Abstract
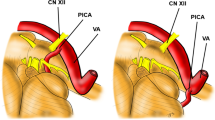
Bilateral complex vertebral artery aneurysms (BCoVAAns) have no established strategy of management. We retrospectively reviewed five consecutive patients with unruptured BCoVAAns between January 2006 and December 2012. Considering surgical risks of lower cranial nerve (LCN) injuries and eventual growth of an opposite side lesion after unilateral vertebral artery (VA) occlusion, we proposed a strategy of combined open and interventional treatment using revascularization. We applied the following several specific techniques: (1) proximal clipping and occipital artery-posterior inferior cerebellar artery (OA-PICA) and/or superficial temporary artery (STA)-superior cerebellar artery (SCA) bypasses; (2) Distal blood pressure, motor evoked potentials (MEPs), and somatosensory evoked potentials (SEPs) monitoring after parent artery temporary occlusion for safe permanent occlusion of the proximal portions of VA and PICA; (3) V3 to V4 bypass using radial artery (RA) graft with proximal clipping or trapping, two of them combined with OA-PICA bypass; (4) VA fenestration as an opportunity to preserve the flow of the parent artery. Two patients were treated bilaterally and 3 unilaterally, with modified Rankin scale assessed at 39 months postoperatively in average 0 in 2, 1 in 2, and 2 in 1, respectively, and the untreated opposite side lesions without regrowth or bleeding. Two patients with patent V3-RA-V4 bypass complained of dysphagia due to LCN palsies. One of them however suffered a cerebellar infarction due to occlusion of the OA-PICA bypass. When BCoVAAns require surgical treatment, revascularization or preservation of the VA should be considered at the first operation. By doing so, the opposite aneurysm can be effectively occluded by coil embolization, even with VA sacrifice if required.








Similar content being viewed by others
References
Anson JA, Lawton MT, Spetzler RF (1996) Characteristics and surgical treatment of dolichoectatic and fusiform aneurysms. J Neurosurg 84:185–193
Fiorella D, Hsu D, Woo HH, Tarr RW, Nelson PK (2010) Very late thrombosis of a pipeline embolization device construct: case report. Neurosurgery 67:onsE313–4
Fiorella D, Kelly ME, Albuquerque FC, Nelson PK (2009) Curative reconstruction of a giant midbasilar trunk aneurysm with the pipeline embolization device. Neurosurgery 64(2):212–217
Katsuno M, Mizunari T, Kobayashi S, Takahashi H, Teramoto A (2009) Rupture of a vertebral artery dissecting aneurysm developing immediately after trapping of a dissecting aneurysm on the contralateral vertebral artery: case report. Neurol Med Chir (Tokyo) 49:468–470
Kitanaka C, Tanaka J, Kuwahara M, Teraoka A, Sasaki T, Takakura K, Tanaki J (1994) Nonsurgical treatment of unruptured intracranial vertebral artery dissection with serial follow-up angiography. J Neurosurg 80:667–674
Klisch J, Turk A, Turner R, Woo HH, Fiorella D (2011) Very late thrombosis of flow diverting constructs after the treatment of large fusiform posterior circulation aneurysms. AJNR Am J Neuroradiol 32:627–632
Kobayashi N, Murayama Y, Yuki I, Ishibashi T, Ebara M, Arakawa H, Irie K, Takao H, Kajiwara I, Nishimura K, Karagiozov K, Urashima M (2014) Natural course of dissecting vertebrobasilar artery aneurysms without stroke. AJNR Am J Neuroradiol 35:1371–1375, Originally published online on March 7, 2014, 10.3174/ajnr.A3873
Kubo Y, Miura K, Suzuki M, Tsuiki K, Kuwata N, Kubo N, Kuroda K, Ogawa A (1998) Development of a dissecting aneurysm on the vertebral artery immediately after occlusion of the contralateral vertebral artery: a case report. Neurosurg Rev 21:177–180
Kubota H, Tanikawa R, Katsuno M, Noda K, Ota N, Miyata S, Yabuuchi T, Izumi N, Bulsara KR, Hashimoto M (2013) Reconstruction of intracranial vertebral artery with radial artery and occipital artery grafts for fusiform intracranial vertebral aneurysm not amenable to endovascular treatment: technical note. Acta Neurochir (Wien) 155(8):1517–24, Discussion 1524
Mizutani T (1996) A fatal, chronically growing basilar artery: a new type of dissecting aneurysm. J Neurosurg 84:962–971
Mizutani T, Miki Y, Kojima H, Suzuki H (1999) Proposed classification of nonatherosclerotic cerebral fusiform and dissecting aneurysms. Neurosurgery 45:253–260
Ohta T, Fujimoto K, Takahashi J (2010) Natural history of asymptomatic non-thrombosed fusiform aneurysm of vertebral artery: a study of 10 cases. Surg Cereb Stroke (Jpn) 38:137–141
Saito N, Kamiyama H, Takizawa K, Takebayashi S, Asano T, Kobayashi T, Kobayashi R, Kubota S, Ito Y (2014) Usefulness of V3-Radial Artery-V4 Bypass in Bilateral Fusiform Aneurysms of Vertebral Artery. Neurol Med Chir (Tokyo) 54(3):189–91
Saito N, Kamiyama H, Takizawa K, Takebayashi S, Kobayashi T, Shimizu T, Kubota S, Maruichi K (2013) Strategy for treatment of unruptured thrombosed large vertebral artery aneurysm. Surg Cereb Stroke (Jpn) 41:27–32
Sanada Y, Ohmori K, Yabuuchi T, Nakagawa N, Nunokawa T, Iwakura T, Kato A (2012) Surgical strategy for bilateral large vertebral dissecting aneurysms: lessons from a case. Surg Cereb Stroke (Jpn) 40:35–40
Siddiqui AH, Alba AA, Kan P, Dumont TM, Jahshan S, Britz GW, Hopkins LN, Levy EI (2012) Panacea or problem: flow diverters in the treatment of symptomatic large or giant fusiform vertebrobasilar aneurysms. J Neurosurg 116(6):1258–1266
Spektor S, Anderson GJ, McMenomey SO, Horgan MA, Kellogg JX, Delashaw JB Jr (2000) Quantitative description of the far-lateral transcondylar transtubercular approach to the foramen magnum and clivus. J Neurosurg 92:824–831
Tanikawa R, Sugimura T, Hino K, Izumi N, Mitsui N, Yamaguchi T, Hashimoto M, Hashizume A, Fujita T (2006) Surgical application of skull base technique for EC-IC bypass to P2 segment. Surg Cereb Stroke (Jpn) 34:440–444
Vishteh AG, Spetzler RF (1999) Evolution of a dolichoectatic aneurysm into a giant serpentine aneurysm during long-term follow up. Case illustration. J Neurosurg 91:346
Yasui T, Komiyama M, Iwai T, Yamanaka K, Nishikawa M, Morikawa T (1998) Evolution of incidentally-discovered fusiform aneurysms of the vertebrobasilar arterial system: neuroimaging features suggesting progressive aneurysm growth. Neurol Med Chir (Tokyo) 41:523–528
Yasui T, Sakamoto H, Kishi H, Komiyama M, Nishikawa M, Iwai Y, Yamanaka K, Nakajima H, Kishi H, Kan M, Fujitani K, Hakuba A (1998) Bilateral dissecting aneurysms of the vertebral arteries resulting in subarachnoid hemorrhage: case report. Neurosurgery 42:162–165
Yoshimoto Y, Wakai S (1997) Unruptured intracranial vertebral artery dissection. Clinical course and serial radiographic imagings. Stroke 28:370–374
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Comments
Takeshi Mikami, Sapporo, Japan
In this report, the authors present a series of patients with bilateral complex vertebral artery (VA) aneurysms that were treated using bypass surgery. The introduction of vascular reconstruction for the treatment of complex aneurysms of the anterior circulation was associated with improved outcomes. This is a valuable article in that it points the way toward the development of a strategy in which vascular reconstruction is used for the treatment of complex aneurysms of the posterior circulation. Another advantage of this report is that it allows for the preservation of the orthodromic basilar flow. The clear schematic illustration provided in this article is useful and enables a better understanding of the reconstruction methods.
One issue that detracts from the usefulness of this paper is that it often discusses various types of aneurysms (e.g., fusiform, thrombosed, calcified, dissecting) together, as if they were all equivalent, though the surgical requirements for the different types of aneurysms in this series are different. Also, in this series, there is no case of subarachnoid hemorrhage. Both fusiform aneurysm and dissecting aneurysm without subarachnoid hemorrhage are benign outcomes in the natural disease course; for these types of aneurysms, extended treatment is of minimal significance. Nevertheless, the morbidity of this case series is relatively high. Neurosurgeons should strive to preserve a balance between allowing the disease to run its natural course and pursuing surgical intervention, given the inevitable risks associated with the latter. In choosing a surgical strategy, the most important decision is which VA should be subjected to the revascularization procedure. In considering this, the positions of the perforating artery and the posterior inferior cerebellar artery as well as VA dominancy should be assessed thoroughly. Although the balloon occlusion test for the posterior circulation is questionable, it is useful in determining the safest possible position for a VA occlusion. Surgical results might be improved further if morphologic deflection of the VA was assessed and considered as well, as the dominant VA often has some morphologic deflection, and revascularization surgery should be performed in the nearer VA.
Overall, I think that this report is helpful, and I expect to see continued development of this technique for the treatment of bilateral complex VA aneurysms.
Brian P. Walcott and Michael T. Lawton, San Francisco, USA
Increasingly, the management of intracranial aneurysms is trending toward endovascular techniques, particularly in the posterior circulation. The International Subarachnoid Aneurysm Trial and the Barrow Ruptured Aneurysm Trial provide evidence supporting this trend for posterior circulation aneurysms, but say nothing about optimal treatment strategies for complex vertebral artery (VA) aneurysms that include dissecting, fusiform, and thrombosed aneurysms. The best management of these lesions remains unclear. New technologies such as flow-diverting stents have been used but are associated with significant morbidity and mortality due to compromise of vertebrobasilar perforators. In this case series from Saito et al., a combined open and endovascular management strategy that uses revascularization for bilateral complex vertebral artery aneurysms was applied in five patients. Overall, their approach was to trap the aneurysm or occlude the proximal vertebral artery, after first performing a bypass to maintain blood flow in the posterior inferior cerebellar artery and/or distal vertebrobasilar circulation. Contralateral lesions were observed in three of the five cases without untoward events. The technical expertise exhibited by the authors is impressive, and the results are generally excellent considering the complexity of these aneurysms.
These results set a very high standard for the management of vertebral artery aneurysms. There are few bypass surgeons with the requisite expertise to perform challenging bypasses like the V3 to V4 vertebral artery bypass with interposition graft. Nonetheless, this report demonstrates that this strategy works and argues convincingly for an aggressive surgical posture in the management of these lesions. It is important to distinguish the VA aneurysm from the basilar trunk aneurysm. Although they are proximate neighbors, the later is a more formidable lesion due to the presence of numerous pontine and midbrain perforators. Results with these basilar trunk lesions and a similar strategy of bypass and proximal occlusion are not nearly as favorable as those with VA aneurysms, and an aggressive surgical posture cannot be recommended. While these basilar trunk aneurysms remain an unsolved problem, VA aneurysms can be viewed as a rare relative with more permissive perforators and a more favorable risk profile that can and should be managed with bypass surgery at the heart of the management strategy.
Rights and permissions
About this article
Cite this article
Saito, N., Kamiyama, H., Takizawa, K. et al. Management strategy for bilateral complex vertebral artery aneurysms. Neurosurg Rev 39, 289–296 (2016). https://doi.org/10.1007/s10143-015-0686-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-015-0686-3