Abstract
Since there are many approaches for successful craniopharyngioma resection, how to choose a suitable approach remains problematic. The aim of this study was to summarize experience of approach selection and outcomes of craniopharyngioma resection in our institute. The data of 182 primary craniopharyngiomas between January 2013 and June 2019 were retrospectively reviewed. Craniopharyngiomas were classified into intrasellar, intra-suprasellar, suprasellar, and intra-third ventricle types based on the location. The surgical approaches, extent of resection, endocrine and ophthalmological outcomes, and complications were evaluated. Gross total resection (GTR) was achieved in 158 (86.8%) patients, near-total resection (NTR) in 20 (11%), and partial resection (PR) in 4 (2.2%). New-onset hypopituitarism occurred in 90 (49.5%) and new-onset diabetes insipidus in 48 (26.4%). Visual function was improved in 110 of the 182 patients, unchanged in 52, and deteriorated in 20. For intra-suprasellar and suprasellar tumors, patients in the endoscopic endonasal approach (EEA) group had higher GTR rate, lower incidence of new-onset hypopituitarism, and better visual outcome than patients in transcranial approach group, but no significant difference in the incidence of new-onset diabetes insipidus was found. There were no surgery-related deaths, and the common complications included permanent oculomotor nerve palsy, hemorrhage, and cerebrospinal fluid leaks. During the follow-up period, tumor recurrence or regrowth occurred in 6.6% of the cases. Tumor location is key for choosing an optimal surgical approach for craniopharyngioma resection. The EEA should be considered as the first choice for intra-suprasellar and suprasellar craniopharyngiomas to achieve better visual outcomes and fewer pituitary hormonal disorders.




Similar content being viewed by others
References
Choudhri O, Chang SD (2016) Subfrontal trans-lamina terminalis approach to a third ventricular craniopharyngioma. Neurosurgical Focus 40(Video Suppl 1):2016 2011 FocusVid 15416. https://doi.org/10.3171/2016.1.FocusVid.15416
Jensterle M, Jazbinsek S, Bosnjak R, Popovic M, Zaletel LZ, Vesnaver TV, Kotnik BF, Kotnik P (2019) Advances in the management of craniopharyngioma in children and adults. Radiol Oncol 53(4):388–396. https://doi.org/10.2478/raon-2019-0036
O’Steen L, Indelicato DJ (2018) Advances in the management of craniopharyngioma. F1000Research 7. https://doi.org/10.12688/f1000research.15834.1
Fernandez-Miranda JC, Gardner PA, Snyderman CH, Devaney KO, Strojan P, Suarez C, Genden EM, Rinaldo A, Ferlito A (2012) Craniopharyngioma: a pathologic, clinical, and surgical review. Head Neck 34(7):1036–1044. https://doi.org/10.1002/hed.21771
Gerganov V, Metwali H, Samii A, Fahlbusch R, Samii M (2014) Microsurgical resection of extensive craniopharyngiomas using a frontolateral approach: operative technique and outcome. J Neurosurg 120(2):559–570. https://doi.org/10.3171/2013.9.JNS122133
Weil AG, Robert T, Alsaiari S, Obaid S, Bojanowski MW (2016) Using the trans-lamina terminalis route via a pterional approach to resect a retrochiasmatic craniopharyngioma involving the third ventricle. Neurosurgical Focus 40(Video Suppl 1):2016 2011 FocusVid 15440. https://doi.org/10.3171/2016.1.FocusVid.15440
Kunihiro N, Goto T, Ishibashi K, Ohata K (2014) Surgical outcomes of the minimum anterior and posterior combined transpetrosal approach for resection of retrochiasmatic craniopharyngiomas with complicated conditions. J Neurosurg 120(1):1–11. https://doi.org/10.3171/2013.10.JNS13673
Morisako H, Goto T, Goto H, Bohoun CA, Tamrakar S, Ohata K (2016) Aggressive surgery based on an anatomical subclassification of craniopharyngiomas. Neurosurg Focus 41(6):E10. https://doi.org/10.3171/2016.9.FOCUS16211
Liu JK, Christiano LD, Gupta G, Carmel PW (2010) Surgical nuances for removal of retrochiasmatic craniopharyngiomas via the transbasal subfrontal translamina terminalis approach. Neurosurg Focus 28(4):E6. https://doi.org/10.3171/2010.1.FOCUS09309
Dho YS, Kim YH, Se YB, Han DH, Kim JH, Park CK, Wang KC, Kim DG (2018) Endoscopic endonasal approach for craniopharyngioma: the importance of the relationship between pituitary stalk and tumor. J Neurosurg 129(3):611–619. https://doi.org/10.3171/2017.4.JNS162143
Sankhla SK, Jayashankar N, Khan GM (2015) Extended endoscopic endonasal transsphenoidal approach for retrochiasmatic craniopharyngioma: surgical technique and results. J Pediatr Neurosci 10(4):308–316. https://doi.org/10.4103/1817-1745.174457
Yamada S, Fukuhara N, Oyama K, Takeshita A, Takeuchi Y, Ito J, Inoshita N (2010) Surgical outcome in 90 patients with craniopharyngioma: an evaluation of transsphenoidal surgery. World Neurosurg 74(2–3):320–330. https://doi.org/10.1016/j.wneu.2010.06.014
Kassam AB, Gardner PA, Snyderman CH, Carrau RL, Mintz AH, Prevedello DM (2008) Expanded endonasal approach, a fully endoscopic transnasal approach for the resection of midline suprasellar craniopharyngiomas: a new classification based on the infundibulum. J Neurosurg 108(4):715–728. https://doi.org/10.3171/JNS/2008/108/4/0715
de Divitiis E, Cappabianca P, Cavallo LM, Esposito F, de Divitiis O, Messina A (2007) Extended endoscopic transsphenoidal approach for extrasellar craniopharyngiomas. Neurosurgery 61(5 Suppl 2):219–227; discussion 228. https://doi.org/10.1227/01.neu.0000303220.55393.73
Gardner PA, Kassam AB, Snyderman CH, Carrau RL, Mintz AH, Grahovac S, Stefko S (2008) Outcomes following endoscopic, expanded endonasal resection of suprasellar craniopharyngiomas: a case series. J Neurosurg 109(1):6–16. https://doi.org/10.3171/JNS/2008/109/7/0006
Jane JA Jr, Prevedello DM, Alden TD, Laws ER Jr (2010) The transsphenoidal resection of pediatric craniopharyngiomas: a case series. J Neurosurg Pediatr 5(1):49–60. https://doi.org/10.3171/2009.7.PEDS09252
Liu JK, Christiano LD, Patel SK, Eloy JA (2011) Surgical nuances for removal of retrochiasmatic craniopharyngioma via the endoscopic endonasal extended transsphenoidal transplanum transtuberculum approach. Neurosurg Focus 30(4):E14. https://doi.org/10.3171/2011.1.FOCUS10297
Deopujari CE, Karmarkar VS, Shah N, Vashu R, Patil R, Mohanty C, Shaikh S (2018) Combined endoscopic approach in the management of suprasellar craniopharyngioma. Childs Nerv Syst 34(5):871–876. https://doi.org/10.1007/s00381-018-3735-8
Yasargil MG, Curcic M, Kis M, Siegenthaler G, Teddy PJ, Roth P (1990) Total removal of craniopharyngiomas. Approaches and long-term results in 144 patients. J Neurosurg 73(1):3–11. https://doi.org/10.3171/jns.1990.73.1.0003
Koutourousiou M, Fernandez-Miranda JC, Wang EW, Snyderman CH, Gardner PA (2018) The limits of transsellar/transtuberculum surgery for craniopharyngioma. J Neurosurg Sci 62(3):301–309. https://doi.org/10.23736/S0390-5616.18.04376-X
Chakrabarti I, Amar AP, Couldwell W, Weiss MH (2005) Long-term neurological, visual, and endocrine outcomes following transnasal resection of craniopharyngioma. J Neurosurg 102(4):650–657. https://doi.org/10.3171/jns.2005.102.4.0650
Conger AR, Lucas J, Zada G, Schwartz TH, Cohen-Gadol AA (2014) Endoscopic extended transsphenoidal resection of craniopharyngiomas: nuances of neurosurgical technique. Neurosurg Focus 37(4):E10. https://doi.org/10.3171/2014.7.FOCUS14364
Elliott RE, Jane JA Jr, Wisoff JH (2011) Surgical management of craniopharyngiomas in children: meta-analysis and comparison of transcranial and transsphenoidal approaches. Neurosurgery 69(3):630–643; discussion 643. https://doi.org/10.1227/NEU.0b013e31821a872d
Tang B, Xie SH, Xiao LM, Huang GL, Wang ZG, Yang L, Yang XY, Xu S, Chen YY, Ji YQ, Zeng EM, Hong T (2018) A novel endoscopic classification for craniopharyngioma based on its origin. Sci Rep 8(1):10215. https://doi.org/10.1038/s41598-018-28282-4
Wang KC, Kim SK, Choe G, Chi JG, Cho BK (2002) Growth patterns of craniopharyngioma in children: role of the diaphragm sellae and its surgical implication. Surg Neurol 57(1):25–33. https://doi.org/10.1016/s0090-3019(01)00657-7
Steno J, Malacek M, Bizik I (2004) Tumor-third ventricular relationships in supradiaphragmatic craniopharyngiomas: correlation of morphological, magnetic resonance imaging, and operative findings. Neurosurgery 54(5):1051–1058; discussion 1058-1060. https://doi.org/10.1227/01.neu.0000120421.11171.61
Forbes JA, Ordonez-Rubiano EG, Tomasiewicz HC, Banu MA, Younus I, Dobri GA, Phillips CD, Kacker A, Cisse B, Anand VK, Schwartz TH (2018) Endonasal endoscopic transsphenoidal resection of intrinsic third ventricular craniopharyngioma: surgical results. J Neurosurg 131:1–11. https://doi.org/10.3171/2018.5.JNS18198
Hofmann BM, Hollig A, Strauss C, Buslei R, Buchfelder M, Fahlbusch R (2012) Results after treatment of craniopharyngiomas: further experiences with 73 patients since 1997. J Neurosurg 116(2):373–384. https://doi.org/10.3171/2011.6.JNS081451
Van Effenterre R, Boch AL (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg 97(1):3–11. https://doi.org/10.3171/jns.2002.97.1.0003
Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M (1999) Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg 90(2):237–250. https://doi.org/10.3171/jns.1999.90.2.0237
Duff J, Meyer FB, Ilstrup DM, Laws ER Jr, Schleck CD, Scheithauer BW (2000) Long-term outcomes for surgically resected craniopharyngiomas. Neurosurgery 46(2):291–302; discussion 302-295. https://doi.org/10.1097/00006123-200002000-00007
Turel MK, Tsermoulas G, Gonen L, Klironomos G, Almeida JP, Zadeh G, Gentili F (2016) Management and outcome of recurrent adult craniopharyngiomas: an analysis of 42 cases with long-term follow-up. Neurosurg Focus 41(6):E11. https://doi.org/10.3171/2016.9.FOCUS16315
Alalade AF, Ogando-Rivas E, Boatey J, Souweidane MM, Anand VK, Greenfield JP, Schwartz TH (2018) Suprasellar and recurrent pediatric craniopharyngiomas: expanding indications for the extended endoscopic transsphenoidal approach. J Neurosurg Pediatr 21(1):72–80. https://doi.org/10.3171/2017.7.PEDS17295
Acknowledgments
Thanks to Yang Zhongjin from Beijing Neurosurgical Institute for drawing the schematic diagrams of the subclassification of craniopharyngiomas for approach selection.
Funding
This study was supported by Beijing Municipal Science & Technology Commission (grant no. Z19110700660000) and the Capital’s Funds for Health Improvement and Research (2020-4-1077). The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This retrospective study was approved by the Ethics Committee of Beijing Tiantan Hospital, Capital Medical University (KYSQ 2019-287-01).
Informed consent
Informed consent was obtained from all adult participants or the parents of 2 minor participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
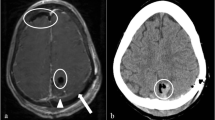
Supplemental Figure 1.
Pre- and post-operative MRI and intraoperative findings of intra-suprasellar craniopharyngiomas. Case 9 showed the space between the pituitary gland and the optic chiasm is enough to remove the tumor though EEA. EEA showed its advantage to remove the left-superior part under direct vision. Case 10 was a 4 years old boy, we did not choose EEA because the huge tumor extends extremely to lateral side, the poorly pneumatized sinuses, smaller facial structure and the difficulty for skull base reconstruction. The tumor was totally removed via the lateral subfrontal approach. Case 11, for this patient, we chose lateral subfrontal approach rather than EEA because the tumor extends extremely ahead and it was difficult to see the front interface of the tumor through EEA. OC= optic chiasm; PS= pituitary stalk; ON= optic nerve; T= tumor; P= pituitary; ICA= internal carotid artery; MCA= middle cerebral artery; ACA= anterior cerebral artery; LT= lamina terminalis. (PNG 3889 kb)
Supplemental Figure 2.
Pre- and post-operative MRI and intraoperative findings of suprasellar craniopharyngiomas. Case 12, the tumor extended into the 3rd ventricle. Removing the tumor through EEA with two corridors: infra-chiasm and supra- chiasm (translamina terminalis). After the tumor was removed via EEA, the posterior wall of third ventricle, Monro foramen, and upper outlet of aqueduct can be seen clearly. Case 13, the tumor was cystic. After the tumor was removed through infra-chiasm corridor via EEA approach, the posterior wall of third ventricle, Monro foramen, and upper outlet of aqueduct could be seen clearly. Case 14, we chose lateral subfrontal approach because the tumor mainly located behind the saddle, which leading to the corridor between the chiasm and the pituitary gland to be narrow and long to remove the tumors located in the retrochiasmatic space through EEA. During the operation, the tumor could not be seen through prechiasmatic space and the lamina terminalis was obstructed by the anterior communicating artery. There were three blind spots for this approach: the undersurface of the optic chiasm and optic nerves, intrasellar and interface between tumor and hypothalamus. Case 15, the tumor mainly located behind the saddle and was severe calcified. The calcification could be resected en bloc through lamina terminalis for it was too hard to resect it piece by piece. Post-operatively, the girl had a temporary bilateral oculomotor nerve palsy and blurred vision in both eyes because of retraction-related injury of the optic apparatus and oculomotor nerve, which was recovered in two weeks. Case 16, we used left pterional approach because the tumor extended outside the carotid bifurcation. Case 17, we chose lateral subfrontal approach because the tumor extended to the retro-clival area. OC= optic chiasm; PS= pituitary stalk; ON= optic nerve; T= tumor; CT= calcified tumor; P= pituitary; ICA= internal carotid artery; 3rd V. = 3rd ventricle; LT= lamina terminalis; HT, hypothalamus; MF, Monro’s foramen. (PNG 8021 kb)
ESM 3
(AVI 485440 kb)
Rights and permissions
About this article
Cite this article
Lei, C., Chuzhong, L., Chunhui, L. et al. Approach selection and outcomes of craniopharyngioma resection: a single-institute study. Neurosurg Rev 44, 1737–1746 (2021). https://doi.org/10.1007/s10143-020-01370-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01370-8