Abstract
Background
The association between N-terminal pro-brain natriuretic peptide (NT-proBNP) and stroke in Japanese hemodialysis (HD) outpatients is unclear. Therefore, in this study, we investigate whether high NT-proBNP levels are associated with future stroke events in this population.
Methods
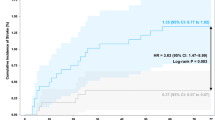
This was a multicenter prospective observational study with post hoc analysis. Baseline NT-proBNP levels were measured at the first HD session of the week and classified into tertiles (first tertile: < 2255 pg/mL; second tertile: ≥ 2255 and < 5657 pg/mL; third tertile: ≥ 5657 pg/mL). Overall hospitalization-free survival rates were compared using the Kaplan–Meier method. The association between NT-proBNP level and hospitalization for stroke was assessed using the multivariate Cox proportional hazards models.
Results
During a 5-year follow-up of 1,229 patients, 103 (8.4%) were hospitalized and 23 (1.9%) died from stroke. The hospitalization-free survival rate for ischemic stroke was lowest in the third tertile (P < 0.01). The crude hazard ratio (HR) of hospitalization was higher in the third tertile compared with the first tertile for both ischemic stroke (HR: 3.92; 95% confidence interval [CI] 2.08–7.37; P < 0.01) and hemorrhagic stroke (HR: 3.75; 95% CI 1.35–10.43; P = 0.01). On multivariate Cox hazard analysis, the adjusted HRs for ischemic stroke were higher in the third tertile. The hospitalization-free survival rates for hemorrhagic stroke and the adjusted HRs did not differ significantly.
Conclusions
Elevated NT-proBNP level was associated with hospitalization for ischemic stroke, suggesting that NT-proBNP level is a valid biomarker for predicting hospitalization for ischemic stroke in HD outpatients.


Similar content being viewed by others
References
Nolan CR. Strategies for improving long-term survival in patients with ESRD. J Am Soc Nephrol. 2005;16:120–7.
Iseki K, et al. Evidence for high risk of cerebral hemorrhage in chronic dialysis patients. Kidney Int. 1993;44:1086–90.
Nitta K, et al. Annual dialysis data report for 2018, JSDT renal data registry: survey methods, facility data, incidence, prevalence, and mortality. Ren Replace Ther. 2020;6:1–18.
Murray AM, et al. Incidence of stroke before and after dialysis initiation in older patients. J Am Soc Nephrol. 2013;24:1166–73.
Nishizawa Y, et al. Intima-media thickness of carotid artery predicts cardiovascular mortality in hemodialysis patients. Am J Kidney Dis. 2003;41:76–9.
Naganuma T, et al. Silent cerebral infarction predicts vascular events in hemodialysis patients. Kidney Int. 2005;67:2434–9.
Naganuma T, et al. Cerebral microbleeds predict intracerebral hemorrhage in hemodialysis patients. Stroke. 2015;46:2107–12.
Di Angelantonio E, et al. B-type natriuretic peptides and cardiovascular risk: systematic review and meta-analysis of 40 prospective studies. Circulation. 2009;120:2177–87.
Sivalingam M, et al. Comparison of B-type natriuretic peptide and NT proBNP as predictors of survival in patients on high-flux hemodialysis and hemodiafiltration. Hemodial Int. 2011;15:359–65.
Yancy CW, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American college of cardiology foundation/American heart association task force on practice guidelines. Circulation. 2013;128:240–327.
Di Castelnuovo A, et al. NT-proBNP (N-terminal pro-B-type natriuretic peptide) and the risk of stroke: results from the BiomarCaRE consortium. Stroke. 2019;50:610–7.
Malachias MVB, et al. NT-proBNP by Itself predicts death and cardiovascular events in high-risk patients with Type 2 diabetes mellitus. J Am Heart Assoc. 2020;9: e017462.
Satyan S, et al. Relationships of N-terminal pro-B-natriuretic peptide and cardiac troponin T to left ventricular mass and function and mortality in asymptomatic hemodialysis patients. Am J Kidney Dis. 2007;50:1009–19.
Winkler K, et al. Change in N-terminal-pro-B-type-natriuretic-peptide and the risk of sudden death, stroke, myocardial infarction, and all-cause mortality in diabetic dialysis patients. Eur Heart J. 2008;29:2092–9.
Kim YK, et al. Association between N-terminal pro-brain natriuretic peptide and acute ischemic stroke in patients on chronic hemodialysis. Int Urol Nephrol. 2010;42:537–43.
Satoh A, et al. N-terminal pro brain natriuretic peptide predicts both all-cause and cardiovascular disease mortality in Japanese hemodialysis patients. Clin Exp Nephrol. 2021;25:1142–50.
Ellinor PT, et al. Discordant atrial natriuretic peptide and brain natriuretic peptide levels in lone atrial fibrillation. J Am Coll Cardiol. 2005;45:82–6.
Wolf PA, et al. Atrial fibrillation as an independent risk factor for stroke: the framingham study. Stroke. 1991;22:983–8.
Whelton PK, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults a report of the American college of cardiology/American heart association task force on clinical practice guidline. Hypertension. 2018;71:e13-115.
Delong ER, et al. Comparing the areas under two or more correlated receiver operating characteristic curves : a nonparametric approach. Biometrics. 1988;44:837–45.
Yotsueda R, et al. Hemoglobin concentration and the risk of hemorrhagic and ischemic stroke in patients undergoing hemodialysis: the Q-cohort study. Nephrol Dial Transpl. 2018;33:856–64.
Seliger SL, et al. Risk factors for incident stroke among patients with end-stage renal disease. J Am Soc Nephrol. 2003;14:2623–31.
Findlay M, et al. Renal replacement modality and stroke risk in end-stage renal disease-a national registry study. Nephrol Dial Transpl. 2018;33:1564–71.
Masson P, et al. Risk of stroke in patients with ESRD. Clin J Am Soc Nephrol. 2015;10:1585–92.
Wang HH, et al. Risk of stroke in long-term dialysis patients compared with the general population. Am J Kidney Dis. 2014;63:604–11.
Kim H, et al. The correlation of left atrial volume index to the level of N-terminal Pro-BNP in heart failure with a preserved ejection fraction. Echocardiography. 2008;25:961–7.
Benjamin EJ, et al. Left atrial size and the risk of stroke and death: the framingham heart study. Circulation. 1995;92:835–41.
Yamazaki M, et al. Relation of N-terminal pro-B-type natriuretic peptide (NT-proBNP) and left atrial volume index to left ventricular function in chronic hemodialysis patients. Heart Vessels. 2011;26:421–7.
Shimizu M, et al. N-terminal pro brain natriuretic peptide as a cardiac biomarker in Japanese hemodialysis patients. Int J Artif Organs. 2018;41:135–43.
Borlaug BA, et al. Ventricular-vascular interaction in heart failure. Heart Fail Clin. 2008;4:23–36.
Matsushita K, et al. High-sensitivity cardiac troponin and natriuretic peptide with risk of lower-extremity peripheral artery disease: the atherosclerosis risk in communities (ARIC) study. Eur Heart J. 2018;39:2412–9.
Feng X, et al. Stroke mechanisms in symptomatic intracranial atherosclerotic disease classification and clinical implications. Stroke. 2019;50:2692–9.
Diederichsen SZ, et al. Natural history of subclinical atrial fibrillation detected by implanted loop recorders. J Am Coll Cardiol. 2019;74:2771–81.
Diederichsen SZ, et al. Incidence and predictors of atrial fibrillation episodes as detected by implantable loop recorder in patients at risk: from the LOOP study. Am Heart J. 2020;219:117–27.
Acknowledgements
This work was supported by Roche Diagnostics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The founders and staff of Roche Diagnostics had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The authors have declared that no conflict of interest exists.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee at which the studies were conducted, the Ethical Committee for Clinical Research of Hiroshima University (IRB approval number H480), and the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10157_2022_2254_MOESM2_ESM.tif
Supplementary file2 ROC curves of pre- and post-HD NT-proBNP for hospitalization for total stroke, ischemic stroke, and hemorrhagic stroke at the 5-year follow-up. Sensitivity and specificity of ROC curves for pre- and post-HD NT-proBNP as predictors of hospitalization for total stroke (A), ischemic stroke (B), and hemorrhagic stroke (C). No significant differences were observed between the AUCs for pre- and post-HD NT-proBNPs (A: P = 0.52, B: P = 0.42, C: P = 0.96). (TIF 1433 KB)
About this article
Cite this article
Yamaoka, M., Yoshida, M., Nakashima, A. et al. N-terminal pro-brain natriuretic peptide predicts hospitalization for ischemic stroke in Japanese hemodialysis patients. Clin Exp Nephrol 26, 1111–1118 (2022). https://doi.org/10.1007/s10157-022-02254-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-022-02254-5