associated with BMD at both the femoral neck and lumbar spine. After multivariable adjustment including the indices for managing CKD–MBD, nutrition, and dialysis adequacy (i.e., iPTH, NRI-JH score, and Kt/V), shorter calf circumference was significantly associated with lower BMD at both the femoral neck [β (95% CI) = 0.36 (0.18–0.55), P < 0.001] and the lumbar spine [0.37 (0.16 to 0.56), P < 0.001]. Weaker grip strength was also associated with lower BMD at the femoral neck [0.32 (0.11–0.53), P < 0.01]. Women, non-DM patients, and older age showed significant differences in the association with BMD in our models, while iPTH, NRI-JH score, and Kt/V did not.
Sensitivity analyses and subgroup analyses
We conducted six sensitivity analyses including body size correction, other nutritional indices, and CKD–MBD drug, the results of which were similar in terms of the point estimates (Supplementary Tables S1 and S2).
Furthermore, in the subgroup analysis by iPTH levels, calf circumference was significantly associated with BMD in both groups (Supplementary Table S3). No evidence was found to suggest that iPTH levels interacted in the association between BMD and calf circumference or grip strength (all P for interaction > 0.61). Subgroup analysis by sex also showed a significant association between calf circumference and BMD in both groups (Supplementary Table S4).
Correlations between bone metabolic markers and calf circumference or grip strength
The scatter plots of bone metabolic markers and calf circumference or grip strength are shown in Fig. 4 and Supplementary Fig. S1, respectively. Calf circumference was negatively correlated with log-transformed BALP [r (95% CI) = − 0.32 (− 0.47 to − 0.16), P < 0.001], total P1NP [− 0.21 (− 0.36 to − 0.04), P < 0.05], or TRACP-5b [− 0.31 (− 0.45 to − 0.14), P < 0.001]. Grip strength was also inversely correlated with log-transformed BALP [− 0.33 (− 0.47 to − 0.17), P < 0.001], total P1NP [− 0.28 (− 0.43 to − 0.12), P < 0.001], or TRACP-5b [− 0.33 (− 0.48 to − 0.18), P < 0.001]. Furthermore, in subgroup analysis using the median iPTH as a cutoff, calf circumference was negatively correlated with log-transformed BALP and TRACP5b in both subgroups (Supplementary Table S5). These metabolic markers were also inversely correlated with BMD (Supplementary Fig. S2).
Scatter plots of the relationships between bone metabolic markers and calf circumference. Scatter plots of the relationships between log-transformed a BALP, b total P1NP, or c TRACP-5b and calf circumference are shown. Each circle represents an individual value. The black lines represent simple linear regression models. The P values were calculated for Pearson’s product–moment correlation coefficients (r-values). BALP = bone-specific alkaline phosphatase; P1NP = type I procollagen N-terminal propeptide; TRACP-5b = tartrate-resistant acid phosphatase 5b
Discussion
In the general Japanese population, the prevalence of osteoporosis diagnosed at the femoral neck is reported to be 22.2% in women and 7.0% in men aged 60–69 years [20]. In this study of hemodialysis patients, osteoporosis diagnosed was approximately three times higher than in the general population. Furthermore, in hemodialysis patients, calf circumference and grip strength were significantly associated with the risk for osteoporosis. These associations were independent of the nutritional state (i.e., NRI-JH, GNRI, and serum Alb), CKD–MBD indices (i.e., serum Ca, serum P, iPTH, and use of vitamin D, phosphate binders, or calcimimetics), and dialysis adequacy (i.e., Kt/V). Calf circumference is related to appendicular skeletal muscle mass, and calf circumference and grip strength are used as surrogate markers for the diagnosis of sarcopenia [14, 21]. Hence, our findings may suggest a close association between sarcopenia and osteoporosis in hemodialysis patients.
Similarly, in a multivariate analysis, shorter calf circumference or weaker grip strength were also associated with low BMD. We assessed the heterogeneity in these associations between sexes [22], and the association between muscle mass and BMD was significant in both sexes. We also demonstrated that calf circumference and BMD were inversely correlated with both bone formation and resorption markers. In this study, lower muscle mass and BMD were associated with a higher bone turnover as elevations in both bone formation and resorption markers indicate increased bone metabolism [23]. Because iPTH promotes bone resorption and affects bone rotation [4], this association was also examined in the subgroup analysis of iPTH. The results showed that calf circumference was significantly correlated with BALP or TRACP-5b in both groups. Several reports have already shown that the elevation of these resorption and formation markers was strongly associated with a rapid decrease in BMD and risk for fractures [24]. Thus, our findings indicate that the loss of muscle mass may be associated with a rapid BMD decline due to a high bone turnover and thus require early intervention.
Recently, it has been clarified that muscle can endocrinologically affect bone metabolism via myokines. Myostatin, which promotes bone resorption, is negatively correlated with muscle mass, and elevated myostatin levels may be related to lower BMD in sarcopenia [25]. Additionally, irisin, whose secretion is increased through exercise, inhibits bone resorption via the suppression of receptor activator of nuclear factor κB ligand expression [26]. Therefore, maintaining muscle mass may suppress bone resorption and preserve BMD through these myokines.
In a cross-sectional study of hemodialysis patients, Tominaga et al. and Ito et al. showed that grip strength was not associated with BMD, whereas muscle mass was significantly associated with BMD [21, 27]. In a study of 131 patients undergoing hemodialysis, Lee et al. reported that upper arm circumference and skeletal muscle mass index were lower in the osteopenia and osteoporosis groups than in the normal group [28]. Although these previous studies reported the association between low muscle mass or strength and low BMD or osteoporosis in hemodialysis patients, the association has not been adequately investigated, adjusting for factors (CKD–MBD, nutrition, and uremia) that have traditionally been considered risk factors for osteoporosis. Our results clearly demonstrated this association in hemodialysis patients and indicate the possibility that maintenance or appendicular muscle training may be needed to prevent osteoporosis, in addition to the conventional management of CKD–MBD, nutrition, and dialysis adequacy. Furthermore, we found that lower muscle mass was associated with higher levels of bone metabolic markers and lower BMD in hemodialysis patients. Because dialysis patients are sometimes unable to perform sufficient exercise because of their complications (e.g., heart failure and cerebral infarction), they will have an increased risk of a low BMD. Therefore, a bone resorption inhibitor may be useful for patients who have difficulty performing proper exercise.
In our multiple regression models, the association between grip strength and BMD at the lumbar spine did not reach statistical significance. Bone mass at the lumbar spine of hemodialysis patients was high, despite the exclusion of spines with localized changes on imaging findings. Aortic calcification, a common complication among dialysis patients, affect BMD values at the lumbar spine assessed using DXA [29]. Thus, the femoral neck may be more suitable than the lumbar spine in the assessment of BMD in hemodialysis patients. Also, older age, women, and non-DM patients were significantly associated with osteoporosis risk or lower BMD in our multivariate model. Aging and women are known risk factors for osteoporosis and lower BMD [30], consistent with our results. It has been reported that osteocalcin levels, a marker of bone formation, are decreased in DM patients, and that osteocalcin increases as blood glucose improves [31]. On the other hand, large studies reported that DM patients have rather higher BMD than non-DM patients [32, 33]. The mechanism by which BMD is higher in patients with DM is still unknown; however, it is hypothesized that insulin promotes bone formation by interacting with IGF-1 receptor [34]. In the present study, decreased calf circumference or grip strength was associated with the risk for osteoporosis or lower BMD, even when adjusted for the presence of DM.
This study has several limitations. First, we could not measure muscle mass directly, which might be helpful for the precise diagnosis of sarcopenia. Second, the causal relationship between muscle mass and BMD could not be revealed because of the observational nature of this study. However, it is reasonable to assume that exercise therapy may improve BMD in dialysis patients because it has already been shown that adequate exercise increases BMD in healthy subjects [35]. Prospective interventional studies are needed to confirm this in the future.
Conclusion
Shorter calf circumference and weaker grip strength were associated with osteoporosis risk and lower BMD in hemodialysis patients, independent of the management of CKD–MBD, nutrition status, and dialysis adequacy. In addition, BMD decline with loss of muscle mass may require earlier intervention due to higher bone turnover. To prevent osteoporosis in hemodialysis patients, clinicians should pay attention to calf circumference and grip strength, in addition to the conventional management.
Data availability statement
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513–21.
Wakasugi M, Kazama JJ, Taniguchi M, Wada A, Iseki K, Tsubakihara Y, et al. Increased risk of hip fracture among Japanese hemodialysis patients. J Bone Miner Metab. 2013;31(3):315–21.
Tentori F, McCullough K, Kilpatrick RD, Bradbury BD, Robinson BM, Kerr PG, et al. High rates of death and hospitalization follow bone fracture among hemodialysis patients. Kidney Int. 2014;85(1):166–73.
Khairallah P, Nickolas TL. Updates in CKD-Associated Osteoporosis. Curr Osteoporos Rep. 2018;16(6):712–23.
Iwasaki Y, Kazama JJ, Yamato H, Matsugaki A, Nakano T, Fukagawa M. Altered material properties are responsible for bone fragility in rats with chronic kidney injury. Bone. 2015;81:247–54.
Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Work Group. KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD–MBD). Kidney Int Suppl. 2017;7(1):1–59.
Evenepoel P, Cunningham J, Ferrari S, Haarhaus M, Javaid MK, Lafage-Proust MH, et al. Diagnosis and management of osteoporosis in chronic kidney disease stages 4 to 5D: a call for a shift from nihilism to pragmatism. Osteoporos Int. 2021;32(12):2397–405.
Moorthi RN, Avin KG. Clinical relevance of sarcopenia in chronic kidney disease. Curr Opin Nephrol Hypertens. 2017;26(3):219–28.
Isoyama N, Qureshi AR, Avesani CM, Lindholm B, Bàràny P, Heimbürger O, et al. Comparative associations of muscle mass and muscle strength with mortality in dialysis patients. Clin J Am Soc Nephrol. 2014;9(10):1720–8.
Iimori S, Mori Y, Akita W, Kuyama T, Takada S, Asai T, et al. Diagnostic usefulness of bone mineral density and biochemical markers of bone turnover in predicting fracture in CKD stage 5D patients–a single-center cohort study. Nephrol Dial Transplant. 2012;27(1):345–51.
Genaro PS, Pereira GA, Pinheiro MM, Szejnfeld VL, Martini LA. Influence of body composition on bone mass in postmenopausal osteoporotic women. Arch Gerontol Geriatr. 2010;51(3):295–8.
Verschueren S, Gielen E, O’Neill TW, Pye SR, Adams JE, Ward KA, et al. Sarcopenia and its relationship with bone mineral density in middle-aged and elderly European men. Osteoporos Int. 2013;24(1):87–98.
Report of a WHO Study Group. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. World Health Organ Tech Rep Ser. 1994;843:1–129.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian working group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21(3):300-7.e2.
Kanda E, Kato A, Masakane I, Kanno Y. A new nutritional risk index for predicting mortality in hemodialysis patients: Nationwide cohort study. PLoS ONE. 2019;14(3): e0214524.
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, et al. Geriatric nutritional risk index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005;82(4):777–83.
Nishizawa Y, Miura M, Ichimura S, Inaba M, Imanishi Y, Shiraki M, et al. Executive summary of the Japan osteoporosis society guide for the use of bone turnover markers in the diagnosis and treatment of osteoporosis (2018 Edition). Clin Chim Acta. 2019;498:101–7.
Tominaga H, Oku M, Arishima Y, Ikeda T, Ishidou Y, Nagano S, et al. Association between bone mineral density, muscle volume, walking ability, and geriatric nutritional risk index in hemodialysis patients. Asia Pac J Clin Nutr. 2018;27(5):1062–6.
Yoneki K, Kitagawa J, Hoshi K, Harada M, Watanabe T, Shimoda T, et al. Association between frailty and bone loss in patients undergoing maintenance hemodialysis. J Bone Miner Metab. 2019;37(1):81–9.
Yoshimura N, Muraki S, Oka H, Mabuchi A, En-Yo Y, Yoshida M, et al. Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: the research on osteoarthritis/osteoporosis against disability study. J Bone Miner Metab. 2009;27(5):620–8.
Kawakami R, Murakami H, Sanada K, Tanaka N, Sawada SS, Tabata I, et al. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr Gerontol Int. 2015;15(8):969–76.
Hayashi M, Nakashima T, Yoshimura N, Okamoto K, Tanaka S, Takayanagi H. Autoregulation of osteocyte sema3a orchestrates estrogen action and counteracts bone aging. Cell Metab. 2019;29(3):627-37.e5.
Henriksen K, Christiansen C, Karsdal MA. Role of biochemical markers in the management of osteoporosis. Climacteric. 2015;18(Suppl 2):10–8.
Ross PD, Knowlton W. Rapid bone loss is associated with increased levels of biochemical markers. J Bone Miner Res. 1998;13(2):297–302.
Yarasheski KE, Bhasin S, Sinha-Hikim I, Pak-Loduca J, Gonzalez-Cadavid NF. Serum myostatin-immunoreactive protein is increased in 60–92 year old women and men with muscle wasting. J Nutr Health Aging. 2002;6(5):343–8.
Kawao N, Moritake A, Tatsumi K, Kaji H. Roles of irisin in the linkage from muscle to bone during mechanical unloading in mice. Calcif Tissue Int. 2018;103(1):24–34.
Ito K, Ookawara S, Hibino Y, Imai S, Fueki M, Bandai Y, et al. Skeletal muscle mass index is positively associated with bone mineral density in hemodialysis patients. Front Med (Lausanne). 2020;7:187.
Lee H, Kim K, Ahn J, Lee DR, Lee JH, Hwang SD. Association of nutritional status with osteoporosis, sarcopenia, and cognitive impairment in patients on hemodialysis. Asia Pac J Clin Nutr. 2020;29(4):712–23.
Toussaint ND, Lau KK, Strauss BJ, Polkinghorne KR, Kerr PG. Relationship between vascular calcification, arterial stiffness and bone mineral density in a cross-sectional study of prevalent Australian haemodialysis patients. Nephrology (Carlton). 2009;14(1):105–12.
Gourlay ML, Overman RA, Ensrud KE. Bone density screening and re-screening in postmenopausal women and older men. Curr Osteoporos Rep. 2015;13(6):390–8.
Kanazawa I, Yamaguchi T, Yamauchi M, Yamamoto M, Kurioka S, Yano S, et al. Adiponectin is associated with changes in bone markers during glycemic control in type 2 diabetes mellitus. J Clin Endocrinol Metab. 2009;94(8):3031–7.
Schwartz AV, Vittinghoff E, Bauer DC, Hillier TA, Strotmeyer ES, Ensrud KE, et al. Association of BMD and FRAX score with risk of fracture in older adults with type 2 diabetes. JAMA. 2011;305(21):2184–92.
Oei L, Zillikens MC, Dehghan A, Buitendijk GH, Castaño-Betancourt MC, Estrada K, et al. High bone mineral density and fracture risk in type 2 diabetes as skeletal complications of inadequate glucose control: the Rotterdam Study. Diabetes Care. 2013;36(6):1619–28.
de Liefde II, van der Klift M, de Laet CE, van Daele PL, Hofman A, Pols HA. Bone mineral density and fracture risk in type-2 diabetes mellitus: the Rotterdam Study. Osteoporos Int. 2005;16(12):1713–20.
Lester ME, Urso ML, Evans RK, Pierce JR, Spiering BA, Maresh CM, et al. Influence of exercise mode and osteogenic index on bone biomarker responses during short-term physical training. Bone. 2009;45(4):768–76.
Acknowledgements
This study was supported by a basic research grant from Yokohama City University Medical Center, Yokohama City University, Yokohama, Japan. We thank the dialysis staff and radiology technologists at Kamiooka Jinsei Clinic and Enago (www.enago.jp) for the English language review.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ozawa, M., Hirawa, N., Haze, T. et al. The implication of calf circumference and grip strength in osteoporosis and bone mineral density among hemodialysis patients. Clin Exp Nephrol 27, 365–373 (2023). https://doi.org/10.1007/s10157-022-02308-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-022-02308-8