Abstract
Background
Laparoscopic rectal resection is technically challenging, with outcomes dependent upon technical performance. No robust objective assessment tool exists for laparoscopic rectal resection surgery. This study aimed to investigate the application of the objective clinical human reliability analysis (OCHRA) technique for assessing technical performance of laparoscopic rectal surgery and explore the validity and reliability of this technique.
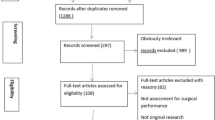
Methods
Laparoscopic rectal cancer resection operations were described in the format of a hierarchical task analysis. Potential technical errors were defined. The OCHRA technique was used to identify technical errors enacted in videos of twenty consecutive laparoscopic rectal cancer resection operations from a single site. The procedural task, spatial location, and circumstances of all identified errors were logged. Clinical validity was assessed through correlation with clinical outcomes; reliability was assessed by test–retest.
Results
A total of 335 execution errors identified, with a median 15 per operation. More errors were observed during pelvic tasks compared with abdominal tasks (p < 0.001). Within the pelvis, more errors were observed during dissection on the right side than the left (p = 0.03). Test–retest confirmed reliability (r = 0.97, p < 0.001). A significant correlation was observed between error frequency and mesorectal specimen quality (r s = 0.52, p = 0.02) and with blood loss (r s = 0.609, p = 0.004).
Conclusions
OCHRA offers a valid and reliable method for evaluating technical performance of laparoscopic rectal surgery.



Similar content being viewed by others
References
Jeong SY, Park JW, Nam BH et al (2014) Open versus laparoscopic surgery for mid-rectal or low-rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol 15:767–774
Bonjer HJ, Deijen CL, Haglind E; COLOR II Study Group (2015) A randomized trial of laparoscopic versus open surgery for rectal cancer. N Engl J Med 373:194
Fleshman J, Branda M, Sargent DJ et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage II or III rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314:1346–1355
Stevenson AR, Solomon MJ, Lumley JW et al (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314:1356–1363
Mackenzie H, Miskovic D, Ni M et al (2013) Clinical and educational proficiency gain of supervised laparoscopic colorectal surgical trainees. Surg Endosc 27:2704–2711
Quirke P, Steele R, Monson J, NCRI Colorectal Cancer Study Group et al (2009) Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet 373:821–828
Martling AL, Holm T, Rutqvist LE, Moran BJ, Heald RJ, Cedemark B (2000) Effect of a surgical training programme on outcome of rectal cancer in the County of Stockholm. Stockholm Colorectal Cancer Study Group. Basingstoke Bowel Cancer Research Project. Lancet 356:93–96
Nagtegaal ID, van de Velde CJ, van der Worp E, Kapiteijn E, Quirke P, van Krieken JH (2002) Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 20:1729–1734
Foster JD, Francis NK (2015) Objective assessment of technique in laparoscopic colorectal surgery: what are the existing tools? Tech Coloproctol 19:1–4
Cuschieri A (2005) Reducing errors in the operating room. Surgical proficiency and quality assurance of execution. Surg Endosc 19:1022–1027
Joice P, Hanna GB, Cuschieri A (1998) Errors enacted during endoscopic surgery—a human reliability analysis. Appl Ergon 29:409–414
Miskovic D, Ni M, Wyles SM, Parvaiz A, Hanna GB (2012) Observational clinical human reliability analysis (OCHRA) for competency assessment in laparoscopic colorectal surgery at the specialist level. Surg Endosc 26:796–803
Tang B, Hanna GB, Bax NM, Cuschieri A (2004) Analysis of technical surgical errors during initial experience of laparoscopic pyloromyotomy by a group of Dutch pediatric surgeons. Surg Endosc 18:1716–1720
Miskovic D, Foster JD, Agha A et al (2015) Standardisation of laparoscopic total mesorectal excision for rectal cancer—a structured international expert consensus. Ann Surg 261:716–722
Foster JD, Gash KJ, Carter FJ et al (2014) Development and evaluation of a cadaveric training curriculum for low rectal cancer surgery in the English Lorec National Development Programme. Colorectal Dis 16:O308–O319
Holm T, Ljung A, Häggmark T, Jurell G, Lagergren J (2007) Extended abdominoperineal resection with gluteus maximus flap reconstruction of the pelvic floor for rectal cancer. Br J Surg 94:232–238
Wilson PJ (2012) Use of human reliability analysis to evaluate surgical technique for rectal cancer. University of Dundee, PhD Thesis
Tang B, Hanna GB, Joice P, Cuschieri A (2004) Identification and categorization of technical errors by Observational Clinical Human Reliability Assessment (OCHRA) during laparoscopic cholecystectomy. Arch Surg 139:1215–1220
Tang B, Hanna GB, Cuschieri A (2005) Analysis of errors enacted by surgical trainees during skills training courses. Surgery 138:14–20
Williams GT, Quirke P, Shepherd NA (2007) Minimum dataset for colorectal cancer. Histopathology Reports (2nd edn). Royal College of Pathologists, London
Munz Y, Moorthy K, Bann S, Shah J, Ivanova S, Darzi SA (2004) Ceiling effect in technical skills of surgical residents. Am J Surg 188:294–300
Hanna GB, Shimi S, Cuschieri A (1997) Optimal port locations for endoscopic intracorporeal knotting. Surg Endosc 11:397–401
Collinson FJ, Jayne DG, Pigazzi A et al (2012) An international, multicentre, prospective, randomised, controlled, unblinded, parallel-group trial of robotic-assisted versus standard laparoscopic surgery for the curative treatment of rectal cancer. Int J Colorectal Dis 27:233–241
Acknowledgments
The authors would like to thank the following experts who participated in the qualitative interviews that were used for development of the task analysis: Professor Willem Bemelman, Mr Mark Coleman, Professor Conor Delaney, Mr Mark Gudgeon, Dr Hitoshi Hasegawa, Professor Robin Kennedy, Professor Wai Lun Law, Professor Roger Motson, Professor Yves Panis, Professor Timothy Rockall, and Professor Steven Wexner.
Funding
This work was supported by the UK National Institute for Health Research, through the Research for Patient Benefit Programme (Grant Number PB-PG-1010-23326). The funding body did not have any role in the planning of the study, recruitment, data collection, or analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the South West England Research Ethics Committee (reference 12/SW/0278).
Informed consent
Written consent was obtained from all patients and also surgeons for the recording and analysis of operations.
Rights and permissions
About this article
Cite this article
Foster, J.D., Miskovic, D., Allison, A.S. et al. Application of objective clinical human reliability analysis (OCHRA) in assessment of technical performance in laparoscopic rectal cancer surgery. Tech Coloproctol 20, 361–367 (2016). https://doi.org/10.1007/s10151-016-1444-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-016-1444-4