Abstract
Background
Acute diverticulitis with extraluminal air constitutes a heterogeneous condition whose management is controversial. The aims of this study are to report the failure rate of conservative treatment for diverticulitis with extraluminal air and to report risk factors of conservative treatment failure.
Methods
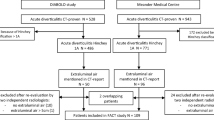
A retrospective study was performed from an institutional review board-approved database of patients admitted with acute diverticulitis with extraluminal air from 2015 to 2021 at a tertiary referral center. All patients managed for acute diverticulitis with covered perforation (without intraabdominal abscess) were included. The primary endpoint was failure of medical treatment, defined as a need for unplanned surgery or percutaneous drainage within 30 days after admission.
Results
Ninety-three patients (61% male, mean age 57 ± 17 years) were retrospectively included. Ten patients had failure of conservative treatment (11%). These patients were significantly older than 50 years (n = 9/10, 90% versus n = 47/83, 57%, p = 0.007), associated with cardiovascular disease (n = 6/10, 60% versus n = 10/83, 12%, p = 0.002), American Society of Anesthesiologists (ASA) score of 3–4 (n = 4/7, 57% versus 6/33, 18%, p = 0.05), under anticoagulant and antiplatelet (n = 6/10, 60% versus n = 11/83, 13%, p = 0.04) and steroid or immunosuppressive therapy (n = 3/10, 30% versus 5/83, 6%, p = 0.04), and with distant pneumoperitoneum location (n = 7/10, 70% versus n = 14/83, 17%, p = 0.001) compared with those with successful conservative treatment. On multivariate analysis, only distant pneumoperitoneum was an independent risk factor of failure (odds ratio (OR) 6.5, 95% confidence interval (CI) [2–21], p = 0.002).
Conclusions
Conservative treatment with antibiotics for acute diverticulitis with extraluminal air is safe with a success rate of 89%. Patients with distant pneumoperitoneum should be carefully monitored.
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sandler RS, Everhart JE, Donowitz M et al (2002) The burden of selected digestive diseases in the United States. Gastroenterology 122:1500–1511. https://doi.org/10.1053/gast.2002.32978
El-Sayed C, Radley S, Mytton J et al (2018) Risk of recurrent disease and surgery following an admission for acute diverticulitis. Dis Colon Rectum 61:382–389. https://doi.org/10.1097/DCR.0000000000000939
Shahedi K, Fuller G, Bolus R et al (2013) Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol 11:1609–1613. https://doi.org/10.1016/j.cgh.2013.06.020
Bridoux V, Antor M, Schwarz L et al (2014) Elective operation after acute complicated diverticulitis: Is it still mandatory? World J Gastroenterol 20:8166–8172. https://doi.org/10.3748/wjg.v20.i25.8166
Sallinen VJ, Mentula PJ, Leppäniemi AK (2014) Nonoperative management of perforated diverticulitis with extraluminal air is safe and effective in selected patients. Dis Colon Rectum 57:875–881. https://doi.org/10.1097/DCR.0000000000000083
Hinchey EJ, Schaal PG, Richards GK (1978) Treatment of perforated diverticular disease of the colon. Adv Surg 12:85–109
Sartelli M, Weber DG, Kluger Y et al (2020) 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emerg Surg 15:32. https://doi.org/10.1186/s13017-020-00313-4
Hall J, Hardiman K, Lee S et al (2020) The American society of colon and rectal surgeons clinical practice guidelines for the treatment of left-sided colonic diverticulitis. Dis Colon Rectum 63:728–747. https://doi.org/10.1097/DCR.0000000000001679
You K, Bendl R, Taut C et al (2018) Randomized clinical trial of elective resection versus observation in diverticulitis with extraluminal air or abscess initially managed conservatively. Br J Surg 105:971–979. https://doi.org/10.1002/bjs.10868
Dharmarajan S, Hunt SR, Birnbaum EH et al (2011) The efficacy of nonoperative management of acute complicated diverticulitis. Dis Colon Rectum 54:663–671. https://doi.org/10.1007/DCR.0b013e31820ef759
Colas PA, Duchalais E, Duplay Q et al (2017) Failure of conservative treatment of acute diverticulitis with extradigestive air. World J Surg 41:1890–1895. https://doi.org/10.1007/s00268-017-3931-9
Costi R, Cauchy F, Le Bian A et al (2012) Challenging a classic myth: pneumoperitoneum associated with acute diverticulitis is not an indication for open or laparoscopic emergency surgery In hemodynamically stable patients. A 10-year experience with a nonoperative treatment. Surg Endosc 26:2061–2071. https://doi.org/10.1007/s00464-012-2157-z
Bolkenstein HE, van Dijk ST, Consten ECJ et al (2019) Conservative treatment in diverticulitis patients with pericolic extraluminal air and the role of antibiotic treatment. J Gastrointest Surg 23:2269–2276. https://doi.org/10.1007/s11605-019-04153-9
Titos-García A, Aranda-Narváez JM, Romacho-López L et al (2017) Nonoperative management of perforated acute diverticulitis with extraluminal air: results and risk factors of failure. Int J Colorectal Dis 32:1503–1507. https://doi.org/10.1007/s00384-017-2852-2
Van Dijk ST, Doelare SAN, Van Geloven AAW, Boermeester MA (2018) A systematic review of pericolic extraluminal air in left-sided acute colonic diverticulitis. Surg Infect 19:362–368. https://doi.org/10.1089/sur.2017.236
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
von Elm E, Altman DG, Egger M et al (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X
Fugazzola P, Ceresoli M, Coccolini F et al (2022) The WSES/SICG/ACOI/SICUT/AcEMC/SIFIPAC guidelines for diagnosis and treatment of acute left colonic diverticulitis in the elderly. World J Emerg Surg 17:5. https://doi.org/10.1186/s13017-022-00408-0
Tejedor P, Pastor C, Pellino G et al (2023) Management of acute diverticulitis with pericolic free gas (ADIFAS): an International multicenter observational study. Int J Surg 109:689–697. https://doi.org/10.1097/JS9.0000000000000213
Vennix S, Musters GD, Mulder IM et al (2015) Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: a multicentre, parallel-group, randomised, open-label trial. The Lancet 386:1269–1277. https://doi.org/10.1016/S0140-6736(15)61168-0
Schultz JK, Yaqub S, Wallon C et al (2015) Laparoscopic lavage vs primary resection for acute perforated diverticulitis: The SCANDIV randomized clinical trial. JAMA J Am Med Assoc 314:1364–1375. https://doi.org/10.1001/jama.2015.12076
Funding
None.
Author information
Authors and Affiliations
Contributions
M.A. and D.M did the conception and design of the work; the acquisition, the analysis and the interpretation of data for the work; F.T. did the acquisition and interpretation of radiological data. All authors reviewed the manuscript and approved the final version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki declaration and its later amendmnentsor comparable ethical standard.
Informed consent
For this type of study formal consent is not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aubert, M., Tradi, F., Chopinet, S. et al. Acute diverticulitis with extraluminal air: is conservative treatment sufficient? A single-center retrospective study. Tech Coloproctol 28, 50 (2024). https://doi.org/10.1007/s10151-024-02928-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10151-024-02928-0